No CrossRef data available.
Article contents
Mechanical and Physical Behavior of Fibrin Clot Formation and Lysis in Combined Oral Contraceptive Users
Published online by Cambridge University Press: 11 August 2020
Abstract
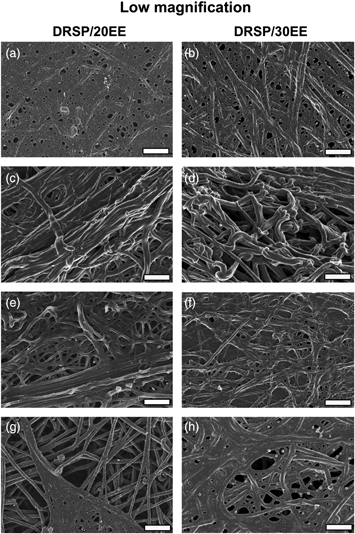
Combined oral contraceptives (COCs) are commonly prescribed and increase the risk of venous thromboembolism (VTE). We have previously found that two COCs, both containing drospirenone (DRSP) and ethinyl estradiol (EE), cause spontaneous fibrin formation in whole blood. The aim of this study was, therefore, to use platelet-poor plasma (PPP) from the same cohort of DRSP/EE users to determine the impact of these COCs on the fibrin component, specifically the fibrin clot viscoelasticity, turbidimetry, and biophysical traits. PPP from 25 females per test group and a control group (n = 25) were analyzed using thromboelastography (TEG), turbidimetry, and scanning electron microscopy. The results highlight abnormal fibrin clot formation, lysis, and architecture; DRSP/20EE showed the greatest effect. DRSP/EE use increased the fibrin fiber diameter and showed dense matted clots. Only when the influence of COCs on the structural properties and behavior of fibrin fibers during thrombus formation and lysis is better understood are we able to predict and prevent coagulopathies associated with these synthetic hormones. Clinical practitioners should take this into consideration for female patients that either have comorbidities, which could burden the coagulation system, or may be exposed to external factors that could increase their risk for VTE.
Keywords
- Type
- Biological Applications
- Information
- Copyright
- Copyright © Microscopy Society of America 2020





