Background
Approximately 20% of ischemic strokes involve the posterior circulation and 10%–15% of spontaneous intracerebral hemorrhage (ICH) affects primarily the brainstem or cerebellum. Reference Sparaco, Ciolli and Zini1,Reference Cordonnier, Demchuk, Ziai and Anderson2 With large infratentorial ischemic or hemorrhagic strokes, parenchymal damage and increasing mass effect cause brainstem dysfunction. In the most severe cases, patients may (in the absence of confounding factors) develop deep unresponsive coma with loss of any motor response to painful stimuli, absence of all cranial nerve reflexes, and apnea, such that they may meet criteria for neurological determination of death (NDD).
Countries across the world differ in whether they conceptually define death by neurological criteria based on permanent loss of brainstem function (previously referred to as ‘brainstem death’) or ‘whole brain death’. Reference Wijdicks3–Reference Greer, Shemie and Lewis5 When the cause of death is supratentorial injury, impaired brainstem function generally occurs in a rostral to caudal direction due to downward herniation, such that the above terms are essentially synonymous. In contrast, with posterior fossa mass lesions, coma and brainstem dysfunction precede supratentorial damage. It is therefore conceivable for patients to meet clinical criteria for NDD, at least transiently, while still having preserved cerebral blood flow (CBF) and potentially some supratentorial function. Consequently, the recent World Brain Death project recommends that in regions utilizing a “whole brain death” definition, as in the United States, “ancillary testing should be performed” and “brain death/death by neurological criteria should not be diagnosed until supratentorial/infratentorial blood flow is lost, even if the clinical examination and apnea test are suggestive”. Reference Greer, Shemie and Lewis5
Canadian guidelines state that “NDD may occur as a consequence of … primary direct brainstem injury,” but also assert that “distinctions between brainstem death (United Kingdom definition) and whole brain death (United States definition) are unclear in Canada”. Reference Shemie, Doig and Dickens6 This ambiguity may contribute to variability in physicians’ perceptions about the need for ancillary testing when the cause of potential death by neurological criteria is an infratentorial process. There are limited data assessing the incidence of this scenario, how clinicians manage it, and what ancillary testing most often shows when it is performed.
We therefore assessed consecutive critically ill patients that died of ischemic stroke or ICH in our region, focusing specifically on those with infratentorial involvement. Our primary goals were to determine the incidence and proportion of patients with infratentorial strokes that died and met clinical criteria for NDD, describe clinicians’ use of ancillary testing in this situation, and, when performed, assess whether ancillary testing was consistent with a diagnosis of “whole brain death” in demonstrating the absence of blood flow to the brain.
Methods
The study was approved by the Conjoint Health Research Ethics Board at the University of Calgary.
This was a retrospective, population-based, multicenter cohort study involving consecutive patients that died of ischemic stroke or ICH in an intensive care unit (ICU) in Alberta between January 1, 2013 and December 31, 2019. There are 19 adult ICUs in Alberta, all of which utilize a common clinical information system (Meta Vision, iMDsoft, Tel Aviv) and database. For every patient, the attending critical care physician prospectively documents the admission diagnosis. For patients that die, the attending physician must record whether clinical criteria for NDD were met and ancillary testing was performed.
Inclusion criteria for our study were age ≥18 years, an admission diagnosis of either ischemic stroke or ICH, and death in the ICU. From this larger cohort, we selected the subgroup of patients that appeared to meet clinical criteria for NDD. Neuroimaging and medical records were reviewed by a neurocritical care physician (AK) to categorize strokes as having primarily a supratentorial or infratentorial location (based on the most affected area or where ICH was thought to have originated), and to identify patients whose last documented neurological examination demonstrated a Glasgow Coma Scale (GCS) score of 3 (no eye opening, verbal response, or motor response), midposition or dilated nonreactive pupils, loss of all other cranial nerve reflexes, and no evidence of spontaneous respiration.
Confirmation of NDD by clinical examination alone requires an apnea test demonstrating the absence of respiration despite worsening respiratory acidosis (pH ≤ 7.28, PCO2 > 60, and PCO2 increment ≥ 20 mmHg). Reference Greer, Shemie and Lewis5,Reference Shemie, Doig and Dickens6 However, physicians sometimes forego a full apnea test when patients are too unstable to be disconnected from mechanical ventilation for several minutes or there are confounding factors that could interfere with respiratory effort (e.g. recent use of sedatives or opiates), or it is not possible to complete the minimum clinical examination (e.g. ocular trauma or other reasons for impaired cranial nerve reflexes). It is also possible that some clinicians view ancillary testing as being necessary to demonstrate “whole brain death” in the context of infratentorial mass lesions, and regard a full apnea test as being unnecessary when ancillary testing has been performed. Therefore, patients that appeared to meet clinical criteria for NDD, but did not undergo full apnea testing, were still categorized as potential NDD cases. Consistent with Canadian and international guidelines, ancillary tests that are used to establish NDD in Alberta may include radionuclide imaging or a digital subtraction angiogram. Reference Greer, Shemie and Lewis5,Reference Shemie, Doig and Dickens6 Radionuclide scans are obtained using diffusible, brain-specific radiotracers, either Tc99m hydroxymethyl-propylene-amine-oxime or Tc99m ethylene cysteine diethyl. Both dynamic and delayed static images are routinely displayed with multiple planar views (anterior, posterior, and lateral), consistent with recommendations of the Society of Nuclear Medicine and American College of Radiology. Reference Zuckier and Kolano7
Our primary outcomes were the incidence and proportion of deceased patients with infratentorial stroke that were confirmed or suspected (in cases where a full apnea test was not performed) to meet clinical criteria for NDD; the proportion of patients with confirmed or suspected NDD that underwent ancillary testing; and the proportion with ancillary testing that had preserved CBF. Secondary aims were to compare findings of ancillary testing between patients with supra- vs. infratentorial stroke and to describe corresponding intracranial pressure (ICP) and cerebral perfusion pressure (CPP) values among patients with suspected NDD in whom it was recorded. Our database also records hourly GCS scores and pupillary light reactivity; this enabled us to determine the time interval between documentation of a GCS score of 3 with bilateral absence of pupillary light reflexes and completion of an ancillary test.
Continuous variables are presented as medians with interquartile ranges, with comparisons performed using Kruskal–Wallis tests. Categorical variables are presented as proportions, with comparisons performed using chi-square analysis or Fisher’s exact test, as appropriate. To assess incidence, we obtained the annual population of Alberta from the provincial government website. Statistical analysis was performed using SAS (Version 9.4, Cary, NC, USA).
Results
Description of Cohort
Between January 1, 2013 and December 31, 2019, there were 924 patients admitted to Alberta ICUs with a primary diagnosis of ischemic stroke or spontaneous ICH, of which 358 (39%) died, including 263 (73%) arising in a supratentorial and 95 (27%) in an infratentorial location (Figure 1; Table 1). NDD was suspected based on clinical examination in 77/358 (22%) deaths, including 61/263 (23%) with supratentorial and 16/95 (17%) with infratentorial stroke. Thus, there were 0.55 cases of infratentorial stroke suspected to meet criteria for NDD based on physical examination per million population per year.
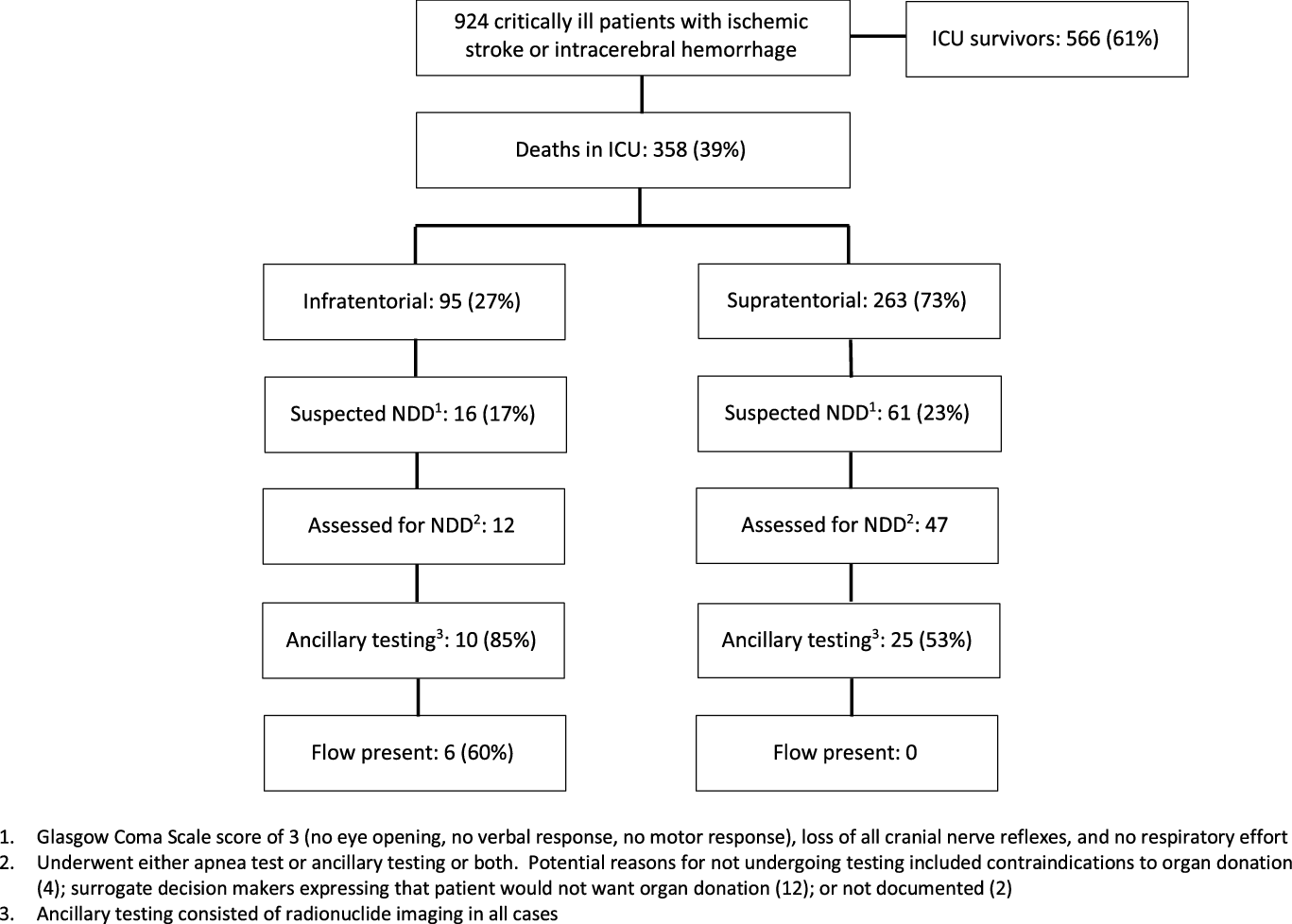
Figure 1: Flow chart describing consecutive patients with ischemic stroke or intracerebral hemorrhage admitted to intensive care units in Alberta, Canada 2013–2019.
Table 1: Characteristics of critically ill patients that died of ischemic stroke or intracerebral hemorrhage in Alberta 2013–2019

APACHE = acute physiology and chronic health evaluation; GCS = Glasgow Coma Scale; ICH = intracerebral hemorrhage; NDD = neurological determination of death.
Characteristics of patients that died of ischemic stroke or ICH are shown in Table 1. Suspected NDD was associated with younger age (56 (48–64) vs. 63 (55–72) year, p = 0.0001) and occurred more with ICH than ischemic stroke (54/195 (28%) vs. 23/163 (14%), p = 0.002). Among patients with suspected NDD, those with infratentorial stroke were significantly younger than those with supratentorial involvement (51 (34–56) vs. 58 (49–66) years, p = 0.02).
Findings of Ancillary Testing
Of the 77 patients with suspected NDD, 18 did not undergo complete testing with either an apnea test or ancillary test because surrogate decision makers were not in favor of organ donation (12/18), there were contraindications to organ donation (4/18), or for unclear reasons (2/18) (Figure 1). All of these patients underwent withdrawal of life-sustaining measures (WLSM) followed by rapid circulatory arrest, with no respiration observed following removal of the endotracheal tube in any of the patients.

Figure 2: Neuroimaging from a patient meeting clinical criteria for death by neurological criteria, but with preserved brain blood flow and perfusion. 52-year-old man with bilateral cerebellar infarcts. Unconfounded physical examination, including apnea test, completed by two physicians was consistent with death by neurological criteria. CT scan (far left) shows effacement of the basal cisterns and fourth ventricle, with enlarged temporal horns in keeping with hydrocephalus. Technetium-99 ECD radionuclide scan (second from left) shows reduced infratentorial, but preserved supratentorial radiotracer uptake. CT angiogram (second from right) shows normal opacification in anterior circulation. CT perfusion imaging (far right) showed lack of perfusion in most of the brainstem and cerebellum but preservation in the cerebral cortex.
There were 47 patients with supratentorial, and 12 patients with infratentorial stroke, that were assessed for NDD with either an apnea test, ancillary testing, or both (Figure 1). None of these patients underwent decompressive craniectomy. Use of ancillary testing was more common with infratentorial stroke (10/12 (85%) vs. 25/47 (53%), p = 0.045) and consisted of radionuclide imaging in all cases.
Among the 10/12 (85%) patients with infratentorial stroke that underwent radionuclide scans, 5/10 also completed a full apnea test (none of whom had evidence of respiration) prior to ancillary testing and 5/10 had apnea documented only with brief interruption of mechanical ventilation (Table 2). Only 2/10 patients that underwent ancillary testing were deemed too unstable to have an apnea test and none had documented confounding factors. CBF was present on both dynamic and static images in 6/10 (60%) cases, including 3/5 (60%) that underwent a full apnea test. In contrast, none of the 25 patients with supratentorial stroke that underwent ancillary testing had evidence of preserved intracranial flow (6/10 (60%) vs. 0/25 (0%); p = 0.0001). Neuroimaging from one representative case of infratentorial stroke is shown in Figure 2 (Patient 8 in Table 2).
Table 2: Summary of patients with neurological examination consistent with death by neurological criteria that underwent either apnea test, ancillary test (radionuclide scan), or both

CBF = cerebral blood flow; CPP = cerebral perfusion pressure (closest to time of CBF scan); F = female; ICH = intracerebral hemorrhage; ICP = intracranial pressure (closest to time of CBF scan); IS = ischemic stroke; M = male; N/A = not assessed.
1 External ventricular drain was removed 18 hours before radionuclide scan.
2 Repeat radionuclide scan was performed 72 hours, at which point there was no longer CBF. External ventricular drain removed 33 hours prior to second scan, at which time ICP was 43 mmHg and CPP 29 mmHg.
In 5/6 (83%) patients with infratentorial stroke and preserved CBF, radionuclide scans showed tracer uptake only in supratentorial brain. Two of these patients also had CT perfusion scans in close proximity to the radionuclide scan (Patients 8 and 10). In both cases, the CT perfusion demonstrated abnormal CBF, mean transit time, and cerebral blood volume in infratentorial regions, but normal results in supratentorial brain. In 1/6 (17%) patients, radiotracer uptake in the posterior fossa was abnormal but present. None of the families of the 6 patients in whom CBF was present were approached for consideration of NDD (heart-beating) organ donation.
The median time interval from first documentation of GCS 3 and absent pupillary light reflexes to completion of ancillary testing was 9 (5–13) hours among patients with preserved CBF, compared with 32.5 (21–40) hours in those with absent CBF (p = 0.04).
One patient with clinical suspicion of NDD but initially preserved CBF underwent repeat imaging 72 hours later, at which point there was no longer any flow (Patient 9).
Isolated Brainstem Stroke
Two patients with isolated brainstem stroke without cerebellar involvement met clinical criteria for NDD (Patients 6 and 12; Table 2). In both cases, there was extensive hemorrhage involving the midbrain, pons, and medulla, with extension into the fourth ventricle and obstructive hydrocephalus. Both patients underwent ancillary testing and CBF was present in one of them. In all other cases of infratentorial stroke evaluated for NDD, there was extrinsic compression of the brainstem.
ICP and CPP
An external ventricular drain (EVD) was present in 4/12 patients with infratentorial stroke that were assessed for NDD, allowing ICP and CPP to be measured (Table 2). In 2/4 patients in whom radionuclide scans showed absent CBF, the last available ICP was 106 mmHg (CPP 0 mmHg) (Patient 2) and 38 mmHg (CPP 42 mmHg) (Patient 7), respectively, although in the latter case the EVD was removed approximately 18 h prior to the scan. In 2/4 patients in whom radionuclide scans showed persistent CBF, ICP was 3 mmHg (CPP 80 mmHg) (Patient 4) and 23 mmHg (CPP 54 mmHg) (Patient 9), respectively. The latter patient was the one in whom there was no CBF on a repeat scan 72 hours later, at which time the EVD was no longer in situ, although the last documented ICP 33 hours prior to the scan was 43 mmHg (CPP 29 mmHg). In comparison, there were five patients with supratentorial stroke and NDD with EVDs, each of whom had markedly increased ICP (mean 79 mmHg; range 60–109 mmHg).
Discussion
This population-based, multicenter cohort study revealed clinical findings consistent with NDD in 17% of consecutive critically ill patients that died as a result of infratentorial ischemic or hemorrhagic stroke. The incidence of this scenario was just over 0.5 per million population per year. Thus, although uncommon overall, and accounting for only a small proportion of all potential NDD cases, it will still be encountered with some regularity at medical centers serving populations of several million people.
In some patients with infratentorial stroke, NDD was diagnosed exclusively based on clinical assessment, but in the majority, ancillary testing was performed. Use of ancillary testing was more common with infratentorial compared with supratentorial stroke. This suggests that there is variability in physicians’ acceptance of clinical assessments as being conclusive for NDD in the setting of posterior fossa lesions, which is also consistent with a recent survey showing that more than half of Canadian critical care physicians believe that ancillary testing should be performed under these circumstances. Reference Chasse, Briard and Yu8 This variability is likely influenced by the lack of clear direction in current Canadian guidelines and highlights the need for future consensus. Reference Shemie, Doig and Dickens6
Despite documentation of coma with no motor response to painful stimulation, the absence of all cranial nerve reflexes, and apnea, a majority of infratentorial stroke patients (60%) that underwent radionuclide scans had evidence of persistent blood flow to the brain. Normal blood flow was only present in supratentorial regions, while it was reduced or absent in the posterior fossa (Figure 2). In contrast, all patients with supratentorial strokes that underwent ancillary testing had globally absent flow. This finding confirms the unique considerations that exist with infratentorial stroke. Loss of brainstem function with preserved CBF in the setting of infratentorial lesions has been described in case reports and series, Reference Varelas, Brady and Rehman9 but has never previously been assessed in a multicenter, population-based study involving consecutive patients. There remains uncertainty about the degree to which preserved CBF and radiotracer uptake indicates meaningful neuronal perfusion and metabolic function, but flow-based studies remain the current standard for ancillary testing in cases of suspected death by neurological criteria. Reference Greer, Shemie and Lewis5,Reference Shemie, Doig and Dickens6
It is likely that, over time, at least some of our patients with initially preserved CBF would have progressed to loss of CBF, as in one of our cases where repeat radionuclide imaging was performed 72 hours later (Patient 9). Reference Varelas, Brady and Rehman9,Reference Hernandez-Hernandez, de Lucas and Munoz-Esteban10 This notion is supported by our observation that patients with absent CBF had a longer median time interval between documentation of a GCS score of 3 with loss of pupillary light reflexes and completion of the ancillary test. With incremental infratentorial mass effect, impaired cerebrospinal fluid circulation and venous outflow obstruction result in worsening hydrocephalus and cerebral edema, respectively, which in turn causes increasing supratentorial mass effect. Reference Marcellino, Braksick and Wijdicks11 However, no study has performed routine, serial imaging to demonstrate that progression to cerebral circulatory arrest invariably occurs in all cases of infratentorial stroke that have a physical examination consistent with death by neurological criteria.
Of the patients with ICP monitors that underwent radionuclide imaging, the presence of very high ICP was accompanied by the absence of CBF in all cases, while patients with relatively lower ICP (<20–25 mmHg) had persistent CBF. Thus, ICP monitoring may predict in advance whether ancillary testing will show loss of CBF. However, in most cases, there is no ICP monitor in situ and the timing of loss of CBF cannot be reliably determined by physical examination.
From a legal perspective, there is currently no federal statutory definition of death in Canada. In 1981, the Law Reform Commission of Canada recommended that Parliament enact a provision stating that “a person is dead when an irreversible cessation of all that person’s brain functions has occurred”. 12 While the language seems to imply a whole brain definition for death, this recommendation was never enacted into federal law. Similarly, in Manitoba, the Vital Statistics Act defines death as occurring “at the time at which irreversible cessation of all that person’s brain function occurs”. 12 In other provinces, when death will be followed by possible organ donation, legislation includes provisions that the determination of death should be made by two physicians in accordance with accepted medical practice.
The “dead donor rule,” namely that organs should not be removed until a potential donor is proven to have died, is considered an inviolable principal in deceased organ donation. Thus, consensus is needed regarding whether patients with infratentorial lesions, unresponsive coma, loss of cranial nerve reflexes, and a failed apnea test should be considered deceased or require ancillary testing to demonstrate cessation of intracranial blood flow. Despite persistent CBF, some have argued that because of permanent loss of consciousness and vital functions like respiration, as well as the expected loss of intracranial blood flow over time, this condition should still be regarded as death by neurological criteria. Reference Manara, Varelas and Wijdicks13 Conversely, recent research has highlighted the limitations of physical examination at detecting consciousness. Reference Edlow, Chatelle and Spencer14,Reference Claassen, Doyle and Matory15 Some have even argued that manifestations of “brainstem death” can conceivably occur with relative sparing of the reticular activating system. Reference Walter, Fernandez-Torre, Kirschstein and Laureys16 Indeed, there are case reports of electroencephalography showing alpha and theta activity in the context of apparent “brainstem death”. Reference Walter, Fernandez-Torre, Kirschstein and Laureys16
Practically, in cases where an unconfounded examination is consistent with death by neurological criteria, but patients are not eligible for organ donation, establishing NDD may not be essential, since the prognosis is invariably poor and WLSM is a common consensual, shared decision between clinicians and surrogate decision makers in Canada. This reasoning is reflected by numerous patients in our cohort where the attending physician suspected, but did not prove death by neurological criteria with an apnea test or ancillary test because either the family was not interested in pursuing organ donation or there were overt contraindications. An exception would be if there were reluctance on the part of surrogate decision makers to consider WLSM, in which case identification of death by neurological criteria would become more important. If there is a decision to proceed with organ donation, assessing for NDD (rather than proceeding with donation after circulatory determination of death) is crucial to maximize the number and quality of organs to be transplanted.
The strengths of our study consist of the population-based design, inclusion of consecutive patients, and large sample size. An important limitation is that not all patients with suspected death by neurological criteria underwent an apnea test; however, this reflects the reality of caring for patients with devastating brain injuries, where there are often potential confounding factors, physiological instability, or other reasons why clinicians may prefer to perform ancillary testing and forego an apnea test. Of note, none of the patients with suspected NDD in whom no apnea test was performed had evidence of respiration after WLSM, thereby further supporting the clinical impression.
In conclusion, patients with large infratentorial ischemic or hemorrhagic strokes may deteriorate to the point of meeting clinical criteria for NDD. This occurs with an annual incidence of about 0.55 cases per million population. There is variability amongst critical care physicians in the perceived need for ancillary testing under these circumstances to establish death by neurological criteria and Canadian consensus is needed. Intracranial blood flow is preserved in a sizable proportion of these patients (more than half in our cohort), at least in supratentorial regions and during the initial hours after loss of brainstem function.
Acknowledgements
The authors thank Dr. Sam Shemie for comments/suggestions regarding the manuscript.
Disclosures
Dr. Kramer is the Medical Director of the Southern Alberta Organ & Tissue Donation Program. Dr. Doig is the former Chair of the Donation Committee of the Canadian Council for Donation and Transplantation and was the Co-Lead of the Canadian NDD consensus panel. Dr. Chassé holds a CIHR grant to investigate use of CT perfusion scanning in NDD assessments. The remaining authors have no conflicts of interest to declare.
Statement of Authorship
AK conceived the study, performed the analyses, and wrote the manuscript. JK, CD, MC, PC contributed to the analysis and interpretation of data, and assisted in revising the manuscript.






