Introduction
The regional variation in the prevalence of common mental disorders has been suggested, with North and South East Asian countries having lower prevalence estimates than countries in other regions (Steel et al. Reference Steel, Marnane, Iranpour, Chey, Jackson, Patel and Silove2014). The recent burden of disease reviews for anxiety and mood disorders also identified comparatively low prevalence rates in the North and South East Asia region (Baxter et al. Reference Baxter, Scott, Vos and Whiteford2013; Ferrari et al. Reference Ferrari, Somerville, Baxter, Norman, Patten, Vos and Whiteford2013). Unmet need for treatment has been reported generally both in developing and developed countries (Wang et al. Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gureje, Haro, Karam, Kessler, Kovess, Lane, Lee, Levinson, Ono, Petukhova, Posada-Villa, Seedat and Wells2007), and substantial proportion of patients with severe disorders have not received any care (Wang et al. Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gureje, Haro, Karam, Kessler, Kovess, Lane, Lee, Levinson, Ono, Petukhova, Posada-Villa, Seedat and Wells2007).
In Japan, a community-based survey conducted in early 1990s reported generally lower lifetime prevalence for most Diagnostic and Statistical Manual of Mental Disorders (third edition revised; DSMIII-R) mood and anxiety disorders (Kitamura et al. Reference Kitamura, Fujihara, Iwata, Tomoda, Kawakami, Nakane and Radford1999) than in developed Western countries. Another community-based survey in an urban population in late 1990s, using the Composite International Diagnostic Interview (CIDI) (Kessler et al. Reference Kessler, McGonagle, Zhao, Nelson, Hughes, Eshleman, Wittchen and Kendler1994), found lower prevalence of anxiety, mood and alcohol use disorders in Japan than in Western countries (Kawakami et al. Reference Kawakami, Shimizu, Haratani, Iwata and Kitamura2004). The former study also reported a very low treatment rate in Japan, with only 10% of those with mental disorders seeking medical treatment (Kitamura et al. Reference Kitamura, Fujihara, Iwata, Tomoda, Kawakami, Nakane and Radford1999).
The World Health Organization (WHO) established the World Mental Health (WMH) Survey Consortium in 2000 to study unmet need for treatment of mental disorders across developed and developing countries (Kessler et al. Reference Kessler, Haro, Heeringa, Pennell and Ustun2006). A coordinated series of WMH surveys has subsequently been conducted in 28 countries around the world, including Japan. The WMH Japan Survey was conducted from 2002 to 2006. The preliminarily report of the WMH Japan Survey conducted in 2002–2003 showed lower 12-month prevalence of mental disorders in Japan compared with most Western countries (Kawakami et al. Reference Kawakami, Takeshima, Ono, Uda, Hata, Nakane, Nakane, Iwata, Furukawa and Kikkawa2005). The treatment rate in Japan based on this report was lower than that in the WMH surveys in most developed countries in Europe and the USA but slightly higher than in China, Columbia or Lebanon (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004; Kawakami et al. Reference Kawakami, Takeshima, Ono, Uda, Hata, Nakane, Nakane, Iwata, Furukawa and Kikkawa2005). However, this initial report was based on a small WMH Japan sample (n = 1663) based on a survey carried out only in the Western part of Japan.
The present paper aims to update the results from the earlier WMH Japan report using the final set of data from the full WMH Japan Survey conducted from 2002 to 2006 (n = 4130), reporting data on 12-month and lifetime prevalence, comorbidity, severity, treatment and demographic correlates of common mental disorders. This paper also compares impairments in role functioning due to mental disorders and chronic physical disorders and closes with a discussion of the implications of findings for mental health policy in Japan.
Methods
Survey population and subjects
A total of 11 communities in Japan were selected as study sites between 2002 and 2006 for the WMH Japan Survey. A full report of the methods employed within the WMH Japan Survey can be found in elsewhere (Kawakami et al. Reference Kawakami, Takeshima, Ono, Uda, Hata, Nakane, Nakane, Iwata, Furukawa and Kikkawa2005). The sites included three urban cities (Okayama, Nagasaki, Yokohama) and eight rural municipalities (Tamano in Okayama prefecture, Kushikino, Fukiage, Ichiki and Higashi-ichiki in Kagoshima prefecture, Sano in Tochigi prefecture, tendo and Kaminoyama in Yamagata prefecture). These sites were selected in consideration of geographic variation and the availability of site investigators. Participants were randomly selected from Japanese-speaking residents in each site aged 20 years or older, based on a voter registration list or a resident registry. Each site excluding Nagasaki site used following two survey methods; an invitation letter was sent to each subject and then an interviewer visited the homes of the subjects to seek permission to participate in the survey, or community volunteers first contacted the subjects in their homes to recruit them into the survey. At the Nagasaki site, an invitation letter was sent to each subject, and an interviewer conducted the face-to-face interview with those who replied positively. After they received invitation letters, trained interviewers visited them, and face-to-face interviews were conducted for those who agreed to participate in the study. The interview schedule was determined according to the Japanese computer-assisted personal interview version of the WMH version of the WHO CIDI (WMH-CIDI), a fully-structured diagnostic interview. Participants in all sites excluding Yokohama site were provided a coupon equivalent to 2000 JPY (approximately 18 USD), while participants in Yokohama site were provided a coupon equivalent to 2500 JPY (approximately 20 USD). A total of 4130 respondents participated in the study. The final response rate was 55.1%. A pilot study by trained lay interviewers using the Japanese version of WMH-CIDI with a small number of clinical patients showed good concordance between clinical diagnosis and WMH-CIDI diagnosis of major depression and alcohol abuse/dependence (Sakai et al. Reference Sakai, Ito, Takeuchi and Kikkawa2003).
The interview was divided into two parts to reduce respondent burden. Part I, administered to all respondents, included the core diagnostic assessment of mental disorders. Part II included correlates of core disorders. Part I was administered to all respondents and Part II to all Part I respondents who met criteria for any mental disorder plus a probability subsample of approximately 10% of other Part I respondents (n = 1682). All respondents were weighted to adjust for differential probabilities of selection and post-stratified to match the population distributions on the cross-classification for sex and age, for which the non-response weight in a given group for sex and age was the inverse of the response rate in this category (Kawakami et al. Reference Kawakami, Takeshima, Ono, Uda, Hata, Nakane, Nakane, Iwata, Furukawa and Kikkawa2005). Part II respondents were weighted by the inverse of their probability of selection for part II of the interview (Kawakami et al. Reference Kawakami, Takeshima, Ono, Uda, Hata, Nakane, Nakane, Iwata, Furukawa and Kikkawa2005).
Written consent was obtained from each respondent. The Research ethics Committees of Okayama University (for the Okayama site, reference No 78, approved on 9/18/2001), Yamagata University (for the Yamagata site, reference Nos 17 and 47, approved on 9/6/2004 and 10/18/2005, respectively), Jichii Medical University (for the Tochigi site, reference No eki03-13, approved on 12/10/2003), Juntendo University (for Yokohama City, reference No 17065, approved on 2/20/2006), and Tokyo University (for the Kagoshima and Nagasaki site, reference No 1582, approved on 12/25/2006) approved the protocol of the present survey.
Diagnostic assessment
WMH-J diagnoses were based on the Japanese version of WMH-CIDI, which was developed by an expert group and checked through an expert review and back-translation procedure. Common mental disorders included: anxiety disorders (agoraphobia, generalized anxiety disorder (GAD), panic disorder, post-traumatic stress disorder (PTSD), social phobia, specific phobia); mood disorders (major depressive disorder, bipolar I and II disorders, dysthymia); substance disorders (alcohol abuse with/without dependence, drug abuse with/without dependence); and impulse-control disorders (intermittent explosive disorder (IED)). Any mental disorders in the survey included common mental disorders listed above, and did not include schizophrenia, autism, dementia, intellectual disability and personality disorders. Disorders were assessed using the definitions and criteria of the Statistical Manual of Mental Disorders, fourth edition (DSM-IV). This instrument demonstrated acceptable reliability and validity (Haro et al. Reference Haro, Arbabzadeh-Bouchez, Brugha, de Girolamo, Guyer, Jin, Lepine, Mazzi, Reneses, Vilagut, Sampson and Kessler2006).
We assessed chronic physical disorders using a standard chronic disorders checklist (Hyattsville, Reference Hyattsville2004). It included allergies, asthma, cancer, cardiovascular (hypertension, heart attack, other heart disease), diabetes, musculoskeletal disorders (arthritis, chronic back/neck pain), chronic headaches, other chronic pain disorders, ulcer, stroke, tuberculosis, other chronic lung diseases and epilepsy. For symptom-based disorders such as chronic pain, respondents were asked to report whether they had each of them in the past 12 months. For each of the silent disorders such as diabetes, they were asked whether a doctor ever told them they had the condition and, if so, whether they continued to have that disorder in the past 12 months. Checklists of this sort had been shown to yield more complete and accurate reports than open-ended questions (Schoenborn et al. Reference Schoenborn, Adams and Schiller2003).
Severity and role impairment
The WMH-CIDI/DSM-IV disorders within 12 months were classified into three groups (severe, moderate and mild) following previously proposed criteria (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004) for a comparison purpose. Severe disorders were defined as either of the following four conditions: (a) those meeting the criteria for bipolar I disorder or substance dependence with a physiological dependence syndrome; (b) a suicide attempt in conjunction with any other mental disorder; (c) reporting at least two areas of role functioning with severe role impairment due to a mental disorder in the disorder-specific Sheehan Disability Scales (SDS) that measured four domains of role impairments, including work, home management, social life and close relationships (Leon et al. Reference Leon, Olfson, Portera, Farber and Sheehan1997); or (d) reporting overall functional impairment at a level consistent with a Global Assessment of Functioning (Endicott et al. Reference Endicott, Spitzer, Fleiss and Cohen1976) not more than 50 in conjunction with any other WMH-CIDI/DSM-IV disorder (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004). Respondents who were not classified as severe were then classified as moderate if the interference in role functioning was rated at least moderate in any SDS domain or if the respondent had substance dependence without a physiological dependence syndrome. All other disorders were classified as mild (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004).
The SDS scale (Sheehan et al. Reference Sheehan, Harnett-Sheehan and Raj1996) was also administered for one physical disorder selected randomly from among all the physical disorders reported by a respondent, as well as for each mental disorder reported by respondents, to compare impairments in role functioning among mental and physical disorders. To correct bias arising from underrepresented physical disorders due to the probability sampling of these disorders, a weight was applied to each case equal to the number of physical conditions. Then the impairment was categorized into two groups according to the highest SDS domain score across the four domains: severe (7–10) and not severe (0–6).
Treatment within 12 months
Treatment was classified into the following three sectors: mental health specialty (psychiatrist, psychologist, other mental health professional in any setting), general medical care (other general medical doctor or nurse) and non-health care (human services such as religious provider, social worker or counselor in a non-mental health setting and complementary and alternative Internet group, self-help group, or alternative provider). Further, health-care service was defined as mental health specialty or general medical.
Other covariates
Socio-demographic correlates included sex (males, 47.1%, females, 52.9%) and age cohorts [aged 18–34 years (23.2%), 35–49 years (23.0%), 50–64 years (26.9%), and ≥65 years (26.9%)]. For marital status, participants were categorized into two groups: married (72.8%) and not married (27.2%). For educational level, participants were categorized into four groups according to completed years of education [0–11 years (27.9%), 12 years (35.2%), 13–15 years (18.9%), 16 years or more (18.0%)]. For household income, participants were divided into two categories using average income of participants [below average (50%) and above average (50%)]. For employment status, participants were divided into five groups: working, student, homemaker, retired and other.
Statistical analyses
Data were reported on lifetime prevalence, 12-month prevalence, severity, and treatment. Persistence of the disorders was defined as a proportion of 12-month cases among lifetime cases (McLaughlin et al. Reference McLaughlin, Green, Gruber, Sampson, Zaslavsky and Kessler2010). Multivariable logistic regression was modeled to study socio-demographic predictors. Standard errors (s.e.) of descriptive statistics were estimated using the Taylor series method. Multivariate significance tests were based on Wald χ 2 tests. The logistic regression coefficients were transformed to odds ratios (OR) with design-adjusted 95% confidence intervals (CI). The statistical significance level was set at 0.05 for a two-sided test. All analyses were performed using SAS version 9.4.
Results
Lifetime and 12-month prevalence and comorbidity
Among the samples (n = 4130), males and females were included; age ranges were 20–98 years old, with a mean age of 53.6. Twelve-month prevalence of any mental disorder was 7.6%. The rank-order of 12-month prevalence estimates was different to that of lifetime prevalence estimates (Table 1). The classes of disorder with highest lifetime prevalence were anxiety disorders (8.1%) and substance use disorders (7.4%), and that with highest 12-month prevalence were anxiety disorders (4.9%) and mood disorders (2.3%). The proportion of 12-month to lifetime cases was highest for anxiety disorders (60.9%), and lowest for substance use disorders (12.9%). Individual disorders with highest lifetime prevalence were alcohol abuse or dependence (7.3%) and major depressive disorder (6.1%), and those with highest 12-month prevalence were specific phobia (2.3%) and major depressive disorder (2.2%). This inversion might reflect the fact that specific phobia had a persistent course reflected in high proportion of 12-month to lifetime cases (68.0%).
Table 1. Lifetime and 12-month prevalence of specific World Health Organization Composite International Diagnostic Interview/Diagnostic and Statistical Manual of Mental Disorders fourth edition (WMH-CIDI/DSM-IV) common mental disorders and the comorbidity, and prevalence and proportions of 12-month cases by the severity among 4130 respondents of the World Mental Health Japan Survey, 2002–2006
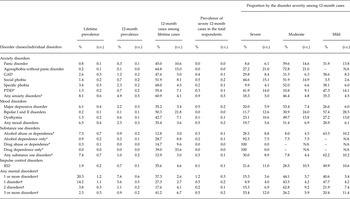
GAD, generalized anxiety disorder; ICD, intermittent explosive disorder; NA: not applicable; PTSD, post-traumatic stress disorder
* Part II sample.
† Part II sample. No adjustment was made for the fact that one or more disorders in the category were not assessed for all part II respondents.
–, no cases.
Disorder severity
Among those with any 12-month disorder, 15.3% were classified as severe, 44.1% moderate and 40.6% mild (Table 1). Regarding class of disorder, the most prevalent 12-month severe disorder in the total sample was anxiety disorders (0.9%). Substance use disorders had the highest percentage of severe cases (30.0%), followed by impulse control disorders (21.6%).
Twelve-month treatment
Among all respondents, 5.3% received any treatment. Among respondents who received treatment, 9.9% had severe cases, 13.0% moderate cases, 9.2% mild cases and 67.9% subthreshold cases. Table 2 shows the proportion of each sector of treatment. Among respondents with any mental disorders, 21.9% had received any treatment, 19.5% had received health care and 6.45% had received non-health care. Severe cases were more likely to receive treatments than moderate and mild cases (44.1, 19.7 and 15.9%, respectively). Most common sector of treatment for all cases as well as severe/moderate cases was mental health specialty. Respondents with substance use disorders and IED were less likely to receive any treatment than those with mood disorders and anxiety disorders (83.7 and 82.5% v. 61.3 and 75.9%). Among respondents with substance use disorders, general medical treatment was most common, while mental health specialty was most common in the other three classes of disorders.
Table 2. Association of 12-month World Health Organization Composite International Diagnostic Interview/Diagnostic and Statistical Manual of Mental Disorders fourth edition (WMH-CIDI/DSM-IV) disorder severity with treatment in Part II samples of the World Mental Health Japan Survey, 2002–2006 (n = 1682)*
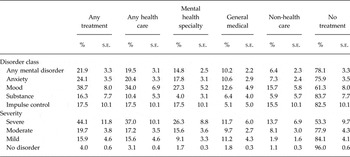
* Significant differences in a proportion for any treatment, mental health specialty, health care, absence of health care and proportion of no treatment among the three categories of a disorder (all P < 0.05).
Socio-demographic predictors of prevalence, severity and treatment
The pattern of socio-demographic correlates of lifetime prevalence was quite different to that of 12-month prevalence (Table 3). Any lifetime mental disorder was more prevalent among males and middle-aged groups (OR, 0.74; 95% CI, 0.54–1.00 and OR, 2.05; 95% CI, 1.19–3.54), and any 12-month mental disorder was more prevalent among females and younger age groups (OR, 1.42; 95% CI, 0.95–2.13 and OR, 3.29; 95% CI, 1.51–7.17). Regarding persistence of disorders, being female and younger age were risk factors of having 12-month mental disorders among lifetime cases (OR, 2.27; 95% CI, 1.28–4.03 and OR, 2.61; 95%CI, 1.05–6.44, respectively) (Table 3). Being presently not married was a risk factor of severe cases (OR, 3.01; 95% CI, 1.40–6.48). Females, younger age groups, respondents who were not working, and those with severe disorders were significantly more likely to receive treatment than mild/moderate disorders.
Table 3. Predictors of lifetime and 12-month prevalence, severity and any treatment for World Health Organization Composite International Diagnostic Interview/Diagnostic and Statistical Manual of Mental Disorders fourth edition (WMH-CIDI/DSM-IV) common mental disorders: the World Mental Health Japan Survey, 2002–2006 (part II sample, n = 1682)
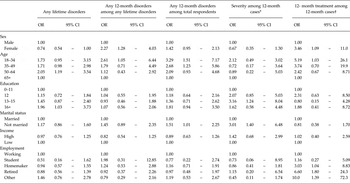
* Severe or moderate (coded = 1) v. mild (coded = 0) among those who experienced any 12-month disorder.
† Controlling for disorder severity.
Socio-demographic predictors of each disorder class
Female respondents were more likely than males to experience anxiety disorders and mood disorders (1.9 v. 3.0% and 0.56 v. 1.7%, respectively), and less likely than males to experience substance use disorders and impulse control disorders within 12 months (0.15 v. 0.80% and 0.31 v. 0.38%, respectively). Young respondents were more likely than other respondents to experience all types of mental disorders within 12 months (data available on request). Table 4 presents the results of multivariable logistic regression analyses for the association between each disorder class and socio-demographic characteristics. Anxiety disorders were more prevalent among those who were younger and presently not married. Mood disorders were more prevalent among those who were female, young and well-educated. Substance use disorders were more prevalent among males. Impulse control disorders were more prevalent among working respondents.
Table 4. Socio-demographic correlates of 12-month prevalence of common mental disorders by disorder class: the World Mental Health Japan Survey, 2002–2006
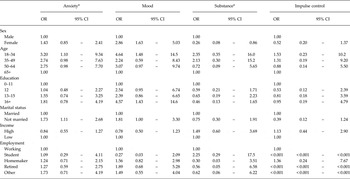
* Part II sample.
Impairment in role functioning due to chronic physical and mental disorders
Table 5 shows comparison rates of severe impairment associated with mental and chronic physical disorders in the past 12 months. The three most common chronic physical disorders were allergies (16.8%), back/neck pain (15.9%) and high blood pressure (14.0%), which were more than double prevalent than any mental disorders (7.6%). At the individual level, proportions of respondents with each disorder who reported severe role impairment due to the disorder were highest for trauma, cancer, heart attack and mental disorders. The estimated numbers of people in Japan with severe disorder-specific impairment were presented on the left column of Table 5. At the societal level, taking into consideration both disorder prevalence and individual-level impact, the estimated number of people in Japan with severe disorder-specific impairment was highest for back/neck pain (3494 thousand) followed by mental disorders (2577 thousand).
Table 5. Proportions of respondents with severe impairment caused by physical and mental disorders in the past 12 months, and estimated number of people in Japan with severe disorder-specific impairment: the World Mental Health Japan Survey, 2002–2006
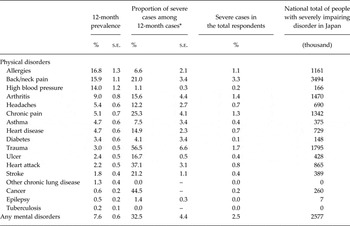
* Having severe impairment (7–10) of the highest Sheehan Disability Scale domain score across the four domains.
Discussion
The present study, using the final data set from the WMH Japan Survey conducted between 2002 and 2006, reported 12-month prevalence of common mental disorders, disorder severity and treatment in Japan. In general, the results were consistent with our previous report (Kawakami et al. Reference Kawakami, Takeshima, Ono, Uda, Hata, Nakane, Nakane, Iwata, Furukawa and Kikkawa2005) and other previous surveys in showing that mental disorders were highly prevalent (Weissman et al. Reference Weissman, Bland, Canino, Greenwald, Lee, Newman, Rubio-Stipec and Wickramaratne1996a , Reference Weissman, Bland, Canino, Faravelli, Greenwald, Hwu, Joyce, Karam, Lee, Lellouch, Lépine, Newman, Rubio-Stipec, Wells, Wickramaratne, Wittchen and Yeh b , Reference Weissman, Bland, Canino, Faravelli, Greenwald, Hwu, Joyce, Karam, Lee, Lellouch, Lépine, Newman, Oakley-Browne, Rubio-Stipec, Wells, Wickramaratne, Wittchen and Yeh1997; McBain et al. Reference McBain, Salhi, Morris, Salomon and Betancourt2012; Baxter et al. Reference Baxter, Scott, Vos and Whiteford2013; Ferrari et al. Reference Ferrari, Somerville, Baxter, Norman, Patten, Vos and Whiteford2013; Steel et al. Reference Steel, Marnane, Iranpour, Chey, Jackson, Patel and Silove2014), and often went untreated (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004; Wang et al. Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gureje, Haro, Karam, Kessler, Kovess, Lane, Lee, Levinson, Ono, Petukhova, Posada-Villa, Seedat and Wells2007; McBain et al. Reference McBain, Salhi, Morris, Salomon and Betancourt2012). The 12-month prevalence of any mental disorders and the four classes of disorders were lower in Japan than in most of other participating WMH countries (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004). The 12-month prevalence of any mental disorder in WMH participating countries was reported to vary from 4.3% in Shanghai to 26.4% in the USA, with an interquartile range of 9.1–16.9% (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004). Also, a meta-analysis showed that pooled period prevalence of common mental disorder was 17.6% (95% CI, 16.3–18.9%) with low prevalence in high income countries in Asia (11.5%; 95% CI, 8.1–16.0%) (Steel et al. Reference Steel, Marnane, Iranpour, Chey, Jackson, Patel and Silove2014). The present findings are consistent with those of the earlier surveys in showing that a low prevalence of mental disorders was found in Asian countries. However, when considering the severity of health problems, it turned out that mental disorders were the second most prevalent cause of severe role impairment among chronic physical and mental disorders in Japan. We estimated about 2.6 million people in Japan suffering from severe role impairment due to mental disorders, which are an important target of the health care service as a whole in this country.
Similar patterns of 12-month prevalence observed in Japan and other WMH countries include: (1) anxiety disorders were the most common class of lifetime/12-month disorders (WHO International Consortium in Psychiatric Epidemiology, 2000; Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004); (2) the proportions of the samples with a serious disorder were smaller than the proportions with a mild disorder (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004); (3) major depressive disorder and specific phobia were the most common individual 12-month disorders like other WMH countries (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004). Alcohol abuse/dependence was less prevalent in 12-month, unlike other WMH countries, where alcohol abuse was one of the most common 12-month disorders. However, if we focused only on lifetime prevalence individual disorders, alcohol abuse/dependence was the most prevalent. This may reflect a shorter persistence of alcohol use/dependence in Japan. But it is also attributable to respondents’ underreporting of present alcohol–related problems due to social desirability or avoiding embarrassment. The prevalence of drug abuse/dependence in Japan was especially lower than in the USA and other Western countries (Bijl et al. Reference Bijl, de Graaf, Hiripi, Kessler, Kohn, Offord, Ustun, Vicente, Vollebergh, Walters and Wittchen2003; Kessler et al. Reference Kessler, Chiu, Demler, Merikangas and Walters2005b ).
While lifetime prevalence of any mental disorders was higher for men and middle-aged (35–64 years old) groups, persistence of common mental disorders was higher for women and younger groups. The gender patterns for both prevalence and persistence are different from those reported in the western countries (Seedat et al. Reference Seedat, Scott, Angermeyer, Berglund, Bromet, Brugha, Demyttenaere, de Girolamo, Haro, Jin, Karam, Kovess-Masfety, Levinson, Medina Mora, Ono, Ormel, Pennell, Posada-Villa, Sampson, Williams and Kessler2009; Patton et al. Reference Patton, Coffey, Romaniuk, Mackinnon, Carlin, Degenhardt, Olsson and Moran2014). The higher overall lifetime prevalence among males and the middle-aged are consistent with higher suicide rates among middle-aged males in Japan (Lamar, Reference Lamar2000). While a previous study did not find that female gender was associated with persistence of depressive symptoms in Japan (Kawakami et al. Reference Kawakami, Roberts, Lee and Araki1995), greater gender discrimination in Japan (United Nations Development Programme, 2013) may be associated with the female dominance in persistence of mental disorders. This should be replicated in other surveys in Japan and other Asian countries to understand if the pattern was Asian culture-related or specific to Japan. It would also be interesting to associate gender segregation experienced by a respondent with disorder persistence. With regard to persistence of each disorder classes, the proportion of 12-month to lifetime cases was highest for anxiety disorders, and lowest for substance use disorders. This inversion might reflect the more persistent course of anxiety disorders and mood disorders than substance use disorders.
Regarding socio-demographic correlates of 12-month disorders, women had a higher risk than men of any mental disorders, anxiety and mood disorders. Men had a higher risk than women of substance use. These results are consistent with a robust gender effect across the clinical subdomains of mental disorder (Baxter et al. Reference Baxter, Scott, Vos and Whiteford2013; Ferrari et al. Reference Ferrari, Somerville, Baxter, Norman, Patten, Vos and Whiteford2013; Steel et al. Reference Steel, Marnane, Iranpour, Chey, Jackson, Patel and Silove2014). All of four classes of mental disorders were more prevalent among young and middle-aged respondents than elder (not less than 65 years old) respondents. Those with high education were more likely to have mood disorders. This result is inconsistent with the earlier cross-national study (WHO International Consortium in Psychiatric Epidemiology, 2000), but a previous study reported that high socio-economic status in childhood had positive association with mood disorders in Japan (Honjo et al. Reference Honjo, Kawakami, Tsuchiya and Sakurai2014), and might explain the observed association between education and mood disorders in part. Another explanation is that increased perceptions of stigma among lower educated people led to underreporting of their symptoms. Those being not married had a greater risk of mood and anxiety disorders, that is also consistent with previous studies (WHO International Consortium in Psychiatric Epidemiology, 2000; Weissman et al. Reference Weissman, Bland, Canino, Faravelli, Greenwald, Hwu, Joyce, Karam, Lee, Lellouch, Lépine, Newman, Rubio-Stipec, Wells, Wickramaratne, Wittchen and Yeh1996b ). Disorder severity had association between marital status, and this result was consistent with the previous study (Shen et al. Reference Shen, Zhang, Huang, He, Liu, Cheng, Tsang, Lee and Kessler2006).
Only one out of five people with any mental disorders received any treatment in Japan in the study period. This treatment rate is lower than that in most other high-income countries included in the WMH surveys. The low treatment rate in Japan might partly reflect less health expenditure (8.35% of gross domestic product (GDP)), because the proportion receiving services was reported to correspond to countries’ percentages of GDP spent on health care (Wang et al. Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gureje, Haro, Karam, Kessler, Kovess, Lane, Lee, Levinson, Ono, Petukhova, Posada-Villa, Seedat and Wells2007). Also, stigma of mental illness is an important factor which affects treatment rates. The WMH Japan survey is the first to measure the association between severity and treatment in Japan, although previous large-scale surveys found the strong relationship between disorder severity and seeking treatment (Kessler et al. Reference Kessler, Frank, Edlund, Katz, Lin and Leaf1997; Bijl et al. Reference Bijl, de Graaf, Hiripi, Kessler, Kohn, Offord, Ustun, Vicente, Vollebergh, Walters and Wittchen2003; Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004). We found a strong association between severity and service use. However, the number of mild and subthreshold cases in treatment far exceeded the number of severe cases in treatment. Because the WMH surveys found that mild cases had little impairment of their functioning (Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004), to increase treatment rate for those with severe or moderate disorders should be a primary focus of the future mental health policy in Japan. We should also investigate if the present treatment is effective for these mild and subthreshold cases, and if there could be a better service or support for them. In addition, psychiatric outpatient clinics are largely increasing in Japan since WMH-Japan survey. This may lead to reduce the treatment gap for patients with mental disorders. Other factors that could affect service use were gender, age, educational status and employment status, though some of the associations were not significant. These results are consistent with other studies (Kessler et al. Reference Kessler, Brown and Broman1981; Demyttenaere et al. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess, Lepine, Angermeyer, Bernert, de Girolamo, Morosini, Polidori, Kikkawa, Kawakami, Ono, Takeshima, Uda, Karam, Fayyad, Karam, Mneimneh, Medina-Mora, Borges, Lara, de Graaf, Ormel, Gureje, Shen, Huang, Zhang, Alonso, Haro, Vilagut, Bromet, Gluzman, Webb, Kessler, Merikangas, Anthony, Von Korff, Wang, Brugha, Aguilar-Gaxiola, Lee, Heeringa, Pennell, Zaslavsky, Ustun and Chatterji2004). Women's diminished perceptions of stigma and their greater abilities to recognize their mental health problems can explain the increased service use among them (Kessler et al. Reference Kessler, Brown and Broman1981). Elderly people might avoid seeking mental health care because of the greater perceived stigma of mental disorders and treatments for people in this age range than for those who are younger (Leaf et al. Reference Leaf, Livingston, Tischler, Weissman, Holzer and Myers1985). Those well-educated may have more knowledge about mental disorders than those poorly educated (Leaf et al. Reference Leaf, Livingston, Tischler, Weissman, Holzer and Myers1985). Those who were not working may have time to seek mental health care, and also working people may hesitate to receive treatment because of stigma at their working place. Higher income showed a negative association with service use that may indicate that financial barrier was rather small in Japan, with universal insurance coverage.
The mental health specialty sector was the most common resource used by people in Japan, although the general medical sector was the largest source of mental health services for most countries (Wang et al. Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges, Bromet, Bruffaerts, de Girolamo, de Graaf, Gureje, Haro, Karam, Kessler, Kovess, Lane, Lee, Levinson, Ono, Petukhova, Posada-Villa, Seedat and Wells2007). This may reflect attempts by policymakers to strengthen human resources for mental health and decrease financial burden of treatment of mental disorders. Treatment rate for substance use disorders was especially low, and the most common service was the general medical sector. This result indicates the importance for gatekeeping by primary care physicians for mental disorders, especially substance use disorders.
The present result should be interpreted considering several limitations. The Japanese version of the WMH-CIDI was not fully validated against clinical diagnoses, although it was developed by an expert group and checked though an expert review and a back-translation procedure. However, a pilot study using the Japanese version of WMH-CIDI with a small number of clinical patients showed good concordance between clinical diagnosis and WMH-CIDI diagnosis of major depression and alcohol abuse (Sakai et al. Reference Sakai, Ito, Takeuchi and Kikkawa2003). The survey did not include schizophrenia because of the problems of non-response bias and overestimation of psychotic symptoms by lay people during structured interviews (Kessler et al. Reference Kessler, Birnbaum, Demler, Falloon, Gagnon, Guyer, Howes, Kendler, Shi, Walters and Wu2005a ). Another limitation was the possibility of selection bias. Weights were applied to the data to adjust for discrepancies between the sample and population data on the cross-classification of gender and age, due to frame under-coverage, non-response and sampling variability. Although we tried to adjust for differential response to match the population distributions, if the response rate was related to mental disorder, severity, or treatment beyond sex and age, the prevalence could be biased. The most plausible bias would be a conservative one, suggesting that the estimated prevalence rates reported here are likely to be lower bound estimates. Although previous studies suggest low prevalence of mental disorders in Asian countries, it is possible that our results might underestimate prevalence of mental disorders in Japan. CIDI has not been fully validated in Japanese and some methodological possibilities such as stigma-related conscious non-disclosure might explain the low prevalence estimates. Prevalence estimates were also subjected to recall bias, because only respondents who reported to have lifetime mental disorders were asked whether symptoms existed in the last 12 months. Also, Japan has the highest number of psychiatric beds in the world. Low prevalence and low treatment rate in this study could be affected by the fact that many patients with severe disorders were admitted to psychiatric beds. However, the most common mental disease among admitted patients was schizophrenia, and the second was dementia. Because both of these disorders were not included in the present study, we believe that the impact by high admission rate might be rather small. The lower response rate might also limit the interpretation of the findings, which might lead to either underestimation or overestimation of prevalence. The response rate was particularly low in Nagasaki site (26%) because a different survey method was used in Nagasaki site, although response rates in other survey sites were moderate to high (41–82%). Because excluding data from the Nagasaki site did not greatly alter the findings, we included the data in the analysis, together with data from other three sites. Although the survey included information about pharmacotherapy and duration of treatment, we could not include those information in our analysis because of missing data. For the estimated prevalence of cases with severe disorders, we selected criteria which were previously used for an international comparison (Sheehan et al. Reference Sheehan, Harnett-Sheehan and Raj1996). However, there might be alternative ways to define the severity and impairment. Also the present ratings of the severity and impairment for each disorder may be overestimated by the presence of comorbid health problems, particularly for mental disorders which have been known to frequently comorbid with other mental and physical disorders. We can overcome some of these limitations and expand the present findings in the ongoing WMH-Japan second survey. We have been working on the WMH-Japan second survey from 2013 to 2015, including people living in the areas stricken by the Great East Japan Earthquake. So in the near future, we will be able to compare results of WMH-J first and second survey, and explore the impact of revised diagnostic criteria of DSM-5 on prevalence estimates, and changes of mental health among people in Japan in the last 10 years.
Acknowledgements
Members of the World Mental Japan Survey Group include: Yutaka Ono, MD, National Center for Cognitive Behavior Therapy and Research, National Center of Neurology and Psychiatry; Yoshibumi Nakane, MD, Nagasaki University, Nagasaki, Japan; Yosikazu Nakamura, MD, MPH, FFPH, Department of Public Health, Jichi Medical School; Akira Fukao, MD, Department of Public Health, Yamagata University, Graduate School of Medical Science; Itsuko Horiguchi, Ph.D, Nagasaki University Tokyo Office; Hisateru Tachimori, Ph.D, National Institute of Mental Health, National Centre of Neurology and Psychiatry; Noboru Iwata, Ph.D, Department of Clinical Psychology, Hiroshima International University; Hidenori Uda, MD, Health, Social Welfare and Environmental Department, Kagoshima Regional Promotion Bureau, Kagoshima Prefecture, Japan; Hideyuki Nakane, MD, Department of Psychiatric Rehabilitation Science, Unit of Rehabilitation Sciences, Nagasaki University Graduate School of Biomedical Sciences; Makoto Watanabe, MD, Ph.D, Department of Preventive Cardiology, National Cerebral and Cardiovascular Centre; Masatsugu Oorui, MD, Sendai City Mental Health and Welfare Centre; Kazushi Funayama, MD, MPH, Ph.D, Yokohama City Institute of Health; Yoichi Naganuma, PSW, MSc, National Institute of Mental Health, National Centre of Neurology and Psychiatry; Toshiaki A. Furukawa, MD, Department of Health Promotion and Human Behaviour, Kyoto University Graduate School of Medicine; Masayo Kobayashi, MD, Department of Public Health, Jichi Medical School; Tadayuki Ahiko, MD, Yamagata Prefectural Institute of Public Health, Yamagata Prefecture; Yuko Yamamoto, Ph.D candidate, Department of Public Health, Juntendo University Graduate School of Medicine; Tadashi Takeshima, MD, National Institute of Mental Health, National Centre of Neurology and Psychiatry; Takehiko Kikkawa, MD, Seisen Jogakuin College.
Financial support
The WMH Japan Survey was supported by the Grant for Research on Psychiatric and Neurological Diseases and Mental Health from the Japan Ministry of Health, Labor and Welfare (H13-SHOGAI-023, H14-TOKUBETSU-026, H16-KOKORO-013, H19-KOKORO-IPPAN-011, H20-KOKORO-IPPAN-009). The funder had no role in the design, analysis, interpretation of results, or preparation of this paper.
Statement of Interest
R. Kessler has been a consultant for Hoffman-La Roche, Inc., Johnson & Johnson Wellness and Prevention, and Sanofi-Aventis Group. R. Kessler has served on advisory boards for Mensante Corporation, Plus One Health Management, Lake Nona Institute and U.S. Preventive Medicine. R. Kessler owns 25% share in DataStat, Inc.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.









