Injuries to the brachial plexus significantly impair the daily activities of patients. With the development of microsurgical techniques several varieties of nerve transfer surgery are increasingly being performed. The outcome at follow-up, however, is different depending on the donor nerve. Therefore the treatment of total brachial plexus avulsion remains a significant challenge. The phrenic nerveReference Gu, Wu and Zhen 1 , Reference Liu, Lao, Gao, Gu and Zhao 2 and the contralateral C7 nerve rootReference Gu, Zhang, Chen, Yan, Cheng and Chen 3 , Reference Gao, Lao, Zhao and Gu 4 are the most commonly used donor nerves in the treatment of total brachial plexus avulsion. To date, however, no studies have investigated which of the two nerves is better for nerve transfer surgery. The aim of this study was to determine which of the two donor nerves yields a superior outcome for nerve transfer in the treatment of total brachial plexus avulsion.
METHODS
Animals and Grouping
A total of 60 healthy adult male Sprague-Dawley rats weighing between 230 and 250 grams were randomly assigned to 1 of 3 groups. We defined the radial nerve without the triceps branch as the antebrachial branch. In Group A the full-length phrenic nerve was harvested through open chest surgery and transferred to the radial nerve antebrachial branch at the level of latissimus dorsi insertion (Figure 1). In Group B the contralateral C7 nerve root was transferred to the radial nerve antebrachial branch at the level of latissimus dorsi insertion, with an ulnar nerve bridge (Figure 2). In Group C the antebrachial branch of the radial nerve was cut at the same level and directly sutured. All rats were maintained under standard conditions (temperature 25°C) with food and water. All surgical procedures were in compliance with Chinese Animal Protection Guidelines. All investigations involving animals were approved by the Animal Research Committee, Shanghai Medical College, Fudan University.
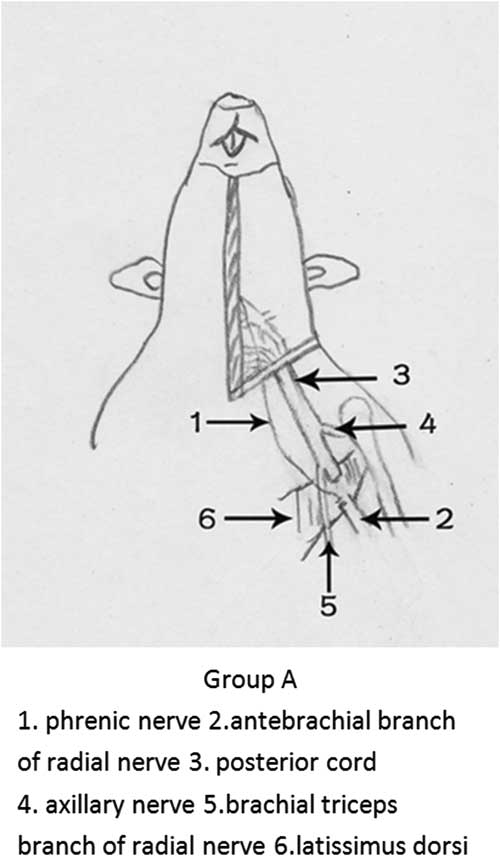
Figure 1 Diagrammatic presentation of surgery in Group A.
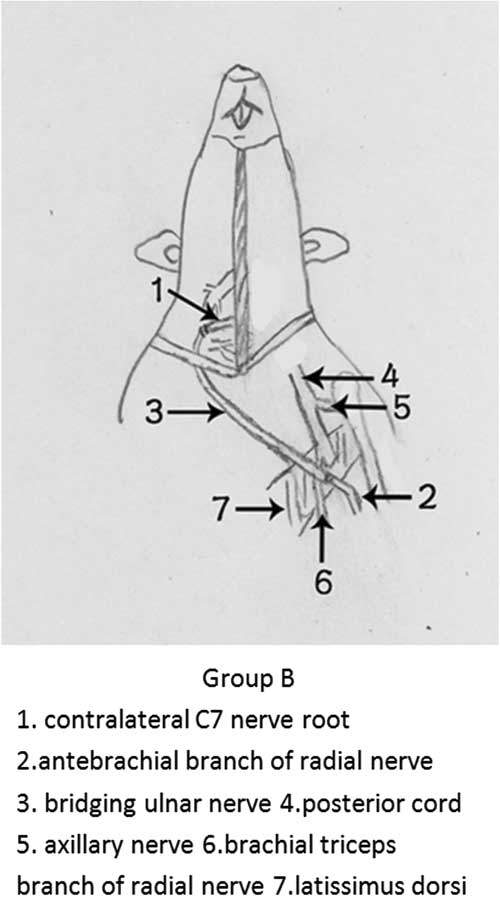
Figure 2 Diagrammatic presentation of surgery in Group B.
Surgery
The rats were injected with pentobarbital (40 mg/kg body weight, intraperitoneally) and then prepped and draped. The surgery was performed in the supine position. All procedures were performed under a microscope at 10× magnification.
In Group A the pectoralis major muscle, 2-6 ribs and the intercostal muscles were cut and the chest cavity was opened to expose the phrenic nerve at the level of the diaphragm insertion on the left side. The phrenic nerve was cut at the level of diaphragm insertion and freed to the level of the first rib. The phrenic nerve was pulled to the brachial plexus at the axilla through the second intercostal space. The brachial triceps branch of the radial nerve was exposed and retrogradely separated, and the remainder of the radial nerve was defined as the antebrachial branch. The antebrachial branch of the radial nerve was cut at the level of latissimus dorsi insertion. The phrenic nerve was sutured to the distal stump of the antebrachial branch with end-to-end neurorrhaphy using a 12-0 microstitch. The ulnar nerve was cut at the same level and embedded into the pectoralis major.
In Group B a cervical incision was made on the right side and the C7 nerve root was exposed. The antebrachial branch was exposed and protected using the same method as in Group A. The contralateral C7 nerve root was sutured to the distal stump of the antebrachial branch with end-to-end neurorrhaphy using a 12-0 microstitch, with a 4.5 cm length ulnar nerve bridge, which was harvested on the left side.
In Group C the antebrachial branch was exposed and cut using the same method as the other two groups. The antebrachial branch was sutured directly with end-to-end neurorrhaphy using a 12-0 microstitch. The ulnar nerve was also cut at the level of latissimus dorsi insertion and embedded into the pectoralis major.
Behavioral Assessment
The behavioral assessment of the rats included their respiration, mode of crawling, the presence of ulceration and the time when the movement of the wrist and toe extension appeared. The behavioral assessment began from the first day after the operation and continued every day until the motion of wrist and toe extension appeared. After that point the animals’ behavior was assessed every 2 weeks.
Electrophysiology
The electrophysiological studies began 4 weeks after the operation and were repeated every 4 weeks. The rats were anesthetized before electrophysiological evaluation (Dantec-Neuromatic 2000, Italy). The stimulating electrode was gently placed on the antebrachial branch at the level of latissimus dorsi insertion. The recording electrode was placed over the extensor carpi ulnaris muscle, the extensor digitorum communis muscle and the extensor carpi radialis muscle. An electrical stimulus (amplitude 2.5 mA, duration 0.04 ms) was applied, and the latency and maximum amplitude of the compound muscle action potential (CMAP) were recorded. The latency delay rate and the amplitude recovery rate of the CMAP on the left side were expressed as a percentage of the results from the right side. The room temperature was maintained at 25°C.
Nerve Histology and Fiber Counting
Following the electrophysiological studies, specimens were obtained at 5 mm both proximal and distal to the nerve coaptation site in Group A and Group C. In Group B, specimens were taken from 5 mm proximal to the proximal coaptation site and 5 mm distal to the distal coaptation site. The specimens were fixed in 2.5% glutaraldehyde buffered with cacodylate, washed in sodium cacodylate buffer (0.2 mol/L, pH 7.4), and postfixed in 1% osmium tetroxide. The samples were then dehydrated and embedded in epon. A thickness of 0.5 μm was cut from the middle of the nerve samples and stained with toluidine blue. The cross-sections were examined under a light microscope (Leica DWLB2, Germany), and the number of myelinated fibers was counted for each specimen using a computerized image analysis system (QWin Histomorphometry System, Leica, Germany) at 400× magnification. The pass rate of the distal myelinated nerve fibers was expressed as a percentage of the number of proximal myelinated nerve fibers.
Muscle Weight and Histology
After the nerve specimens were taken (see above), the extensor carpi ulnaris muscles, extensor digitorum communis muscles and extensor carpi radialis muscles from both sides were cut from the muscle origins and insertions. The wet weights of the muscles were measured with an electronic scale with a precision of 0.0001 g. The recovery rate of the wet muscle weight on the left side was expressed as a percentage of the weight from the right side. The muscle samples were then fixed in 10% paraformaldehyde and washed in buffer. The samples were dehydrated in alcohol, embedded in paraffin, cross-sectioned at the thickness of 5 μm at the same position of the muscle belly, stained with hematoxylin-eosin and examined under a light microscope. The mean cross-sectional area of the muscle fibers was calculated. The recovery rate of the cross-sectional area on left side was expressed as a percentage of the area from the right side.
Data Analysis
The groups were compared using a two-way analysis of variance with SPSS 16.0 statistical software. The results are shown as the mean ± standard deviation. A p value <0.05 was regarded as a statistically significant difference.
RESULTS
Behavioral Assessment
The rats lost the function of wrist and toe extension due to the antebrachial branch. The rats in Group A experienced tachypnea due to the loss of the phrenic nerve on the surgical side; however none of the rats in this group died because of respiratory problems, nor were ulcerations discovered on the surgical side. Motion of the wrist and toe extension was identified in Group A between 19 to 27 days (average 22.6±3.32 days). The motion showed a similar rhythm as the respiratory rate and did not disappear under anesthesia. In contrast, the motion of the wrist and toe extension was observed in Group B between 53 to 63 days (average 57.2±2.98 days), which was significantly longer than Group A (p <0.05).
CMAP Maximum Amplitude Recovery Rate
The amplitude of the CMAPs of the extensor carpi ulnaris muscles, the extensor digitorum communis muscles and the extensor carpi radialis muscles initially decreased postoperatively and gradually recovered. The maximum amplitude recovery rate of the CMAP at 24 weeks postoperatively ranged from highest to lowest in Group C, Group B and Group A, respectively. The full results and statistical significance are shown in Table 1.
Table 1 CMAP Maximum Amplitude Recovery Rate 24 Weeks After Operation

%, mean ± SD, n=8
Values in parentheses = p compared with Group A; * = p <0.05
CMAP Latency Delay Rate
The CMAP latency of the extensor carpi ulnaris muscles, the extensor digitorum communis muscles and the extensor carpi radialis muscles gradually shortened after the surgery and ranged from lowest to highest in Group C, Group B and Group A, respectively, at 24 weeks postoperatively. However, there were no statistically significant differences between the groups (Table 2).
Table 2 CMAP Latency Delay Rate 24 Weeks After the Operation
%, mean ± SD, n=8
Values in parentheses = p compared with Group A
Number of Myelinated Nerve Fibers
The number of myelinated nerve fibers at the distal part of the nerve coaptation site ranged from highest to lowest in Group C, Group B and Group A, respectively, at 24 weeks postoperatively. There was no significant difference between Group C and Group B, while a statistically significant difference was found between Group A and the other two groups (Table 3).
Table 3 The Attributes of Myelinated Nerve Fibers 24 Weeks After Operation
Mean ± SD, n=8
Values in parentheses = p compared with Group A; * = p <0.05
Pass Rate of the Myelinated Nerve Fibers
At 24 weeks postoperatively the pass rate of the myelinated nerve fibers at the nerve coaptation site ranged from highest to lowest in Group C, Group A and Group B, respectively. The pass rate in Group B was significantly lower compared to the other two groups (Table 3).
Cross-sectional Area of the Myelinated Nerve Fibers
The cross-sectional area of the myelinated nerve fibers gradually recovered postoperatively. Significant differences were observed in the cross-sectional area of myelinated nerve fibers at the distal part of the nerve coaptation site and ranged from highest to lowest in Group C, Group B and Group A, respectively, at 24 weeks postoperatively (Table 3).
Muscle Wet Weight Recovery Rate
The wet weight of the forearm extensive muscles gradually recovered with time. At 24 weeks postoperatively, the wet weight recovery rate of the forearm extensive muscles ranged from highest to lowest in Group C, Group B and Group A, respectively. The recovery rate was significantly higher in Group B than in Group A (Table 4).
Table 4 Muscle Wet Weight Recover Rate 24 Weeks After Operation
%, mean ± SD; n(Group A,B) =10, n(Group C) =9
Values in parentheses = p compared with Group A; * = p <0.05
Cross-sectional Area Recovery Rate of the Muscle Fibers
The cross-sectional area of the muscle fibers gradually recovered with time and ranged from highest to lowest in Group C, Group B and Group A, respectively, at 24 weeks postoperatively. These results were significantly different between groups (Table 5).
Table 5 Cross-sectional Area Recover Rate of Muscle Fibers 24 Weeks After Operation
%, mean ± SD, n=10
Values in parentheses = p compared with Group A; * = p <0.05
DISCUSSION
The phrenic nerve and the contralateral C7 nerve root are the most commonly used donor nerves in total brachial plexus avulsion. The aim of our study was to identify which of these two donor nerves yields a superior outcome in the treatment of total brachial plexus avulsion. The outcome of nerve transfer to recover elbow flexion with either the phrenic nerveReference Liu, Lao and Zhao 5 or the contralateral C7 nerve rootReference Pan, Wei, Chen and Gu 6 to the musculocutaneous nerve is good, while the effect of nerve transfer to recover digital motion with either of the two donor nerves is less than ideal. A clear comparison can therefore be achieved by choosing the radial nerve or the median nerve as the recipient nerve. We chose the antebrachial branch because the radial nerve contains more motor nerve fibers than the median nerve.
As the results show, the postsurgical time to the motion of the wrist and toe extension in Group B was longer compared to Group A. The earlier recovery time observed with the phrenic nerve as the donor nerve compared to the contralateral C7 nerve root was due to several advantages of the phrenic nerve. First, the phrenic nerve gives off spontaneous impulsesReference Gu and Ma 7 , Reference Zhang, Ma, Terenghi, Mantovani and Wiberg 8 with a high frequency and large amplitude, which can continuously stimulate nerve regeneration, while the C7 nerve root does not. Second, we obtained the full-length phrenic nerve through the exposed chest cavity in order to directly suture it to the antebrachial branch at the level of latissimus dorsi insertion using end-to-end nerve transfer. Therefore the nerve regeneration distance was shorter and the exacerbation of muscle atrophy could be controlled earlier. In contrast, the nerve regeneration using the contralateral C7 nerve root began from the contralateral supraclavicular region on the opposite side. As a result the nerve regeneration distance was significantly longer than the phrenic nerve.
Using the contralateral C7 nerve root as the donor nerve, however, resulted in improved functional recovery of the wrist and toe extension at 24 weeks postoperatively. This finding might be attributed to the difference in the number of donor nerve fibers between the two groups. As previously demonstrated, nerve transfer is more effective with more motor nerve fibers from the donor nerve. In addition, the number of phrenic nerve fibers is significantly lower compared to the number of nerve fibers in the contralateral C7 nerve rootReference Chen and Gu 9 . Although the pass rate of myelinated nerve fibers in Group A was higher compared to Group B, the absolute number of nerve regeneration fibers in Group A was still significantly lower compared to Group B. Therefore, using the contralateral C7 nerve root as donor nerve increased motor innervation.
In a previous study from our laboratory in a rat model, we showed that using the phrenic nerve as the donor nerve yielded a better outcome compared to using the ipsilateral C7 nerve root in an end-to-side neurotization, which is in contrast with the results from our current study.Reference Yang, Yang, Yu and Gu 10 One reason for this finding may be the advantages of the phrenic nerve discussed above. However, the absolute number of motor nerve fibers from donor nerves in nerve regeneration is more important in end-to-end neurorrhaphy compared to end-to-side neurotization.
It is important to note the limitation of our study, which was our use of an animal model, which may differ in the degree and mechanism of injury compared with humans. In particular, the obligatory conspicuous co-contraction of the opposite arm during volitional movements following nerve transfer with the contralateral C7 nerve root is not necessarily functionally disruptive in rats, while it significantly impairs the daily functioning of humans.
CONCLUSION
Our experimental results showed that the contralateral C7 nerve root yielded a superior outcome as the donor nerve for end-to-end nerve transfer in the treatment of total brachial plexus avulsion in a rat model.
Disclosures
Xiaotian Jia, Cong Yu, and Jianyun Yang do not have anything to disclose.
Statement of Authorship
Xiaotian Jia performed the experiments and wrote the manuscript. Cong Yu analyzed the data. Jianyun Yang conceived and designed the experiments.









