With advances in medical and surgical care, an increasing number of children born with CHD, including those with single-ventricle lesions, are surviving into adulthood. Reference Pundi, Johnson and Dearani1–Reference Barron, Kilby, Davies, Wright, Jones and Brawn3 The journey of individuals with single-ventricle CHD has many obstacles and challenges both medically and psychosocially. Reference Rodriguez and Book4–Reference Cantwell-Bartl and Tibballs7 These challenges are faced not only by the patients, but also by their families and other loved ones. As these patients mature, many find meaningful romantic relationships.
Partners of individuals with chronic illnesses face many obstacles and challenges of their own. Previous research has shown that spouses of individuals with chronic illnesses present symptoms similar to those of the burnout experienced by medical professionals, including depression, uselessness, and loneliness. Reference Ekberg, Griffith and Foxall8 In a study in Sweden involving partners of patients with chronic illnesses with at least 3 months duration, four themes were identified: ‘Managing challenges in daily life,’ ‘Seeking support and use own capabilities to manage life,’ ‘Appreciating the good parts of life,’ and ‘Adapting to constant changes and an uncertain future.’ Reference Eriksson, Wejåker, Danhard, Nilsson and Kristofferzon9 Increased support from the health care system was also desired. Reference Eriksson, Wejåker, Danhard, Nilsson and Kristofferzon9 In a group of spouses caring for individuals with acquired brain injury evaluated 2 years after initial injury, older age, more significant disability, longer duration of marriage, and presence of adult children were all independently associated with increased caregiver burden. Reference Laratta, Lucca, Tonin and Cerasa10
The current data available on spousal experience is primarily found in older couples with acquired chronic illness or injury. Scant information is available on younger couples with congenital conditions. While there are early data on the experiences of parents of children with CHD, no data exists about the experiences of spouses and partners of patients with CHD. The goal of the current qualitative pilot study was to evaluate the experience and challenges that partners of individuals with single-ventricle CHD encounter in their daily lives.
Methods
This study is part of a larger study analysing the lifetime journey of patients with single-ventricle CHD and their families. This initiative is the result of a unique diverse collaboration between three institutions at The University of Texas at Austin (UT): 1) the Texas Center for Pediatric and Congenital Heart Disease (UT Dell Medical School, UT Health Austin, and Dell Children’s Medical Center), 2) the Design Institute for Health (UT Dell Medical School and College of Fine Arts), and 3) the Value Institute for Health and Care (UT Dell Medical School and McCombs School of Business). This collaboration brought together clinicians, clinical and qualitative researchers, designers, and value-based health care specialists with different perspectives and experiences to understand the journey of individuals with single-ventricle CHD as well as that of their families and loved ones in a more comprehensive and unbiased way. The study was approved by the Institutional Review Board at the University of Texas at Austin (2019080031). Informed consent was obtained prior to enrolment in the study. The study was registered at ClinicalTrials.gov (NCT04613934).
Study population
Outpatient cardiology records between January 2017 and October 2019 were queried for patients with a potential diagnosis of SV CHD (including hypoplastic left heart syndrome, tricuspid atresia, unbalanced atrioventricular septal defect, and other single-ventricle variants). Outpatients or inpatients identified by the clinical team during the study, and their families, were also eligible for inclusion. Research team members confirmed eligibility based on diagnosis. Study flyers were posted in clinics and on social media inviting patients and families to contact the study team and determine eligibility. Patients and family members of patients who received cardiac care outside of our institution were eligible for inclusion.
Partners of patients 18 years of age and older who spoke either English or Spanish, after approval from the patient, were contacted via mail, email, and/or phone to inform them of the study and invite them to participate. Data were collected between February 2020 and September 2020. Participants were asked to complete an optional, limited socio-demographic survey as part of the study.
Experience Group sessions
This project utilises Experience Group sessions, a qualitative research methodology. This research method is designed to understand the lived experiences of individuals living with or affected by a medical condition. It utilises a grounded theory approach derived from social sciences research that includes inductive methods to generate insights directly from the data acquired. Reference Chapman, Hadfield and Chapman11 Experience Group session methodology does not have an a priori hypothesis, but allows the data to lead the development of themes and insights, potentially identifying participant insights that may not have been previously recognised as important needs and experiences. A particular characteristic of Experience Group sessions is the emphasis on grouping people with similar characteristics. Since participants tend to discuss with strangers things they have in common, a relatively homogeneous group of participants allows the participants to become “intimate strangers” and shares important elements of their experiences. It also recognises participants as the experts of their journey and experiences. Reference Guzik, McKinney and Ulack12 Sessions are lightly moderated by a non-clinical facilitator to avoid potential focus on preconceived ideas that researchers may have, allowing exploration of the participant’s experience and expertise.
Experience Group sessions are designed as 90-minute semi-structured discussions with facilitators asking general open-ended questions to encourage discussion. Examples of open-ended questions utilised to encourage conversation include What does a good day look like for you? What does a bad day look like? What are your goals? What are your fears? The facilitators additionally support the conversation to encourage and allow for all participants to have an opportunity to express and discuss their experiences both similar and in contrast to other participants’ experiences. Experience Group sessions were conducted virtually using HIPAA-compliant Zoom (www.zoom.us) due to the COVID-19 pandemic. Discussion topics included both participant daily experiences as well as aspects of care delivery that they and their partners experienced.
Audio recordings from Experience Group sessions were transcribed and underwent systematic coding utilising inductive thematic analysis using NVivo software (QSR International, Victoria, Australia). Study team members coded each transcript independently. No a priori codebook was utilised given the inductive nature of the analysis. Data from the sessions guided the themes identified by each individual coder. The coders met to review themes identified by each individual. A Modified Delphi Process was utilised to identify the main themes. Reference Dalkey13,Reference Jones and Hunter14 Coders undertook multiple rounds of discussion where each coder had opportunities to bring forward a proposed theme identified through their coding. There were subsequent comparisons of the themes identified amongst the coders to determine those that were consistently identified.
1:1 interviews
All partners were invited to participate in an EG session. If they were unable to participate in a session, they were invited to complete a 1:1 interview. Additionally, follow-up, in-depth interviews were conducted in a subset of participants and families from the Experience Group sessions to further explore their insights. An attempt was made to include participants with as diverse socio-demographic backgrounds and experiences as possible, as identified from the discussions during the experience Group sessions. These 1:1 interviews were performed to draw further insights from patients’ and partners’ lives. Similar to the experience Group sessions, all interviews were held online via HIPAA-compliant Zoom (www.zoom.us). Audio recordings from the interviews were transcribed. The transcripts were debriefed using group learning sessions and tagged for themes.
Results
All individuals with single-ventricle CHD who participated in the study and disclosed having a partner (n = 7) agreed to have the study team contact their partner to invite them to participate. A total of six (85.7%) partners of patients with single-ventricle CHD consented and were enrolled in the study. These included four (66.7%) males; all spoke English. All participants were partners of a single-ventricle CHD patient of the opposite sex and four (66.7%) were married. Five (83.3%) participated in an experience Group session, one (16.7%) participated in a primary one-on-one interview, and two (33.3%) who originally participated in an experience Group session took part in an additional in-depth 1:1 interview.
General themes
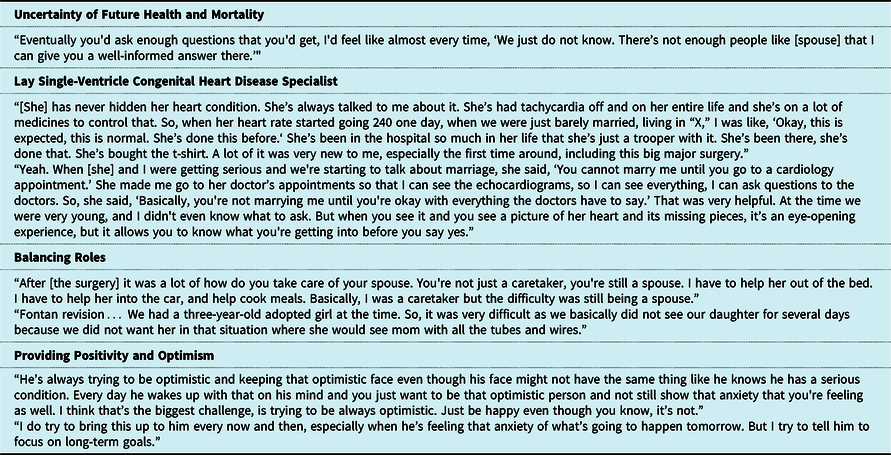
Four overarching themes were identified. These included: 1) Uncertainty of future health and mortality, 2) Becoming a lay SV CHD specialist, 3) Balancing roles, and 4) Providing positivity and optimism. Example quotes for each theme are presented in Table 1.
Table 1. Example quotes
Uncertainty of future health and mortality
Uncertainty of the future was discussed by all participants. This uncertainty was framed in both positive and negative terms. Many participants spoke about the uncertainty resulting from them and their partner taking advantage of every day and living in the moment. The negatively framed portion of the uncertainty included three main areas: the next complication or surgery, life expectancy, and family planning. Participants spoke of waiting for the next major single-ventricle CHD event to occur spanning from an arrhythmia requiring an emergency department visit and pacemaker changes, to liver dysfunction and major single-ventricle CHD surgical interventions. Most of the participants had been present for one of these types of events in their partner’s life, which heightened this negative anticipation.
As the participants are partners of some of the first generation of individuals with single-ventricle CHD to survive into adulthood, this leads to significant uncertainty of life expectancy. Many participants recount asking doctors for indications of life expectancy, with the answer eventually being “we don't know.” Participants expressed an understanding that there is a lack of significant long-term data available in the single-ventricle CHD population.
All but one participant spoke about the impact of family planning with their partner. The concerns with family planning and the inability to bear children came up early in relationships. Family planning was discussed by all male participants and one of the two female participants. Participants described receiving conflicting messages from providers on the ability to have children. The female participant spoke of the concern about passing on single-ventricle CHD to a child.
Becoming a lay single-ventricle CHD specialist
All participants acknowledged the complexity of single-ventricle CHD and spoke of the steep learning curve after meeting their partners. They all reported finding out about their partner’s single-ventricle CHD very early in their relationships, either through the partner offering up the information or the conversation being prompted by the sternotomy scar. Over time, participants became more facile with the diagnosis, complications, and unique aspects of their partner’s single-ventricle CHD including arrhythmias, Fontan revisions, and Fontan-related liver disease. They identified the most common external evidence of their partner’s single-ventricle CHD as a difficulty with significant physical activity.
All but one participant attended cardiology visits with their partners and many had experienced emergency department visits and/or cardiac surgeries with their partners. Participants discussed the sometimes uncomfortable nature of their partner receiving care in a paediatric setting, from having to explain to others in the surgery waiting room that it was their partner not their child who was undergoing surgery, to awkward interactions with providers and staff who are not used to caring for adults. They further expressed the importance of providers who have a strong understanding of not just adults with CHD, but single-ventricle CHD specifically.
Balancing roles
Participants expressed the challenges of balancing roles and responsibilities as a partner, parent, and a caregiver when needed by their partner. They reported difficulty in navigating hospitalisations of their partner and not wanting their children to see their parent in that setting. Participants also expressed the need for flexibility from their work in order to be able to quickly change plans if something medically came up with their partner.
Providing positivity and optimism
An overarching role for the partners, both said and unsaid, was providing optimism and positivity to their partner. Participants spoke frequently about the future and things like plans for retirement. They also spoke optimistically of scientific advances and the potential for future advances to improve and prolong their partner’s life. Participants reflected on being the support for their partners and redirecting them when they were “down” or pessimistic. Many stories and anecdotes expressed by the participants throughout the interviews and Experience Group sessions were very positive and optimistic in nature.
Overall
Overall, the participants grew into an advocate role for their partners. They became a second voice for their partners and found ways to support them to live their fullest and most meaningful lives with as few restrictions as possible.
Discussion
Surgical and medical advances in single-ventricle CHD over the last three decades have resulted in more children born with single-ventricle CHD living into adulthood. These advances have created a new cohort of partners of individuals with single-ventricle CHD with important needs and challenges. In this first-of-its-kind pilot investigation, the lived experiences of partners of individuals with single-ventricle CHD are explored. Overall, participants not only expressed a supportive role grounded in positivity but also reported challenges with uncertainty of future length and quality of life, while balancing roles as a partner, a caregiver, and in some cases, a parent. Despite single-ventricle CHD being a very complex medical condition, participants voiced a strong understanding of the condition, its history, and possible complications.
Uncertainty surrounding the condition was a significant theme throughout the sessions. Illness uncertainty and its impact on patients has been described in other conditions. Reference Guan, Santacroce, Chen and Song15–Reference Simpson, Zarotti and Varey17 Mishel described the “Uncertainty in Illness Theory”, a framework for how patients handle uncertainty surrounding a health condition. Reference Mishel18 According to this theory, through multiple steps and influences, patients make an appraisal of the uncertainty as either a danger or an opportunity to which they employ coping mechanisms and eventually adapt. Throughout a disease course, particularly in chronic illnesses, this appraisal can fluctuate between the two. Similarly, participants in this study voiced both opportunity and danger appraisals from the uncertainty experienced. In Mishel’s framework, “structure providers” such as social support and education work to reduce uncertainty. As the single-ventricle CHD population continues to age, more accurate data will be available with which to educate partners and patients. However, work must be done to determine the most effective methods of delivering that education.
Need for support underlies multiple themes discussed by the participants. Partner and caregiver support groups exist in many other disease settings, particularly in oncology. Reference Levy19 Support groups exist within the congenital heart community as well but are traditionally focussed on patients and parents. The lack of partner support groups likely stems from the relative recency to which that specific population developed. These support groups may serve as a component of the “structure providers” social support in Mishel’s framework. Beyond support groups, many partners may benefit from additional supports and directed educational initiatives. With one of the major themes identified as balancing their multiple roles, supports such as childcare, meal support, transportation, and other areas of support may benefit partners and families. Further work is needed to understand the specific needs of partners and how to efficiently provide those types of support.
While the relationship between a partner and an individual living with single-ventricle CHD is different than that of a parent of a child with single-ventricle CHD, it should be noted that some themes identified in the current study overlap with those expressed by parents in other investigations. Namely, the role of uncertainty and balancing of roles. Reference Elliott, Erickson, Russell, Chrisman, Gross Toalson and Emerson20 Given the differing relationships partners and parents have, these themes may be more pervasive throughout the lifelong journey of families impacted by single-ventricle CHD.
All participants reported a significant understanding of single-ventricle CHD in general and of the nuances of their partner’s individual condition. A majority of participants reported regularly attending clinic visits with their partner. The role partners play in chronic illness is complex and has been shown to have positive and negative impacts on patient health behaviours and outcomes. Reference Martire and Helgeson21 It is important to recognise the role, positive or negative, that the partner has in a patient’s care and to involve them in the care paradigm. Further, dyadic interventions have shown positive results in diabetes management, weight loss, and HIV medication adherence. Reference Martire and Helgeson21
In the uncertainty of those adults living with single-ventricle CHD, their partners provide a positive view of the future. Given the increased prevalence of mental health disorders in all adults with CHD, this positivity may provide a mechanism to prevent and/or manage these mental health conditions. Reference Westhoff-Bleck, Briest and Fraccarollo22 They also become a strong advocate within the health system for the patient. Given the complexities of the health system coupled with the complexities of single-ventricle CHD, this role is likely beneficial for individuals living with single-ventricle CHD. The need for this role in the health system should be a further call to action to rethink and redesign care delivery and resources around the needs of the individuals with single-ventricle CHD and their families.
Limitations
As a pilot investigation, this study has a small sample size. As such, the findings may not be representative of the broader population. However, as the themes identified were strongly present across the current participants, they are likely themes that would continue to be identified in a larger cohort. The limited sample size does potentially lead to missed themes that may become more apparent in a larger sample. Additionally, there is the potential for response bias as those who are interested in participating in research and a study such as this as well as those who consented to the study team contacting their partner, may have different backgrounds and experiences than those who chose not to participate. Further, all participants’ partners were currently in good health. It is possible that partners of individuals who are in worse health have a different lived experience. Additionally, all participants spoke English as their first language. As the socio-demographic questionnaire was optional to allow for as much participant anonymity as they desired, it was only completed by half of the participants which did not allow for an assessment of the impact of these factors on themes. Those living with single-ventricle CHD and their partners of different cultural or socio-economic backgrounds may have different experiences. As such, additional broader studies with this new population are critical to further our understanding.
Conclusion
Improvements in medical and surgical care of individuals with single-ventricle CHD have created a new population with important and different needs: their partners. The partners have a unique lived experience marked by uncertainty and continued evolution. It is imperative to include partners in the care paradigm as they play an important role with the patient. Further work is necessary to understand the generalisability of these findings as well as to determine nuances in the partner experience. This new and ever-growing population provides a significant opportunity to design care delivery around the needs of both those living with single-ventricle CHD and their partners and family.
Acknowledgements
We want to thank the entire Corage Project team for their work and support, including: Adam Zeiner, Michelle Mizrahi, Eileen Stewart, Christine Dillingham, Taylor Cook, Arotin Hartounian, Elizabeth McCullum, Stacey Chang, Scott Wallace, Elizabeth Teisberg, Alice Andrews, Diana Gonzalez, Sarah O’Hara, Amy Madore, Stephanie Morgan, Diego Ramonfaur, Jacob Strelow, Joel Suarez, and Laura Paquette.
Financial support
Research was funded by internal funds from Dell Medical School at The University of Texas at Austin and the Texas Center for Pediatric and Congenital Heart Disease at UT Health Austin and Dell Children’s Medical Center.
Conflicts of interest
None
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional review board of the University of Texas at Austin Dell Medical School.






