Introduction
Perinatal depression (PND) refers to depressive episodes that occur during pregnancy or after delivery. Affecting approximately 18% of all pregnancies worldwide (Gavin et al., Reference Gavin, Gaynes, Lohr, Meltzer-Brody, Gartlehner and Swinson2005), this disorder is associated with many poor outcomes for women's maternal and physical health and the emotional and cognitive development of infants and children during their sensitive growth periods (Beardslee et al., Reference Beardslee, Versage and Gladstone1998; Muzik and Borovska, Reference Muzik and Borovska2010; Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011). The early identification and timely intervention could improve the prognosis of PND means that in many countries screening for PND is incorporated as part of the routine perinatal care (Buist et al., Reference Buist, Austin, Hayes, Speelman, Bilszta, Gemmill, Brooks, Ellwood and Milgrom2008; Earls et al., Reference Earls2010; Milgrom and Gemmill, Reference Milgrom and Gemmill2014; O'Connor et al., Reference O'Connor, Rossom, Henninger, Groom, Burda, Henderson, Bigler and Whitlock2016; Urato, Reference Urato2017; ACOG, 2018). For screening to work, however, identification of women with positive screening results needs to be followed by timely intervention after referral. In this review, referral was defined as the process of recommending women to receive further mental health care after screening. The process of referral could be divided into three steps. First, the providers make the referral for women with positive screening results (step 1). Then, women accept the referral and try to access mental health services (step 2: ‘uptake’). Finally, relevant resources must be available to provide the necessary support (step 3). Steps 1 and 3 are both responsibilities of the healthcare system and routine screening should only be carried out if the prerequisites of these two are met. This review, therefore, focuses on step 2, namely uptake by women with positive screening results after being offered referrals. Low uptake rates reduce the overall effectiveness of screening. If a woman does not take up the offer of referral after the positive screening, the basis of introducing universal screening is weakened (Hewitt and Gilbody, Reference Hewitt and Gilbody2009; Thombs et al., Reference Thombs, Arthurs, Coronado-Montoya, Roseman, Delisle, Leavens, Levis, Azoulay, Smith, Ciofani, Coyne, Freeley, Gilbody, Schinazi, Stewart and Zelkowitz2014).
Previous studies investigating the uptake of referrals after screening have reported that the uptake rates varied very widely (0% to 94%) (Tam et al., Reference Tam, Newton, Dern and Parry2002; Miller et al., Reference Miller, Shade and Vasireddy2009). Uptake of referral after depression screening is a complex process. There are barriers related to patients and healthcare providers. These needed to be addressed in order to increase the uptake rate. A systematic review of uptake would help to inform the debate on the case for screening in those countries where screening is not yet routinely performed. In those where screening is already taking place, understanding the reasons behind low uptake rates and what interventions would increase these rates would be useful to improve the effectiveness of screening.
In this paper, we presented a systematic review that included studies reporting uptake rates after screening for PND and a meta-analysis on the overall uptake rate. We also explored the relationship between the type of referral interventions after administering the screening test and uptake. In addition, we summarised the reasons behind the lack of engagement with mental health care after referral. In contrast to related reviews (Byatt et al., Reference Byatt, Levin, Ziedonis, Moore-Simas and Allison2015; Long et al., Reference Long, Cramer, Jenkins, Bennington and Paulson2019), we have specifically focused on uptake of referral (step 2) for reasons stated above.
Methods
Literature review
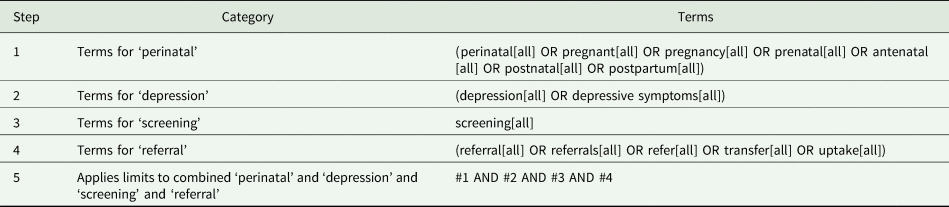
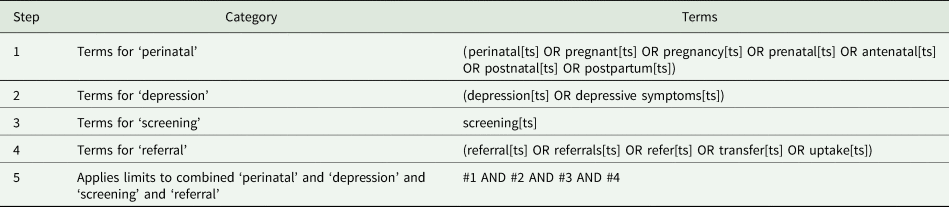
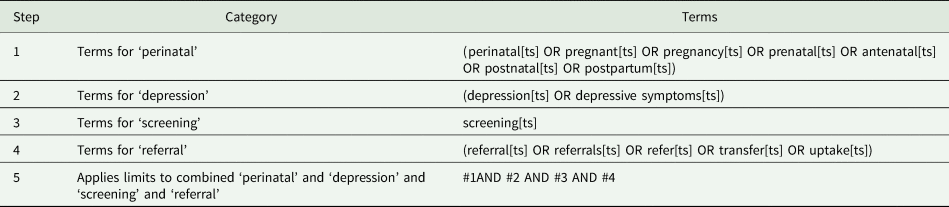
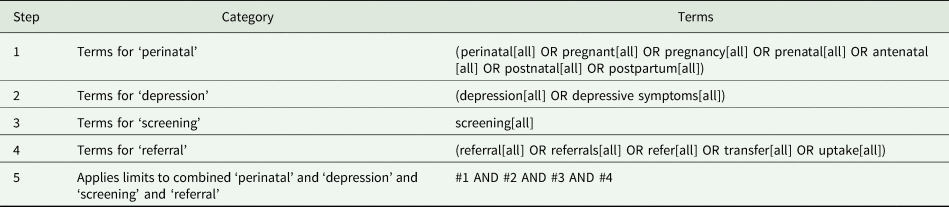
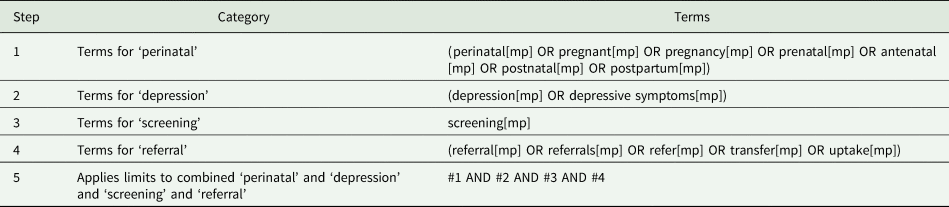
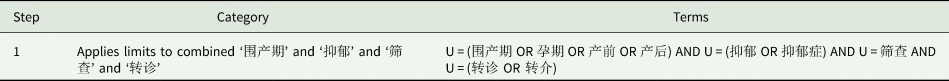
This systematic review and meta-analysis was undertaken according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The protocol was registered in the PROSPERO database, number CRD42019138095. One of us who has experiences in women's mental health (WG) developed the search strategy and the full search strategy is available in Appendix A. In brief, we searched Pubmed, Web of Science, Cochrane Library, Ovid, Embase, CNKI, Wanfang Database and VIP Database for studies in English or Chinese from the inception of the database until January 13, 2019. In English database, we used the search terms (‘perinatal’, ‘pregnant’, ‘pregnancy’, ‘prenatal’, ‘antenatal’, ‘postnatal’ OR ‘postpartum’) AND (‘depression’ OR ‘depressive symptoms’) AND ‘screening’ AND (‘referral’, ‘referrals’, ‘refer’, ‘transfer’ OR ‘uptake’). We used the search terms (‘围产期’, ‘孕期’, ‘产前’ OR ‘产后’) AND (‘抑郁’ OR ‘抑郁症’) AND ‘筛查’ AND (‘转诊’ OR ‘转介’) in Chinese database.
Inclusion and exclusion
After removing duplications, we reviewed each title and abstract based on inclusion and exclusion criteria. Inclusion criteria were: (1) language limited to English and Chinese; (2) participants were pregnant or postpartum (within 2 years of delivery) women who were screened positive for PND by any validated screening tool; (3) reported uptake rates (the number of women who accept the referral and try to access mental health service among women who were offered referral); (4) if there were interventions other than the administering of the screening test, the objective or one of the objectives of the interventions was to improve referral status. Exclusion criteria were: (1) no detail of referral process or exact data of uptake of referral were reported; (2) case report or case series. Then full-text articles were retrieved to determine eligibility criteria. Finally, references of retrieved full-text articles were screened for additional eligible publications. Investigators (WX and LL/QL/JW/PY/XM) independently assessed each study for inclusion. Disagreements were resolved through discussion with each other or consulting a third one (WG). When the full-text was not available (e.g. only the abstract was available), we would contact the author by email and if no reply was received within a month, the article would be excluded.
Extraction
The following study-level characteristics were independently extracted (WX and LL/QL/JW/PY/XM) and disagreements were resolved via discussion or consulting a third one (WG): first author, publication year, study type, study country (countries are classified by income level according to World Bank Country and Lending Groups) (The World Bank Group, 2016), screening tool, sample size (number of women who were screened positive and were offered referral), time points of screening (prenatal, postnatal or perinatal), year of study, referral methods (referral to mental health services or on-site assessment or treatment), referral interventions, uptake of referral (number of women who accepted referrals and tried to access mental health service), referral uptake rates, the reasons for non-uptake and patient outcomes.
Quality assessment
We used the Loney criteria to assess the quality of observational studies and quasi-experimental studies, and used Cochrane Risk of Bias Tool (ROS) to assess the quality of randomised controlled trials (RCTs) (Loney et al., Reference Loney, Chambers, Bennett, Roberts and Stratford1998; Higgins et al., Reference Higgins, Altman, Gotzsche, Juni, Moher, Oxman, Savovic, Schulz, Weeks and Sterne2011). The Loney criteria included eight items on the risk of bias from three aspects: A. Validity of the study methods: (1) The study design and sampling method are appropriate for the research question. (2) The sampling frame is appropriate. (3) The sample size is adequate. (4) Objective, suitable and standard criteria are used for the measurement of the health outcome. (5) The health outcome is measured in an unbiased fashion. (6) The response rate is adequate and the refusers are described. B. Interpretation of the results: (7) The estimates of prevalence and incidence are given with confidence intervals and in detail by subgroup, if appropriate. C. Applicability of the findings: (8) The study subjects and the setting are described in detail. The maximal total score is eight points, with higher scores suggesting a lower risk of bias. ROS helps to evaluate the risk of bias from six aspects: selection bias, performance bias, detection bias, attrition bias, reporting bias and others. Each item was determined as ‘high risk of bias’, ‘low risk of bias’, ‘unclear risk of bias’. Assessment of bias was performed by two authors (WX and XJ) and disagreements were reconciled through discussion.
Data analysis
In our review, prospective or retrospective studies that did not assign women to intervention or control groups at the referral stage were considered observational studies. Before and after comparison studies which examined the difference before and after the referral intervention took place were regarded as quasi-experimental studies. Studies that randomly allocated women to a referral intervention group or no intervention group, or to a high-intensive referral intervention group or low-intensive referral intervention group were categorised as RCT. The data provided by observational studies and quasi-experimental studies were used to estimate the pooled rate of uptake. RCT was used to evaluate the effect of interventions.
The ‘meta’ module in R-3.5.1 statistical software package was used for the calculation of the pooled rate of uptake. First, the uptake rates reported in each study were transformed using the Freeman-Tukey Double arcsine method according to the distribution of rates (Freeman and Turkey, Reference Freeman and Turkey1950; Luo et al., Reference Luo, Tan, Zhou, Wang, Chang, Guo and Shen2013). Then we calculated the pooled rate and 95% confidence intervals (CIs) in a meta-analysis. Heterogeneity was assessed using Cochran's Q test, and quantified by the I2 value and tau2. If the heterogeneity results showed that p ⩽ 0.10 or I 2 > 50% and suggested high heterogeneity, the random-effect model would be adopted. Otherwise, the fixed-effect model would be applied. Publication bias was evaluated by presenting a funnel plot and performing Egger's linear test. Sensitivity analysis was performed by serially removing studies one by one to explore the impact of doing so on the overall uptake rate. Any study for which removal substantially changed the uptake rate would be noted. Multivariate meta-regression was conducted to explore the source of heterogeneity and then the odds ratios (OR) were calculated through a formula: OR = exp(β) (β: regression coefficient). Through literature review, study country, time points of screening, referral methods and referral interventions were identified as predictor variables (Smith et al., Reference Smith, Shao, Howell, Wang, Poschman and Yonkers2009; Byatt et al., Reference Byatt, Levin, Ziedonis, Moore-Simas and Allison2015; Gajaria and Ravindran, Reference Gajaria and Ravindran2018; Savovic et al., Reference Savovic, Turner, Mawdsley, Jones, Beynon, Higgins and Sterne2018). Subgroup analyses were performed to estimate the pooled uptake rate with regard to the significant factors in meta-regression analyses and the differences between subgroups were investigated through chi-squared test (the significance level was p < 0.05).
There were insufficient numbers of RCTs to allow for meta-analysis. Therefore, we conducted a descriptive analysis based on the uptake rates provided by the RCT in SPSS 18.0 to show the effectiveness of interventions.
Results
Search results
The systematic literature search yielded 2302 articles, including 2296 English articles and six Chinese articles (Fig. 1). After removing duplicates, a total of 1818 references were identified. Of the 1818 reviewed, 1681 were eliminated after title/abstract review and 105 were eliminated after full-text reviews because they did not meet inclusion criteria (The main reasons for exclusion are shown in Fig. 1.) This resulted in 32 studies for inclusion. After additional searches, a further nine studies were included from reference lists of included papers. In total, 41 articles were included in this review, including one RCT, one before and after comparison study, and 39 observational studies.
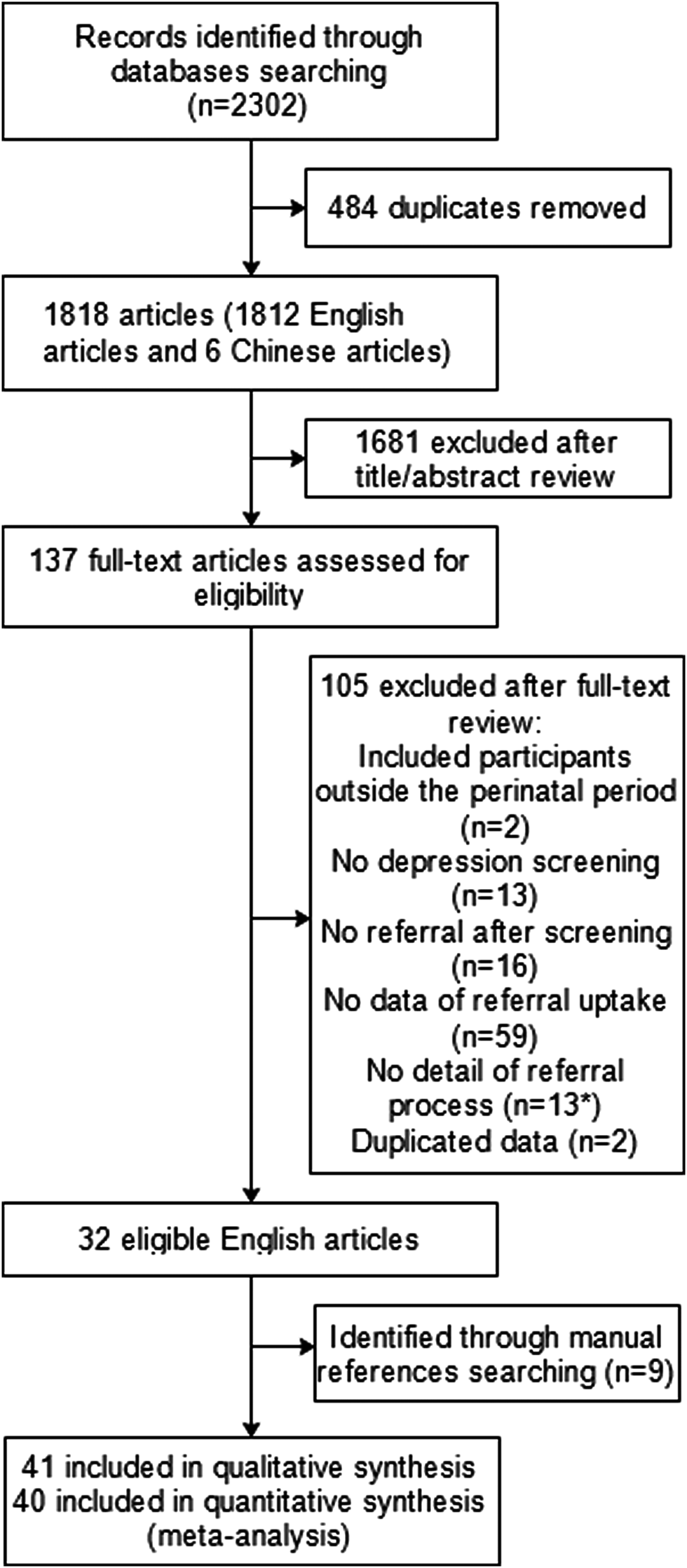
Fig. 1. Article selection process. *Three articles were excluded because we did not get reply within 1 month after we contacted the authors by email.
Quality assessment
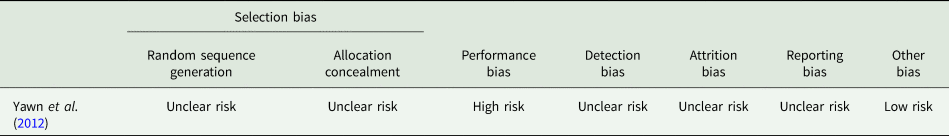
Consensus was reached in over 90% among the two independent authors (WX and XJ) in quality assessment. In 40 observational or quasi-experimental studies, 12 of the 40 eligible studies scored five points, 15 scored four points, 11 scored three points and two scored two points based on the Loney criteria. For the validity of the study methods, 62% of studies (n = 25) used a biased sampling method, 95% of the studies (n = 38) did not apply an appropriate sampling frame, 72% (n = 29) had an insufficient sample size and 72% (n = 29) had low response rates or did not describe refusers. None provided confidence intervals. Three studies did not report the characteristics of study subjects. Result of the quality assessment of the RCT is shown in Appendix B. The RCT had ‘high risk’ in performance bias which meant it did not blind the randomisation status to participants or personnel.
Study characteristics
Table 1 shows the characteristics of the eligible studies. Forty studies were observational or quasi-experimental studies with 9380 women who were screen positive. One was RCT with 555 women who were screen positive. Two-thirds of the 41 studies (n = 27) were carried out in the USA. The rest were conducted in Australia (n = 6), Iceland (n = 2) and there was one study each from Turkey, Singapore, New Zealand, China, Republic of South Africa and Israel. The sample size ranged from 5 to 1751 participants. Mean sample ages of women ranged from 23.4 to 35.7 years.
Table 1. Characteristics of studies included in this review
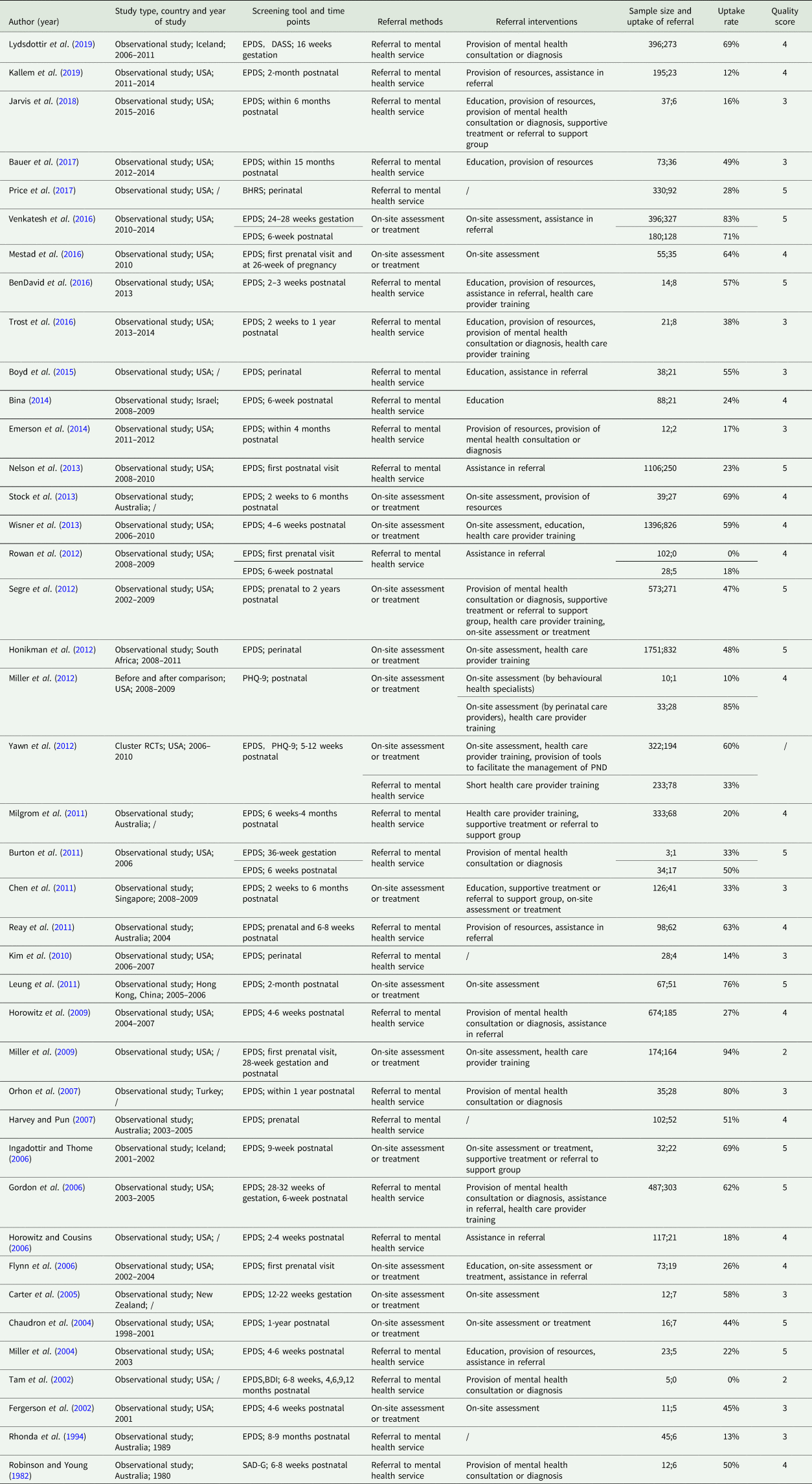
Most studies (n = 38, 93%) used the Edinburgh Postnatal Depression Scale (EPDS) as the screening tool (Cox et al., Reference Cox, Holden and Sagovsky1987). The remaining used Patient Health Questionnaire (PHQ-9) (n = 2) (Wittkampf et al., Reference Wittkampf, Naeije, Schene, Huyser and van Weert2007), Beck Depression Inventory (BDI) (n = 1) (Beck et al., Reference Beck, Ward, Mendelson, Mock and Erbaugh1961), Behavioural Health Risk Screen (BHRS) (n = 1) (Price et al., Reference Price, Corder-Mabe and Austin2012), self-assessment of Depression, General Scale (SAD-G) (n = 1) (Snaith et al., Reference Snaith, Bridge and Hamilton1976) and Depression Anxiety Stress Scales (DASS) (n = 1) (Lovibond and Lovibond, Reference Lovibond and Lovibond1995). Time points of screening ranged from first antenatal checks to 2 years after delivery, which was broadly in line with the timing of prenatal/postnatal appointments or well-baby visits. Main screening sites were healthcare facilities, including obstetrics, paediatrics or neonatal intensive care units. After identifying women who were screened positive, programme members or health care providers who performed screening, including obstetricians, nurses, or midwives, would recommend referral. Some studies conducted remote screening through mail or telephone. The majority of studies referred women with positive screening results to mental health service for further mental health assessment or treatment. Providers of mental health services included mental health professionals (e.g. psychologists, psychiatrists), perinatal care providers (e.g. obstetricians, midwives), primary care providers (e.g. general practitioner) and behavioural health specialists. Some studies provided on-site assessment or treatment, which were mainly performed in the clinic by program members, social workers, or health care providers who conducted the screening. When women who were screened positive attended mental health department/clinic to undergo further assessment/treatment or received on-site assessment/treatment provided by studies, it constituted as uptake of referral in this review. In prospective studies, the outcomes of referral were mostly determined through follow-up by telephone. Of the prospective studies, 12 provided the length of follow-up which ranged from 2 weeks to 6 months. In retrospective studies, the outcomes of referral were always determined by reviewing the medical records.
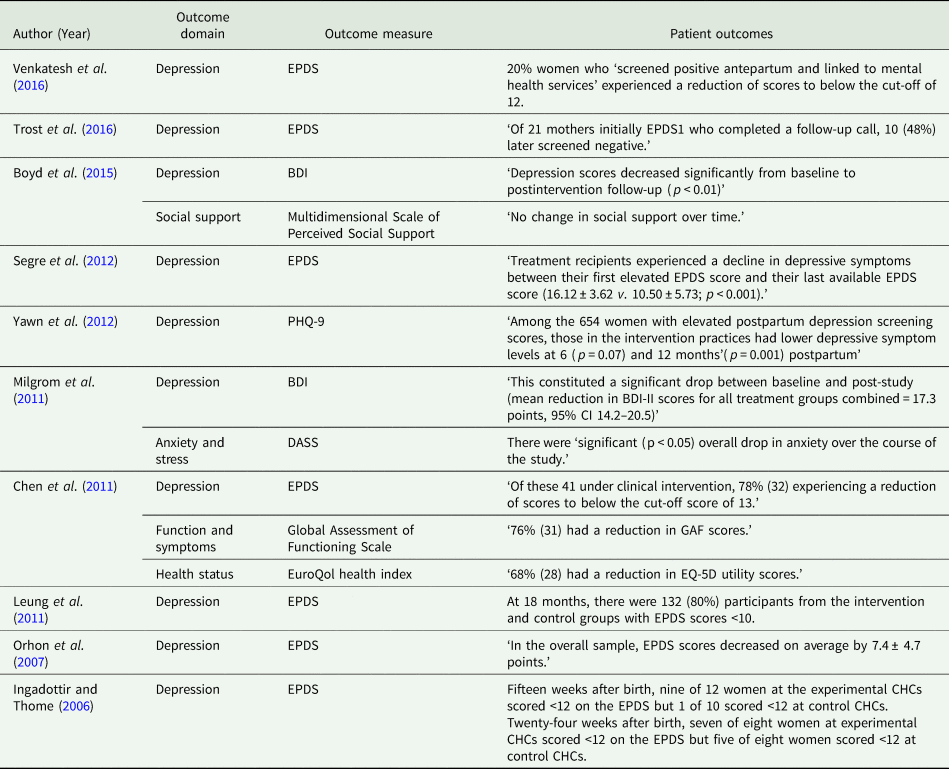
Out of the 41 studies included in this review, 10 of them reported patient outcomes related to their depression (Appendix C). All ten studies showed improvement among patients who received further specialist support after referral.
Pooled referral uptake rate
In 40 observational or quasi-experimental studies, three provided referral data of both prenatal and postnatal periods, one provided data of pre-intervention and post-intervention. Therefore, we had a total of 44 referral rates from 40 observational or quasi-experimental studies for the following analysis. The rates of referral uptake in different countries varied widely as Table 1 shows.
Figure 2 shows the uptake rates of all included observational or quasi-experimental studies and the pooled rate. Significant heterogeneity (I 2 = 97.7%, τ 2 = 0.0537, p < 0.01) was observed across the included studies. The pooled uptake rate was 43% (95% CI 35–50%), using the random effect model.
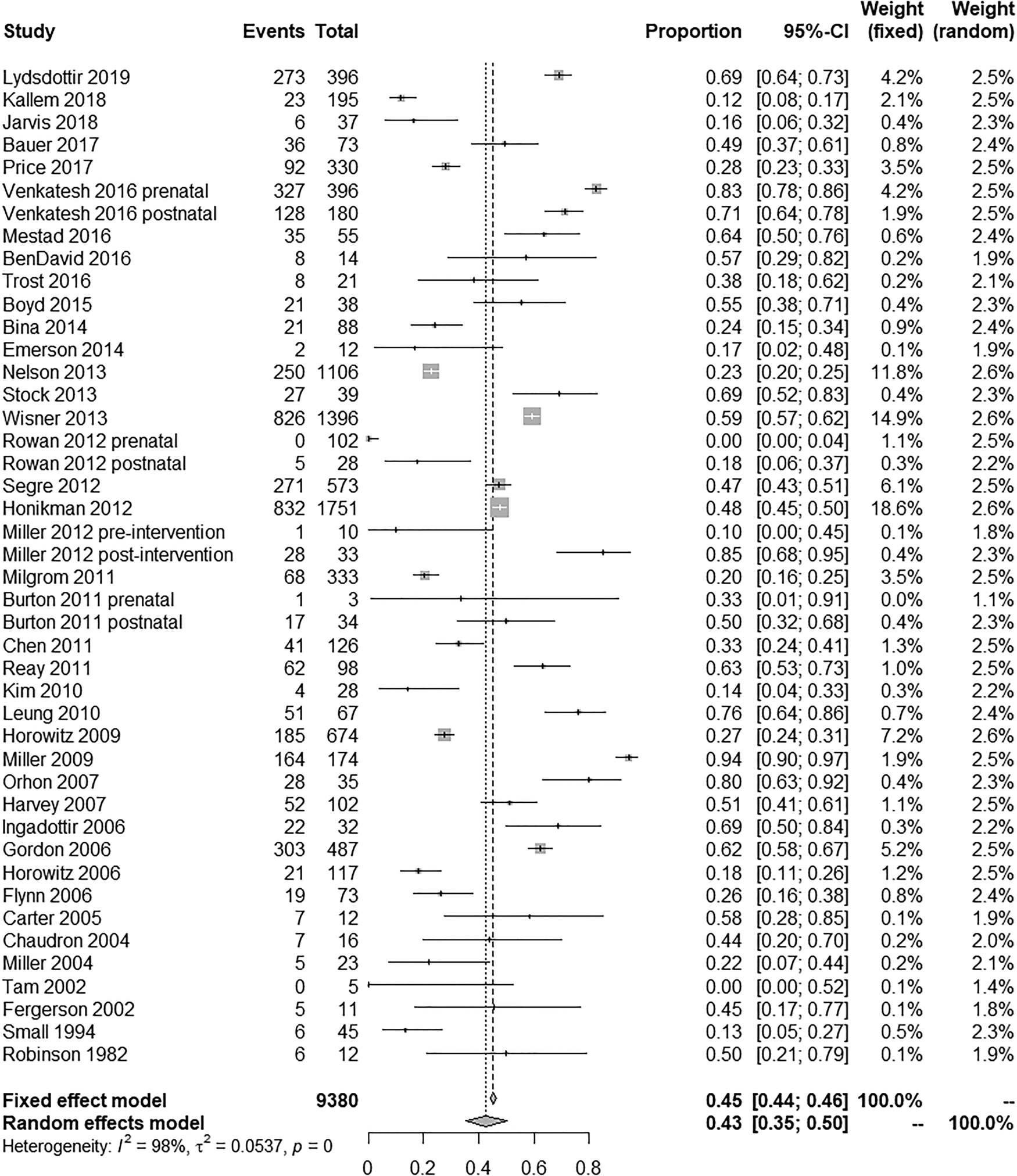
Fig. 2. Forest plot of the results of the meta-analysis of referral uptake rates in included studies.
Publication bias and sensitivity analysis
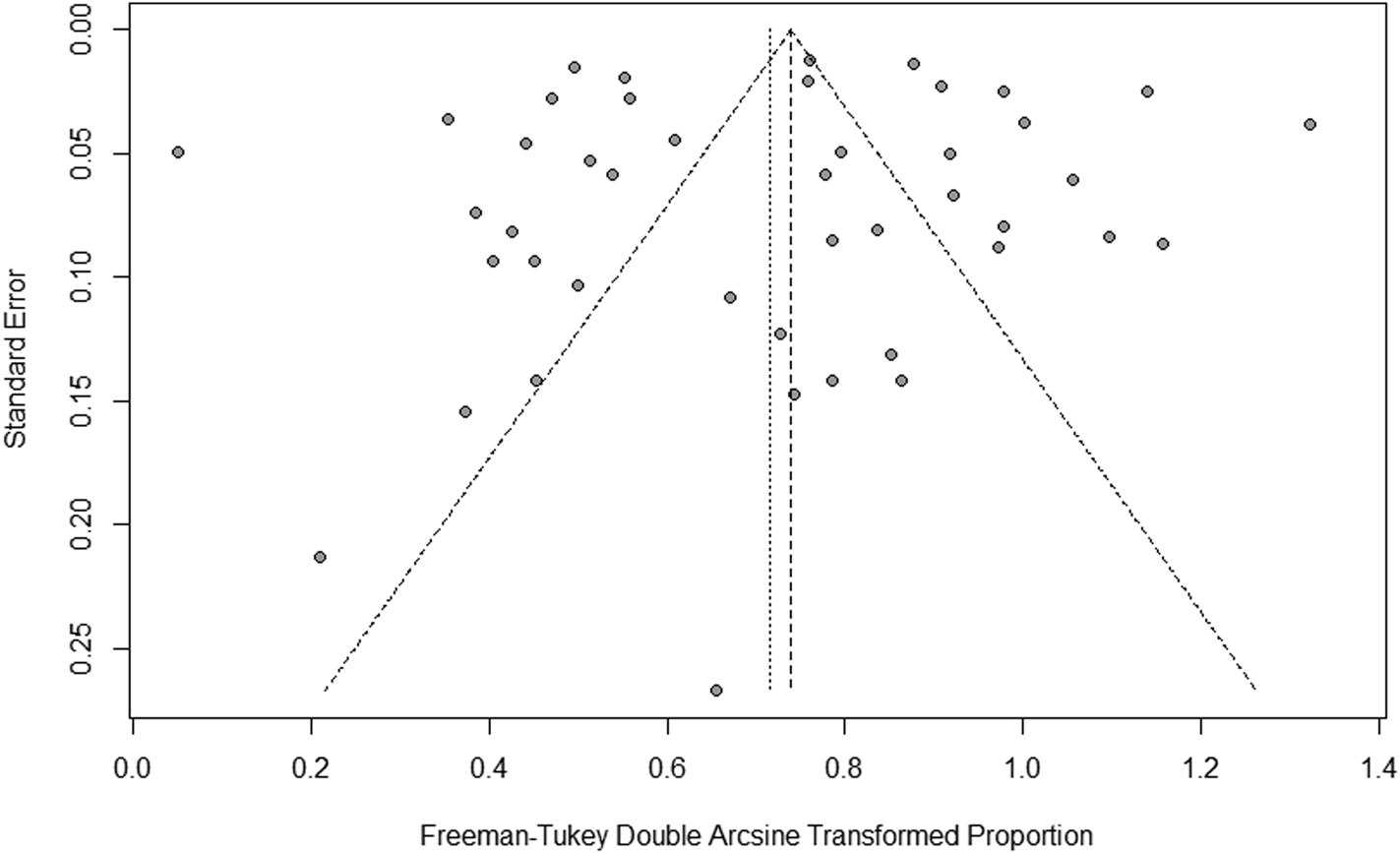
The funnel plot was almost symmetrical suggesting that publication bias was likely to be small (see Appendix D). This was consistent with the result of the Egger's test (t = −0.32, p = 0.75).
Sensitivity analysis was performed through serially removing studies one by one. The I2 values ranged from 97.3% to 97.8%, the tau2 ranged from 0.0477 to 0.0655 and the combined referral rate ranged from 41% (95% CI 34–48%) to 44% (95% CI 37–52%), indicating that the results of the meta-analysis were reliable.
Meta-regression analysis
The results of multivariate regression analysis are provided in Table 2. Referral methods were associated with the rate of uptake of referral but not with study country, time points of screening and referral interventions. The uptake rate where on-site assessment or treatment was used was significantly higher than the rate where the intervention was a referral to the mental health sector (OR = 1.31, 95% CI 1.13–1.52).
Table 2. Multivariate meta-regression analysis of referral rate
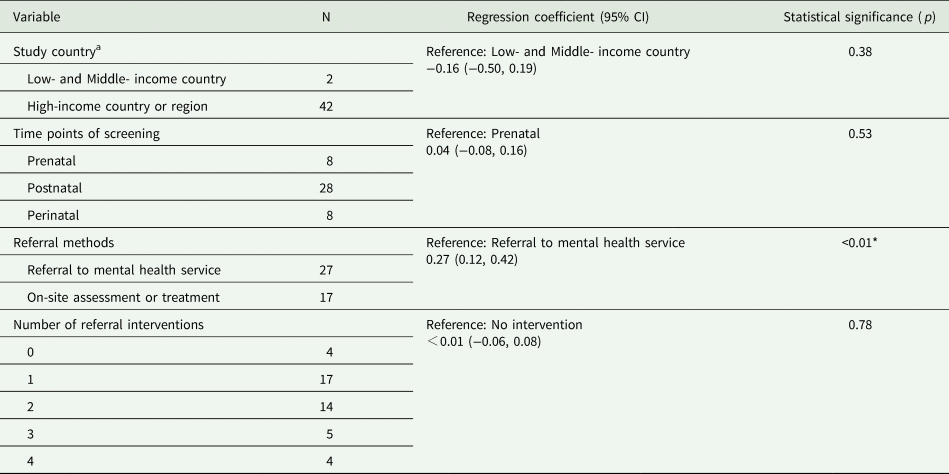
a Income based on World Bank classifications.
*p < 0.05.
Subgroup analyses
Subgroup analyses by referral methods showed significant differences in the uptake rate (χ 2 = 17.95, p < 0.01). Studies that provided on-site assessment or treatment had higher rates (60%, 95% CI 51–69%) than studies that referred women to mental health service (32%, 95% CI 23–41%).
Referral interventions for women who were screened positive
Table 3 shows the referral interventions in eligible studies. Table 4 shows the characteristics of the RCT, which showed a significant difference in uptake rates between intervention and control group.
Table 3. The nature of referral interventions among included studies
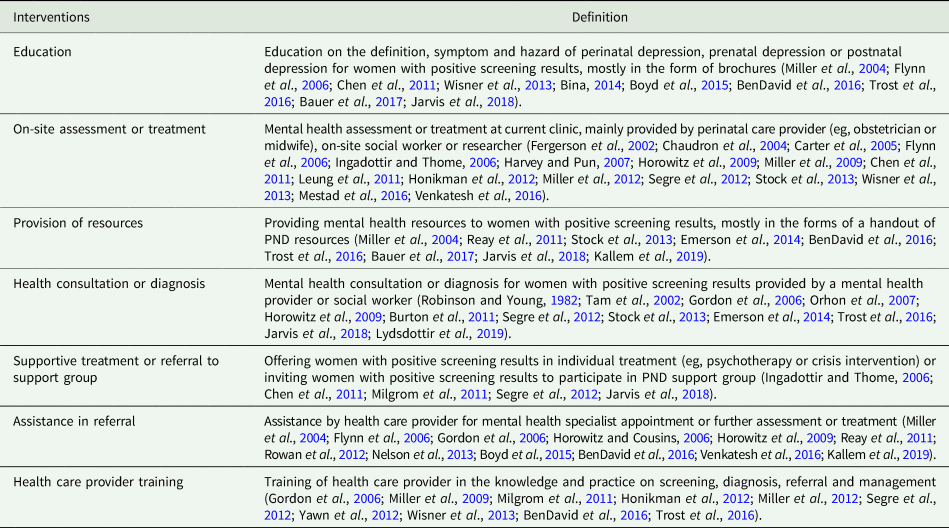
Table 4. Characteristics of the experimental study included
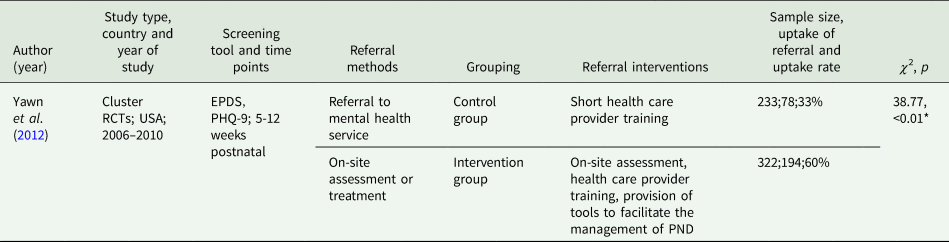
*p < 0.05.
The reasons for non-uptake among screen-positive women
We examined the reasons for non-uptake at women or provider levels. For the former, the most frequent reasons were ‘lack of time’ and ‘perception that mood had improved’. Others cited ‘cost concerns’ or ‘transportation problems’. The perception of the nature of PND also affected referrals. Some declined referral because of stigma associated with psychiatric treatments. Some thought ‘it is normal to have some depression in the puerperium’ and therefore did not perceive the need for further health care. Women's preferences for the type of service offered also influenced the level of acceptance. It was reported that women were ‘not interested in receiving specialised services; home visitation was generally a much more acceptable referral’ and some women tended to ‘use their own resources’ instead of resorting to support provided by the research team. The reasons related to health care provider level mainly concerned the interaction between women with positive screening results and health care providers. Some women declined because of disagreement with their health care providers. For instance, some women wanted ‘a quick fix’ while psychiatrists ‘looked for something long term like counseling’. Meanwhile, the attitude of providers could influence referrals. ‘Women appreciated health professionals who gave their time, acknowledged their feelings and offered support’; and ‘when women's feelings were denied, when they felt unable or were not given the opportunity to talk, then the experience of seeking help could be a very negative one’.
Discussion
Principal findings
Our systematic review and meta-analysis identified 41 studies that reported the uptake rate of referral and the effect of interventions for women with positive PND screening results. These included 39 observational studies and one quasi-experimental study (total N = 9380 women with positive screening results) which were used to estimate the pooled uptake rate, and one RCT (N = 555 women with positive screening results) which was used to evaluate the effectiveness of referral interventions. The overall pooled uptake rate for women with positive screening results was 43% (95% CI 35–50%). Where the women were referred to was the most important determinant. Studies that provided on-site assessment or treatment had higher uptake rates than studies that referred the women to a separate mental health service. The RCT showed significant improvement in uptake rates after the implementation of referral interventions. The more frequently mentioned reasons for refusing referral were ‘lack of time’ and ‘perception that mood had improved’.
Comparison with other studies and guidelines
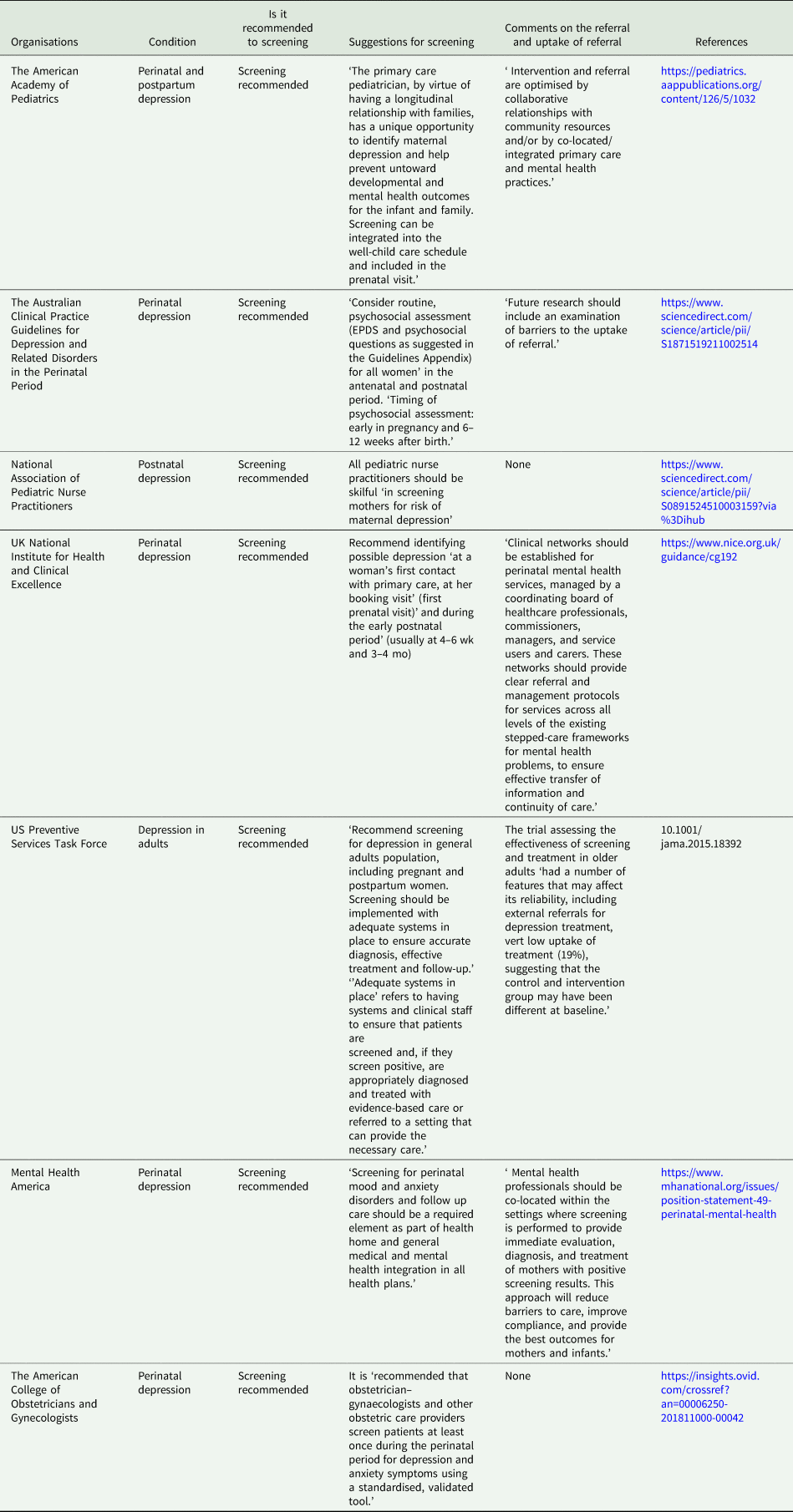
Compared to Byatt et al. (Reference Byatt, Levin, Ziedonis, Moore-Simas and Allison2015) and Long et al. (Reference Long, Cramer, Jenkins, Bennington and Paulson2019), we focused on the uptake rate and the effectiveness of interventions. We showed that nearly 60% of women with positive screening results do not take up the offers for referrals to psychological/psychiatric services after screening. This uptake rate is considerably lower than those in other screening programs, such as cancer screening (Yabroff et al., Reference Yabroff, Washington, Leader, Neilson and Mandelblatt2003; Callen et al., Reference Callen, Westbrook, Georgiou and Li2012; Dalton, Reference Dalton2018). Such a low uptake rate will reduce the utility of screening programs. The low uptake raises the importance of finding the reasons for it and developing the strategy for improvement. We note that government or professional bodies in many high-income countries have recommended screening for PND (Appendix E). For seven of them, only five included any comments on the challenge presented by a low uptake rate or suggestions on how this can be improved. Our findings suggest that it is an important oversight that needs to be addressed.
Among the different methods of referral, on-site assessment or treatment appeared to be more effective. Previous studies have shown that women who received referrals to the same site as their prenatal or postnatal care were more likely than those referred offsite (Smith et al., Reference Smith, Shao, Howell, Wang, Poschman and Yonkers2009; Flynn et al., Reference Flynn, Henshaw, O'Mahen and Forman2010; Price et al., Reference Price, Coles and Wingold2017). Access to further assessments and treatment on-site is more convenient and would reduce the degree of stigma and therefore more acceptable to women. To achieve on-site referral, mental health services are needed in the perinatal health care settings. However, collocated mental health professionals are likely to be absent in almost all resource-poor areas (Patel and Prince, Reference Patel and Prince2010). Equipping perinatal health providers with the capacity of providing basic mental health services may be a practical option. It is important to note that among the 40 eligible observational or quasi-experimental studies in our review, all but two were conducted in high-income countries or regions. As epidemiological evidence indicates PND is more common in low-and middle-income countries (Akhtar and Landeen, Reference Akhtar and Landeen2007; Shidhaye and Giri, Reference Shidhaye and Giri2014), and that many of these countries have huge populations (Patel and Prince, Reference Patel and Prince2010), this inequity needs to be addressed urgently. An important global health priority would, therefore, be to conduct locally relevant research in low-and middle-income countries, especially the evaluation of the feasibility and cost-effectiveness of approaches to provide on-site assessment and treatment (for example, the use of mobile health technology or the training of perinatal care providers).
We found that the quality of the evidence on the effectiveness of the interventions to increase uptake was weak, as there was only one RCT that showed ‘high risk’ in performance bias. Furthermore, we note that interventions examined in previous studies tended to lack considerations for support from the woman's family, which was found to influence women's response to referral (Dennis, Reference Dennis2005; Ahmed et al., Reference Ahmed, Stewart, Teng, Wahoush and Gagnon2008). Another important consideration in improving the design of interventions is to collect qualitative information on the barriers to mental health services. In this review, among the two more frequent reasons mentioned were ‘lack of time’ and ‘perception that mood had improved’. The former may be addressed by improving the accessibility of health care services (including time, costs and transportation) (Lara-Cinisomo et al., Reference Lara-Cinisomo, Wisner, Burns and Chaves-Gnecco2014; Nagle and Farrelly, Reference Nagle and Farrelly2018; Jones, Reference Jones2019). As the changes in circumstances for women and their families in the perinatal period can often be overwhelming, convenience when designing interventions would be important. The latter may reflect beliefs and cultural attitudes that may be modified by interventions aimed at improving knowledge about depression (Sword et al., Reference Sword, Busser, Ganann, McMillan and Swinton2008; Canty et al., Reference Canty, Sauter, Zuckerman, Cobian and Grigsby2019).
Strengths and limitations
Strengths of this review included: first, our research question focused on the uptake of referral by women with positive PND screening results which has not been reported in previous reviews; second, we examined the effect of interventions and reasons of non-uptake to inform screening programs as well the design of further research to increase uptake of referral. Our review has several limitations. First, in the protocol registered with PROSPERO, the subject of the review is on referral in general. For reasons explained in detail in the Introduction, this review focuses on uptake rather than all three steps in the referral and treatment process. Second, the heterogeneity for the pooled uptake rate was high across the eligible studies. Only the referral method was identified as a moderator of the observed heterogeneity, suggesting that future studies should further explore the factors that contribute to the high heterogeneity. Third, the quality of the included studies was an important limitation in estimating the uptake of referral and assessing the effectiveness of interventions to increase uptake, with only one RCT in 41 eligible studies. Fourth, we searched for publications in English and Chinese only and those that would have missed articles in other languages. Finally, we only included information from published studies when assessing uptake rates. As we do not have information from the ongoing services worldwide, we cannot exclude the possibility that the uptake rates from these services may be higher than those reported in published studies.
Implications
We find that almost three-fifths of women with positive perinatal depression screening results do not take up the offers for referrals to mental health service. In countries where screening is recommended, the reasons behind this low uptake should be assessed. Though efforts to address the challenge will be hampered by the weak overall quality of evidence on interventions to increase uptake, there is some suggestion that referral to on-site assessment and treatment may be helpful. Finally, as little is known in low-and middle-income countries where most affected women live, this issue should be addressed as an important global health research priority.
Data
All the data supporting the findings of this meta-analysis have been provided in Tables and Figures.
Acknowledgements
We thank Lu Liu, Qiao Li, Jie Wang, Ping Ye and Xiaodi Ma, all from Central South University, for literature searches, screened articles for inclusion and extracted data.
Financial support
This work was funded by The National Nature Science Foundation of China (grant No 81773446, 81402690).
Conflict of interest
None.
Ethical standards
This research did not involve human and/or animal experimentation.
Appendix A: Search Strategy
Search Strategy (PubMed, -2019/01)
Search Strategy (Cochrane Library, -2019/01)
Search Strategy (Web of Science, -2019/01)
Search Strategy (Embase, -2019/01)
Search Strategy (Ovid, -2019/01)
Search Strategy (CNKI, -2019/01)
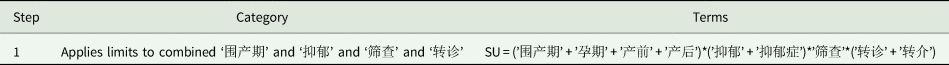
Search Strategy (Wanfang, -2019/01)
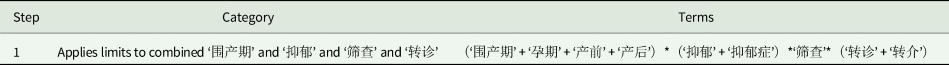
Search Strategy (VIP, −2019/01)
Appendix B: Results of quality assessment of the included RCT
Appendix C: Patient outcomes reported by included studies
Appendix D: Funnel plot of the meta-analysis of referral uptake rates
Appendix E: Recommendations from different organisations on perinatal depression screening