Background
Cervical spondylotic myelopathy (CSM) is a progressive degenerative disease and the most common cause of spinal cord dysfunction worldwide.Reference Nurick1 Its etiology is multifactorial and includes disc protrusion, ossification of the posterior longitudinal ligament, thickening of the ligamentum flavum and osteophyte formation, which result in narrowing of the spinal canal and ultimately lead to compression of the spinal cord.
Depending on the severity of the disease, symptoms can include neck pain, loss of hand dexterity, gait difficulties, and sphincter disturbance.Reference Fehlings, Wilson and Kopjar2–Reference Uomoto, Turner and Herron4 There are multiple scoring systems used to assess the severity of cervical myelopathy. The modified Japanese Orthopedic Association (mJOA) score is among the most commonly utilized and is a recommended outcome assessment tool for these patients.Reference Kalsi-Ryan, Singh and Massicotte5 According to this scoring system, mild myelopathy is defined as a score from 15 to 17, moderate from 12 to 14, and severe from 0 to 11.Reference Tetreault, Kopjar and Nouri6
Surgery is usually indicated to halt or reverse the myelopathic symptoms.Reference Houten and Cooper7, Reference McCormick, Steinmetz and Benzel8 The natural history of cervical myelopathy can be a progressive decline in neurological function in a significant proportion of patients.Reference Matz, Anderson and Holly9 Moreover, the severity of symptoms has been correlated to the likelihood of achieving a good clinical outcome with surgical decompression; patients with severe CSM are less likely to achieve a mJOA ≥16 with surgery.Reference Tetreault, Kopjar and Vaccaro10 Longer duration of symptoms has been correlated with poor surgical outcomes; Reference Tetreault, Wilson and Kotter11 therefore, prompt assessment and management are warranted to achieve better results for this patient population. In a public healthcare system, wait times to see a specialist from the time of referral (consultation wait time (CWT)) and wait times to receive surgical treatment from the time of surgical booking (surgical wait time (SWT)) can be substantial. With the increasing prevalence of CSM and the significant disease burden associated with spinal cord dysfunction for both the patients and society, it is essential to recognize factors that could be obstacles to timely management.
The primary objective of this study was to examine CWT and SWT in patients surgically assessed for CSM in the Canadian public healthcare system. Secondary objectives were to identify demographic, clinical, and radiographic factors that predict CWT and SWT in this same patient population and to compare wait times between CSM and other degenerative conditions of the spine.
Methods
Study Design
We conducted a multicentre, prospective observational study of consecutive patients with CSM enrolled in the CSORN between March 2015 and July 2017. CSORN is a group of over 50 neurosurgical and orthopedic spine surgeons from 18 tertiary care academic and non-academic hospitals across Canada that prospectively collect data on patients with spinal conditions. This database serves as a national registry created to answer research questions and to facilitate the implementation of best practices. Thirty-five surgeons from seven Canadian centers participated in this prospective CSM study.
A national database research coordinator audits data quality and performance and sends reports to each contributing hospital site coordinator on a quarterly basis. Reports track data completion and follow-up rates to facilitate internal data validation at each site. A national privacy and security framework was created for CSORN that includes a governance structure, standard operating procedures, training processes, physical and technical security, and privacy impact assessments. This model ensures privacy and security of personal health information. Written informed consent is obtained from all participating patients. Patient identification is anonymized to ensure that patients in the Network cannot be individually identified. All participating sites obtained Research Ethics Board (REB) approval prior to any data collection. Decisions regarding data collection, storage, and analysis are independent of any particular company or commercial interest.
Patient Sample
Local research coordinators enrolled patients at each site. All patients presenting to the participating surgeons with clinical signs and symptoms of CSM and MRI evidence of cord compression and/or myelopathy secondary to spondylosis were invited to participate in this study. To be included, patients also had to have referral and consultation dates available for CWT and surgical booking date and operative date for SWT. Further exclusion criteria included: previous cervical spine surgery, fracture, tumor or intradural pathology, anterior horn disease, or multiple sclerosis
Patient Variables
Baseline pre-operative patient characteristics included socio-demographic factors (age, sex, body mass index (BMI), nicotine use, education level, work status, and marital status), symptom duration, and the physical component score (PCS) of SF-12. All patients were treated in a single payer, publically administered healthcare system. These patients were stratified by CWT, SWT, as well as by the severity of the symptoms based on mJOA score. CWT was defined from the referral date to the first surgical consultation date and SWT was defined from surgical booking to the actual surgical date. Categorical data were compared using the Chi-square two-tailed tests. For demographic comparisons between wait time groups, statistical significance was achieved with a p-value of less than 0.05. Survival analysis was used for identification of independent predictors of CWT and SWT within the nationwide registry.
Using the CSORN database, a comparison cohort of lumbar stenosis patients enrolled during the same study period (March 2015 and July 2017) was used to contrast CSM and stenosis wait times.
Statistical Analysis
Outcomes were assessed using survival analysis. As a preliminary analysis to compare differences in survival across groups, the Kaplan–Meier (KM) method was used to estimate the survivor function of cumulative time waiting for consultation/surgery. Since not every referred patient was treated surgically, separate analyses were conducted for CWT and SWT.
Cox regression procedures were employed to find the best multivariable models predicting CWT and SWT outcomes. A data-splitting technique was used to develop and test the multivariable models. Data splitting is a method of obtaining a nearly unbiased internal assessment of accuracy. With this technique, an 80% random sample of the full data set was used for model development (BUILD sample) and the entire data set for validation (TEST sample).
Multivariable analyses were performed on the BUILD sample to identify the statistically significant variables, using a backward stepwise selection procedure. CollettReference Collett12 suggests avoiding rigid application of a particular significance level with this selection procedure. To guide decisions on entering and omitting terms, the significance level should not be too small; the significance level was set at the recommended level of 10%.
There were 22 potential predictors entered into regression models in clusters. The first cluster was primarily demographic-type variables: age, gender, BMI, marital status, living arrangement, education level, smoking status, exercise, and comorbidity. The second cluster was clinical variables: symptom duration, numeric pain rating, medication use, medication duration, intensity, and alignment. The third cluster was patient reported questionnaires: Neck Disability Index, SF-12 (Mental Component Score (MCS) and PCS, PHQ-9, EQ-5D, and mJOA.
All significant variables from the cluster modeling procedures were then entered into a multivariable model to determine the best models predicting outcome using the same selection procedure and significance levels. This combined analysis of multiple clusters/predictors has been previously shown to enhance the prediction of persistent pain.Reference Hasenbring, Marienfeld, Kuhlendahl and Soyka13, Reference Sampath, Bendebba, Davis and Ducker14 The outcome variables were cumulative number of calendar days waiting for consultation (CWT) and waiting for surgery (SWT). Adjusted R-squared values were computed for each final regression model. R-squared in survival analysis does not describe how appropriately a model fits the data because R-squared can be increased just increasing the number of variables. As a result, R-squared in this context examines the percentage of explained variation in the regression models.
Kaplan–Meier log rank tests were conducted to compare CWT and SWT in patients with CSM to lumbar stenosis patients entered into the CSORN database.
Results
Since not every referred patient was treated surgically, descriptive results are reported separately for CWT and SWT. Table 1 displays demographic data for both CWT and SWT. No statistical difference between provinces was found for either CWT or SWT. A total of 80 (CWT) and 124 (SWT) patients were excluded from analysis because the primary outcome was not obtained.
Table 1: Demographic data for patients with CSM from the CSORN registry as stratified by CWT and SWT

Consultation Wait Time
Data from 264 patients were available for analysis. The median CWT was 46 days. There were 31% mild (median CWT = 40), 35% moderate (median CWT = 60), and 33% severe CSM (median CWT = 32) based on mJOA scores. Kaplan–Meier log rank tests revealed no statistically significant difference in median CWT between mild and moderate group or mild and severe group. There was, however, a statistically significant difference (p <0.011) in CWT between the moderate and severe groups (Figure 1).
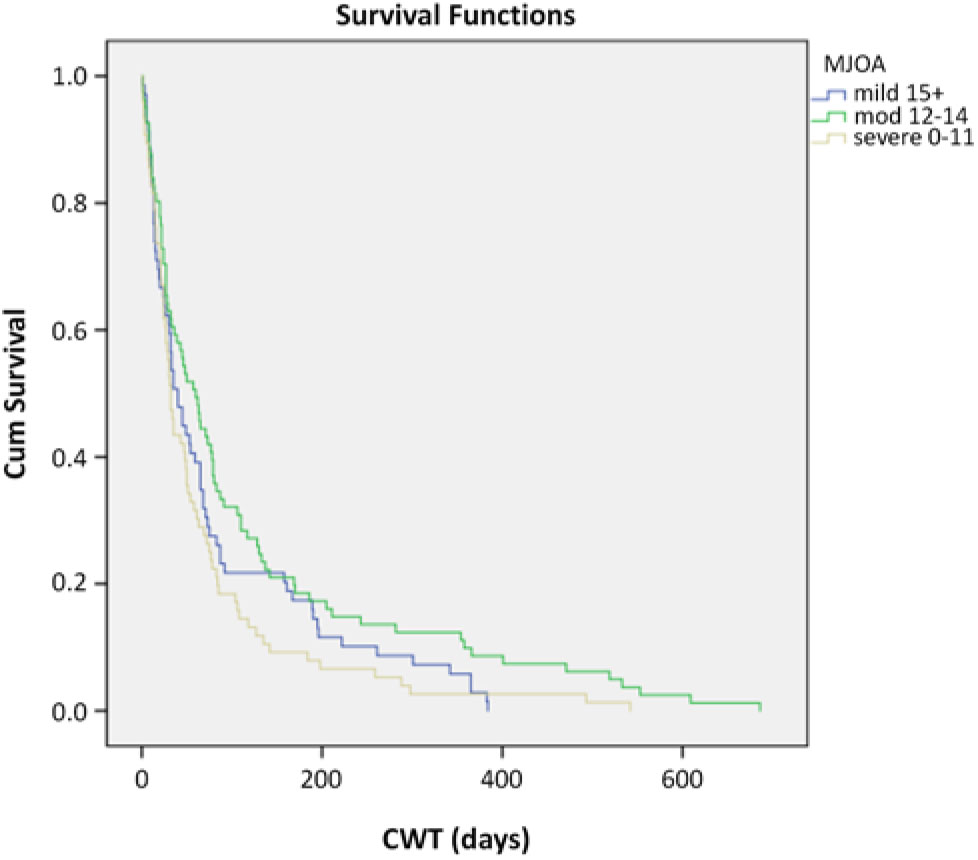
Figure 1: CWT Kaplan–Meier survival curves stratified by disease severity.
Multivariable Modeling
Using the build sample, multivariable regression analysis revealed five significant predictors of shorter CWT: short symptom duration (p <0.0001), less baseline neck pain (p <0.011), radiologic cord compression (p <0.059), lower BMI (p <0.023), and lower PCS scores (p <0.106) (Table 2). A separate regression analysis using the test sample confirmed the same five predictors. Overall, the model explained 18% of the variance (adjusted R-squared = 0.18).
Table 2: Regression analysis of predictors of CWT

HRR = hazard rate ratio, CI = confidence interval, and PCS = Physical Component Score of the SF-12.
Surgical Wait Time
Two hundred and seven patients underwent surgery and were included in the SWT analyses. The median SWT was 42 days. There were 25% mild (median SWT = 54), 40% moderate (median SWT = 43), and 35% severe CSM (median SWT = 24) based on mJOA scores. Kaplan–Meier log rank tests revealed a statistically significant difference in median SWT between mild and severe groups (p <0.005) and between moderate and severe groups (p <0.017). There was no statistically significant difference between mild and moderate groups (Figure 2).
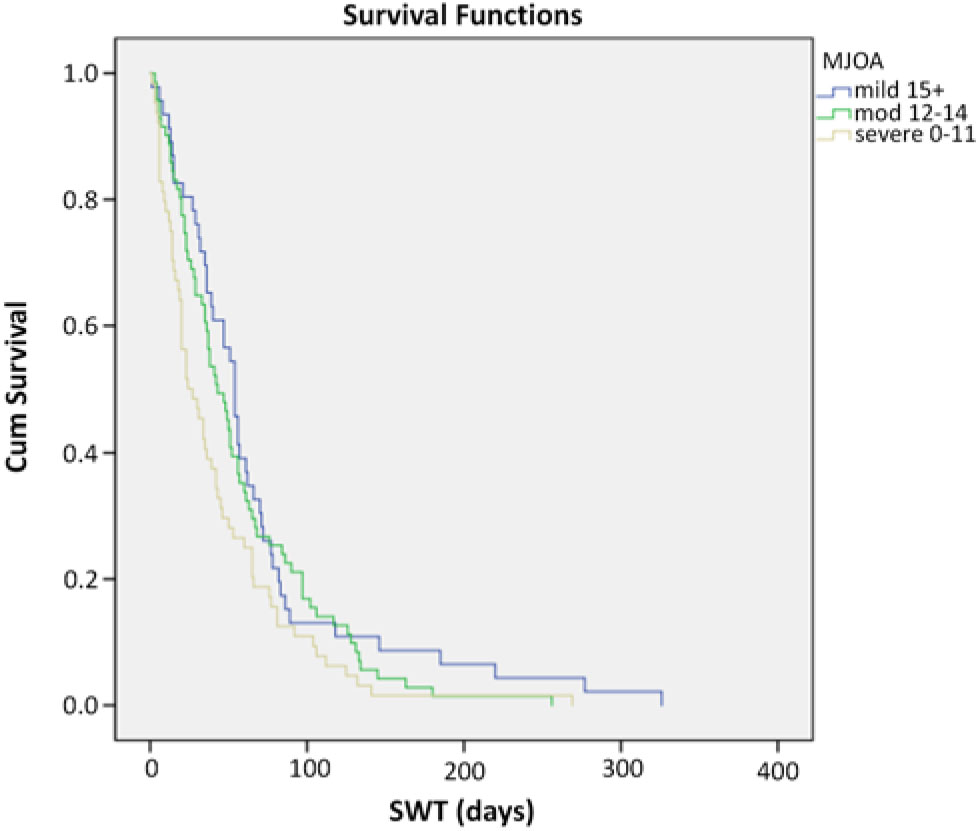
Figure 2: SWT Kaplan–Meier survival curves stratified by disease severity.
Multivariable Modeling
Using the build sample, multivariable regression analysis revealed only two significant predictors of shorter SWT: medication duration of less than 1 year (p <0.002) and less baseline neck pain rating (p <0.083) (Table 3). A separate regression analysis using the test sample confirmed the same two predictors. Overall, the model explained 11% of the variance (R-squared = 0.11).
Table 3: Regression analysis of predictors of SWT
HRR = hazard rate ratio and CI = confidence interval.
CSM and Lumbar Stenosis Comparison
A query of the CSORN database returned a total of 2799 patients who were surgically treated for lumbar stenosis. Their median CWT was 82 days compared to 46 days for CSM. The median SWT was 69 days for lumbar stenosis compared to 42 days for CSM. Kaplan–Meier log rank tests revealed that both CWT and SWT were significantly shorter in CSM group compared to spinal stenosis group (p <0.001).
Discussion
To our knowledge, this is the first study to investigate wait times and predictors in patients with CSM. In a public healthcare system such as the Canadian one, knowing the estimated wait time from referral to seeing a spine surgeon and from assessment to surgical treatment is necessary information to assist in quality improvement strategies.
In this study, patients with severe myelopathy waited less than patients with moderate symptoms to see a spine specialist and waited less than the moderate and mild groups to have surgery; however, mJOA on its own was not a significant predictor of wait times. There was no difference between the severe and mild groups for CWT. Two explanations are that our study may have been underpowered to detect a significant difference between each severity category or that the impact of the severity of the disease is indeed more pronounced on SWT than on CWT. Severity of symptoms may be better assessed by a surgeon, and hence the assessment has more impact on SWT. Disease severity may moreover not always be well communicated between referring doctors and surgeons, explaining less impact on CWT. The referral and prioritization mechanisms currently in place do work to some extent, but good communication between referring doctors and spine specialists cannot not be overemphasized. Improving the referral pathway for patients before they become severe would improve healthcare outcomes.Reference Tetreault, Kopjar and Vaccaro10, Reference Tetreault, Wilson and Kotter11 Increased awareness and continuous medical education of this common problem are part of the solution.
The other predictors of a shorter CWT were short symptom duration at time of referral, less neck pain, cord compression, lower BMI, and lower PCSs. Predictors of shorter SWT, on the other hand, only included short medication duration and less neck pain. Patients with more chronic findings and longer duration of symptoms had to wait longer to receive either consultation or surgical treatment. The rationale for this may be based on the knowledge that duration of symptoms has been shown to have a negative effect on surgical CSM outcomes.Reference Tetreault, Kopjar and Vaccaro10, Reference Tetreault, Wilson and Kotter11 Subacute CSM patients are often seen and offered treatment in an expedited fashion, thereby prioritizing patients with the best chance of improvement.Reference Tetreault, Kopjar and Vaccaro10, Reference Tetreault, Wilson and Kotter11 The other findings reflect that surgeons are less likely to see and operate rapidly on patients with severe neck pain.
Both CWT and SWT were significantly shorter in CSM compared to lumbar stenosis, which was expected. Our findings suggest that clinically appropriate prioritization schemes have been established at the participating centers. Patients with myelopathy, who have a higher likelihood of deterioration and with potential increased morbidity from delayed management, are treated faster than patients with lumbar stenosis.
The median CWT and SWT in this study were 46 and 42 days, respectively. We were unable to identify published data from other healthcare systems for comparison. Considering the potential clinical deterioration over time and the fact that patients with longer duration of symptoms and more severe disease have worse outcomes, time does matter in CSM. It is critical that CSM be diagnosed promptly, referred and managed in an expedient manner. A delay of close to 3 months from initial referral to definitive treatment may be suboptimal.Reference Tetreault, Kopjar and Vaccaro10, Reference Tetreault, Wilson and Kotter11 The length of the wait is an incentive to overcome the obstacles to expedited care. Improving communication and improved referral screening strategies are central to improving CWT. Imaging review by the spinal surgeon, rapid access clinics, and physiotherapist triage clinics are all potential improvement strategies that could improve CWT and needs to be studied further in this population. On the other hand, multiple factors are potential barriers to expedited surgical treatment. Access to semi-urgent operative time, case sharing among surgeons and proactive waitlist management are all part of dealing with limited resources, a problem commonly cited by surgeons to explain increased SWT. Surgery for CSM has been shown to be cost-effective while spinal cord impairment is associated with significant cost and productivity loss.Reference Tetreault, Karpova and Fehlings15 A combined effort by physicians and funders to increase expedited definitive care for these patients is justified and should be the focus of further study.
One limitation of this study is a lack of generalizability to other healthcare systems; however, the homogeneity of the Canadian healthcare structure increases the validity of these results for any single payer system. Moreover, no difference between provinces was found for both CWT and SWT reinforcing the homogeneity of this healthcare system. Although we acknowledge different referral schemes within Canada, the goal of this paper was not to compare pathway systems, but to define CWT and SWT and potential predictors in Canada and give incentives for improvement for this time-sensitive pathology. Interestingly, however, different screening strategies among different provinces did not impact CWT in this population. We did not establish a correlation between wait times and patient outcomes; our goal was to analyse predictors of shorter wait times. Lastly, we did not address two other potentially significant contributors: the time from symptom onset to first medical assessment and the time taken by primary care physicians to initiate consultation. Physicians will often request different investigations (imaging, nerve conduction studies) prior to making referrals. This “diagnostic” wait time has the potential to be long but needs to be kept to a minimum.
Conclusion
In this study, symptom severity had an impact on consultation and SWT in patients with cervical myelopathy. Patients with shorter duration (either symptoms or medication) and less neck pain had shorter waits to see a spine specialist in Canada and to undergo surgical treatment. This study highlights some of the obstacles to expedited care in this patient population. Process improvement strategies should be deployed to optimize outcomes in a population of patients in whom time matters.
Acknowledgements
The authors thank all of the subjects who participated in the study and the support/research coordinator staff and investigators from the CSORN contributing sites: Foothills Medical Centre, Winnipeg Health Sciences Centre, Vancouver General Hospital, Victoria Hospital – London Health Sciences Centre, Queen Elizabeth II – Halifax Sciences Centre Neurology, Hopital de L’enfant Jesus, and University of Alberta hospital site.
Conflict of Interest
Dr. Fisher reports personal fees from Medtronic, personal fees from Nuvasive, grants from AOSpine, grants from Medtronic, and grants from OREF, outside the submitted work. Dr. Dea reports personal fees from Stryker, personal fees from Medtronic, and personal fees from Baxter, outside the submitted work. Dr. Johnson reports grants from Stryker, outside the submitted work. Dr. Rampersaud reports personal fees from Medtronic, during the conduct of the study and personal fees from Medtronic, outside the submitted work. Dr. Jacobs reports personal fees from Stryker and personal fees from Medtronic, outside the submitted work. Dr. Manson reports grants from Medtronic Canada and personal fees from Medtronic Canada, outside the submitted work. Dr. Christie reports personal fees from Medtronic Canada, grants from Medtronic Canada, and grants from Rick Hanson Institute, outside the submitted work. Dr. Manson reports grants from Medtronic Canada and personal fees from Medtronic Canada, outside the submitted work. All other authors have nothing to disclose.
Statement of Authorship
BS: concept and design, analysis and interpretation of data, drafting the manuscript, and critical revision of the manuscript. CF: concept and design, acquisition of data, analysis and interpretation of data, drafting the manuscript, critical revision of the manuscript, and supervision. WBJ: concept and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript. MJ: concept and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript. CSB: concept and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript. SC: concept and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript. RC-M: concept and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript. JP: concept and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript. AN: concept and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript. DC: concept and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript. NM: concept and design, analysis and interpretation of data, and critical revision of the manuscript. HH: concept and design, analysis and interpretation of data, and critical revision of the manuscript. KCT: concept and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript. YRR: concept and design, analysis and interpretation of data, and critical revision of the manuscript. GM: concept and design, analysis and interpretation of data, drafting the manuscript, critical revision of the manuscript, and statistical analysis. ND: concept and design, acquisition of data, analysis and interpretation of data, drafting the manuscript, critical revision of the manuscript, and supervision.