To the editor,
Deep brain stimulation (DBS) is the most effective treatment option for patients with pharmacologically intractable movement disorders, including monogenic, generalized dystonia. Reference Cif, Ruge and Gonzalez1,Reference Vidailhet, Vercueil and Houeto2 The evidence demonstrates its efficacy and ability to restore normal function over the long term. Reference Cif, Ruge and Gonzalez1
In the case of generalized dystonia, DBS can provide sustained and at least short-term effect, even after temporary discontinuation. Reference Grips, Blahak and Capelle3,Reference Ruge, Cif and Limousin4 It has been proposed that DBS modulates the central motor network by normalizing potentiation-like plasticity and GABAergic inhibition, which are expected to be abnormal in the case of dystonia. Reference Ruge, Cif and Limousin5 These modulatory changes can subsequently lead to less worsening of symptoms. Reference Ruge, Cif and Limousin5 Most reports have demonstrated this effect during short-term assessment (< 48 hours) after discontinuing DBS stimulation. Reference Grips, Blahak and Capelle3,Reference Ruge, Cif and Limousin5–Reference Grabli, Ewenczyk and Coelho-Braga7 Pregnancy, on the other hand, can represent a challenge for women with generalized dystonia and an in situ DBS. Reference Ziman, Coleman and Starr8
Herein, we present a case describing the pregnancy and delivery outcomes of a patient with DYT-THAP1 dystonia who discontinued her DBS stimulation throughout her pregnancy.
This is the case of a 32-year-old woman of polish ancestry, born at 35 weeks’ gestation through cesarean section delivery, with no motor or verbal regressions in developmental milestones. By the age of 6, she started to show slowly progressive dystonic posturing and cramping in her left foot. Symptoms further spread to entire left side of her body, and by age 12, there was cervical involvement. By the time she reached 18, she had noticed a spread to the jaw and the lower facial muscles, with further progression to severe posturing of the fingers of the right hand. Her initial examination at the movement disorders clinic revealed generalized asymmetrical dystonia with major involvement of the left hemibody. In the left upper limb, she showed supination and abduction with flexion of the metacarpophalangeal joints with extension of the interphalangeal joints. In the left lower limb, she exhibited toe curling and plantar flexion particularly exacerbated during walking. To a lesser extend, there was a metacarpophalangeal joint and wrist flexion in the right hand as well. Muscle stretch reflexes were slightly brisk in the right lower limb and left upper limb. There was evident jaw opening dystonia with pulling of the lower face, with no marked tongue movements, as well as no significant upper facial involvement. Her genetic testing revealed a pathogenic variant in the THAP1 gene (c.305dup [p.Pro103Thrfs * 11]).
Several pharmacotherapeutic interventions failed to reduce her symptoms, including levodopa, trihexyphenidyl, tetrabenazine, and baclofen. Botulinum neurotoxin (BoNT) injections were applied mainly for jaw opening and cervical dystonia. By the age of 24, the patient underwent bilateral globus pallidus internus (GPi) DBS implantation. The scores of her Burke–Fahn–Marsden Dystonia Rating Scale (BFMDRS) improved from 25 to 5 following her surgery. Her functional ability improved significantly a few months into the surgery and she continued lower dose treatments with BoNT for jaw-opening dystonia.
Her first pregnancy was at the age of 32 with the following DBS setting; Left GPi-DBS 4 + 3- 90 ms 139 Hz 2.1 mA; Right GPi-DBS C + 11-90 ms, 139 Hz, 2.1 mA. During her visit to the movement disorders clinic while in the first trimester of her pregnancy, she reported suffering tinnitus in her left ear. She turned her DBS off noticing an immediate and complete resolution of this symptom. Furthermore, she did not experience any return or rebound in her dystonia, and hence, decided to be off DBS stimulation throughout pregnancy. In the second trimester of pregnancy, she restarted treatment with BoNT for jaw dystonia, the only symptom that had not responded to DBS in the past. Delivery occurred at full term by 37 weeks’ gestation, through planned cesarian section, in which she received epidural anesthesia. She reported no further increase in her dystonia before, during, or after delivery and her baby was delivered safely with no complications. After delivery, the DBS was turned on without complications or recurrence of tinnitus.
The currently limited available reports suggest that pregnancy is generally safe in the case of generalized dystonia. In addition, those cases of monogenic dystonia and in situ DBS implantation do experience an overall good outcome (Table 1). Reference Ziman, Coleman and Starr8 Still, these cases, may present a great challenge for health care providers. In part, this attributed to the fact that patients may experience worsening of their symptoms during stressful event such as delivery. Moreover, avoidance and/or reduction of medical treatment, and botulinum toxin also affect the severity of dystonia.
Table 1: Pregnancy outcomes for patients on DBS
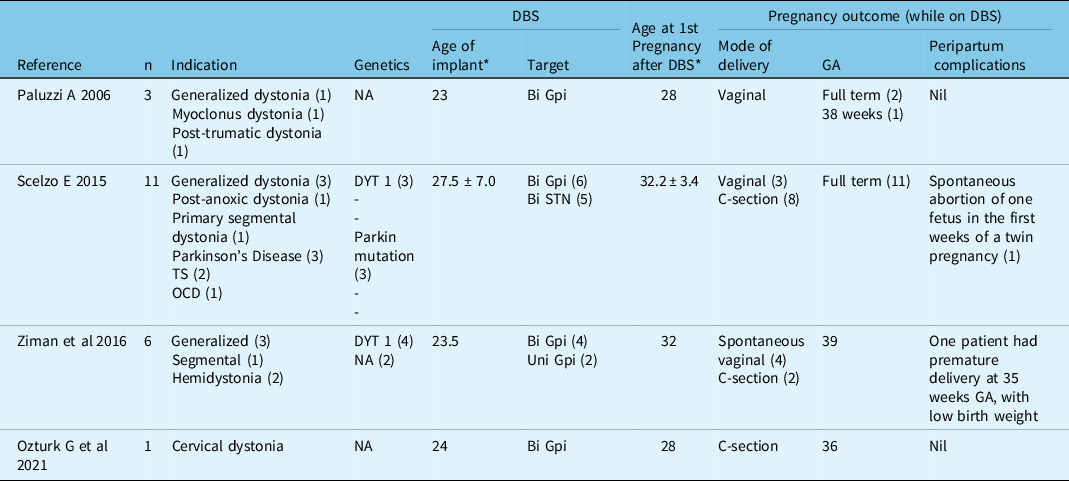
GA: Gestational age; *median.
This report supports previously published cases addressing the safety of pregnancy and delivery outcomes in the case of monogenic generalized dystonia. Additionally, we also provide evidence of a similar favorable outcome despite prolonged DBS discontinuation throughout pregnancy.



