CLINICIAN’S CAPSULE
What is known about the topic?
Transport of STEMI patients directly to the cath lab (STEMI bypass) by advanced care paramedics (ACPs) is common practice. The safety of this practice with primary care paramedics (PCPs) is unknown.
What did this study ask?
What is the prevalence and breakdown of events during PCP STEMI bypass?
What did this study find?
Clinically important events are common in STEMI bypass patients. A smaller proportion of events would be addressed differently by ACP compared to PCP protocols.
Why does this study matter to clinicians?
This study adds to the evidence that PCP STEMI bypass is safe.
INTRODUCTION
Background
For patients presenting with an ST-elevation myocardial infarction (STEMI), every minute of delay increases ischemic time and mortality.Reference De Luca, Suryapranata, Ottervanger and Antman 1 Percutaneous coronary intervention (PCI) is the recommended method of reperfusion, providing it can be performed within 90 minutes of first medical contact.Reference O’Gara, Kushner and Ascheim 2 , Reference O’Connor, Al Ali and Brady 3 As per the American Heart Association (AHA) guidelines, STEMI patients should be transported by emergency medical services (EMS) to a PCI capable hospital when a door-to-balloon time of 90 minutes or less can be achieved.Reference O’Gara, Kushner and Ascheim 2 , Reference O’Connor, Al Ali and Brady 3
In eligible patients meeting prehospital criteria for PCI, it is recommended to transport patients directly to the PCI facility, bypassing closer emergency departments. This has been termed STEMI bypass.Reference O’Gara, Kushner and Ascheim 2 In Ottawa and many other jurisdictions, the EMS system is composed of primary care paramedics (PCPs) (analogous to Basic Life Support [BLS] medics) capable of defibrillation and basic interventions as well as advanced care paramedics (ACPs) capable of performing all Advanced Cardiac Life Support (ACLS) interventions (analogous to Advanced Life Support [ALS] medics). It is not always possible to have an ACP crew readily available to transport STEMI patients to a PCI centre; insisting this were the case would lead to longer door-to-balloon times. Since 2005, Ottawa PCP crews have been transporting patients directly to the PCI centre. This “PCP STEMI Bypass” protocol may lead to prolonged PCP transport time, but faster access to PCI.
Importance
Fifty percent of deaths from acute coronary syndrome occur in a prehospital environment; however, this includes patients presenting in cardiac arrest prior to first medical contact.Reference O’Connor, Brady and Brooks 4 The exact mortality and instability of STEMI patients in the field are not entirely known nor what interventions STEMI patients may require en route to the PCI facility. Some studies have shown that clinically significant events are common, but it is unclear whether ALS interventions are frequently required, or whether an increased transport time has an impact.Reference Ryan, Craig, Turner and Verbeek 5 , Reference Ross, Alsayed and Turner 6 Two recent studies have been published in this journal examining PCP STEMI bypass.Reference Bussières, Bégin and Leblanc 7 , Reference Kwong, Ross and Turner 8 Bussières et al. looked at a PCP STEMI bypass in a rural setting in a PCP-only EMS system, whereas Kwong et al. evaluated a PCP STEMI bypass guideline in a dense urban environment with both PCP and ACP care. Our study adds to the existing literature examining the safety of a PCP STEMI bypass by examining its use in a different setting.
Goal of this investigation
The objective of this study was to investigate the safety of PCP-only STEMI bypass by examining the existing PCP-only STEMI bypass program in Ottawa. Specifically, we sought to determine the prevalence and categorize any clinically important events during transport and to determine the proportion of such events that could only be treated by ACP protocols.
METHODS
Study design and setting
We conducted a health record review of STEMI patients transported for primary PCI from January 1, 2011, to December 21, 2015. January 2011 was the date when electronic prehospital patient care reports replaced paper reports, and December 2015 was the start date of our study; therefore, all electronic available data were included. Ottawa has a single PCI facility located at an academic tertiary care centre. The prehospital system is composed of both PCPs capable of BLS and equipped with automated external defibrillators (AEDs) as well as ACPs capable of full ALS care. In some cases, an ACP crew will intercept a PCP crew either on scene or rendezvous during transport in a process termed ACP-intercept. This process can be initiated automatically by dispatch when an ACP-only transport crew is sent to relieve a PCP-only first response car (not capable of patient transport), or when a PCP-only crew calls for ACP backup.
Study population
We included STEMI patients presenting to the Ottawa Heart Institute for primary PCI after transport by the Ottawa Paramedic Service under a STEMI bypass agreement. Inclusion criteria for STEMI bypass include signs and symptoms of cardiac ischemia of ≤12 hours with a 12-lead electrocardiogram (ECG) showing ST-elevation ≥1 mm in at least two contiguous limb leads, or ST-elevation ≥2 mm in at least two contiguous pre-cordial leads. Exclusion criteria for STEMI bypass was a transport time to the catheterization laboratory of greater than 60 minutes since the STEMI-positive ECG.
Case identification and data collection
Our case identification strategy used the dispatch database to determine urgent transports to the Ottawa Heart Institute during the study period. From this, we derived the type of STEMI bypass (overall total, ACP-only, PCP-only, and ACP-intercept). We reviewed the prehospital electronic patient care report and hospital chart for PCP-only and ACP-intercept cases identified. Our study did conform to the RECORD statement of health record reviews.Reference Benchimol, Smeeth and Guttmann 9 We piloted a data extraction form which was used to manually extract patient and system characteristics, as well as the primary and secondary outcomes. This study was approved by the Ottawa Health Science Network Research Ethics Board.
Outcome measures
Our primary outcome was clinically important events occurring under the care of paramedics. We determined our definitions of clinically important events based on previous definitions in the literature,Reference Ryan, Craig, Turner and Verbeek 5 , Reference Ross, Alsayed and Turner 6 author consensus, and by ensuring they could be objectively extracted. Events included were hypotension (systolic blood pressure < 90), bradycardia (HR < 60), tachycardia (HR > 100), arrhythmias (supraventricular tachycardia, ventricular tachycardia, rapid atrial fibrillation, and third-degree heart block), decreased level of consciousness (Glasgow Coma Scale [GCS] < 15), need for airway support (positive pressure ventilation with a bag-valve mask, placement of oral or nasal pharyngeal airway, insertion of supraglottic airway or endotracheal intubation), and cardiac arrest (initial and subsequent rhythm, if defibrillation took place, and if return of spontaneous circulation [ROSC] was achieved). Using the paramedic protocols, the proportion of clinically important events that could only be treated by ACP protocols and not by PCP protocols, was determined by consensus between two independent investigators (SM, MA) who were blinded to the outcome data. A third investigator (RD) was used if consensus could not be reached by a unanimous agreement. Secondary outcomes were interventions performed during transport, prehospital mortality, in-hospital mortality during index visit, and rate of erroneous STEMI bypass (defined as a case deemed not to be a STEMI on arrival to cardiac catheterization laboratory).
Data analysis
We presented information on the prevalence of clinically important events and their description using descriptive statistics. Where appropriate, we reported differences in event proportions between PCP and ACP crews with 95% confidence intervals (CI) and chi-square statistics. We compared continuous variables using two-tailed t-test statistics.
RESULTS
Characteristics of study subjects
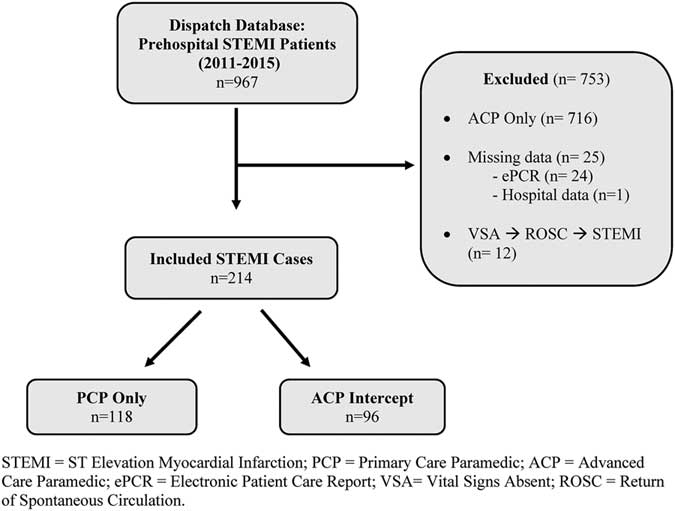
There were 967 STEMI bypass cases transported by the Ottawa Paramedic Service to primary PCI from January 1, 2011, to December 21, 2015 (Figure 1). Of these, 716 were ACP-only transports and therefore excluded. A further 37 cases were excluded (25 due to missing data, and 12 were calls for out-of-hospital cardiac arrest with a STEMI on ROSC ECG). This left 214 STEMI bypass cases that were included in the study: 118 PCP-only and 96 ACP-intercept.

Figure 1 Study flow diagram.
Overall patient and system characteristics for included cases are presented in Table 1. The mean age was 61.4 years (SD 13.37; range 23–94), and 78.0% of patients were male. The most common infarct locations were inferior (44.5%) followed by anterior (31.8%). Many patients had cardiac risk factors, the most common being hypertension (56.9%) and smoking (62.0%). Most patients were administered acetylsalicylic acid (ASA) by EMS (91.1%). Nitro was administered in 36.4% of patients and more commonly in the ACP-intercept group (47.9%) compared with the PCP-only group (27.1%) – difference of 20.8%, 95% CI 7.8–33.0; p=0.002.
Table 1 Patient and system characteristics
ACP=advanced care paramedic; ASA=acetylsalicylic acid; contact time=time interval from arrival to patient’s side to arrival to catheterization laboratory; erroneous STEMI bypass=no STEMI on arrival to catheterization laboratory; nitro=nitroglycerin spray; paramedic PCP contact time=time interval from PCP arrival on-scene to transfer of care to ACP; patch to base hospital=patch to emergency physician for online medical control; PCP=primary care paramedic; response time=time interval from notified to arrival on-scene; SD=standard deviation; STEMI=ST-elevation myocardial infarction; time to ECG=time interval from arrival to patient’s side to STEMI positive ECG.
Mean response time was 6 minutes, 19 seconds, and was slightly shorter in the ACP-intercept group (5 minutes, 45 seconds v. 6 minutes, 50 seconds; p=0.03). Overall, STEMI patients were under the care of paramedics for 29 minutes, 40 seconds. In the ACP-intercept group, patients were under the care of a PCP paramedic for an average of 7 minutes, 46 seconds before ACP-intercept arrived. The most common type of ACP-intercept path was from a PCP-only first response car to ACP transport crew (80.2% of ACP-intercept cases), whereas a transfer from a PCP-only transport crew to an ACP transport crew was lower (19.8% of ACP-intercept cases). The overall rate of an erroneous STEMI bypass was 17.3% (20.3% in the PCP-only group and 13.5% in the ACP-intercept group; difference of 6.8%, 95% CI –3.6–16.6; p=0.19). Paramedics patched to a base hospital physician in 16.4% of cases; the most common reasons for patching were to request nitro orders followed by questions about destination decisions.
Main results
A total of 127 clinically important events occurred among 214 cases (59.3% overall; 54.2% of PCP-only cases v. 65.6% of ACP-intercept cases; difference of 11.4%, 95% CI –1.8–23.9; p=0.09) (Table 2). The 63 events in the ACP-intercept group were further stratified into events occurring while a PCP was attending (43.7%) or if the event had occurred after care had been transferred to the ACP (21.9%). This left a total of 106 clinically important events occurring under the care of a PCP (Figure 2).
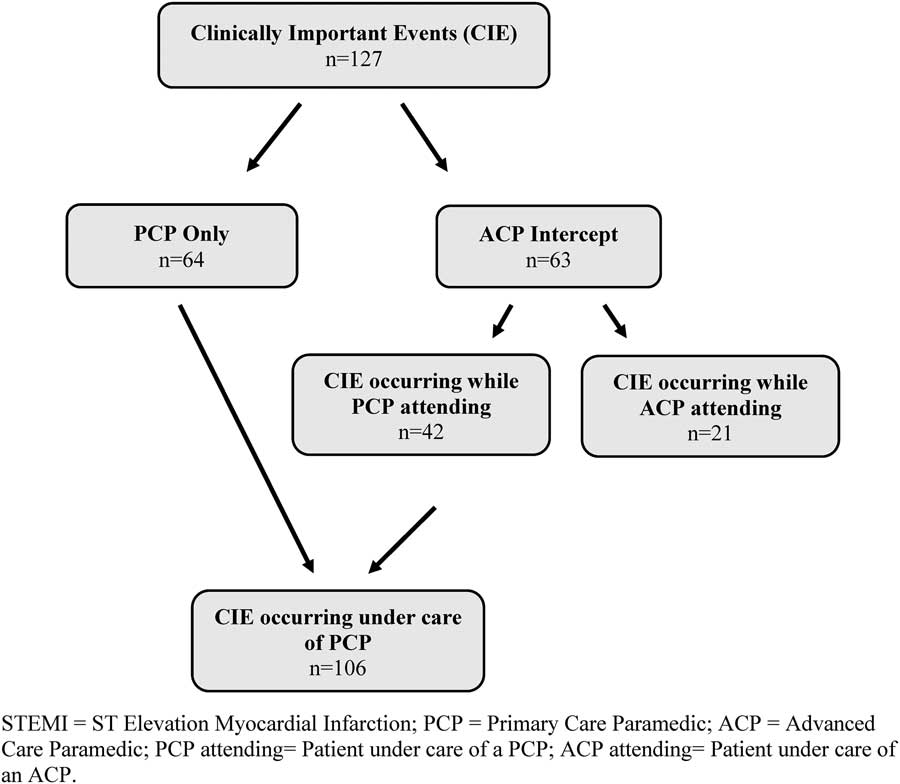
Figure 2 Clinically important events flow diagram.
Table 2 Clinically important events during STEMI bypass
ACP=advanced care paramedic; ACP attending=patient under care of an ACP; A-fib=atrial fibrillation with heart rate greater than 100 beats per minute; altered LOC=altered level of consciousness; BVM=bag-valve mask; CIE=clinically important event; ETT=endotracheal tube; GCS=Glasgow Coma Scale; LMA=laryngeal mask airway; NPA=nasal pharyngeal airway; OPA=oral pharyngeal airway; PCP=primary care paramedic; PCP attending=patient under care of a PCP; prehospital mortality=death during care by prehospital provider; ROSC=return of spontaneous circulation; SVT=supraventricular tachycardia; V-tach=ventricular tachycardia; 3 degree AVB=third-degree AV block.
The most common clinically important events identified were bradycardia (30.4%) followed by hypotension (26.2%) and tachycardia (20.6%). Arrhythmias occurred in 7.5% of cases, most commonly fast atrial fibrillation (3.3%) followed by third-degree heart block (1.9%). Altered level of consciousness (6.5%) and the need for airway manipulation (2.3%) were much less common. There were two cardiac arrests occurring during transport (one in the PCP-only group and one in the ACP-intercept group), both of which achieved ROSC and survived to hospital discharge. Overall, hospital mortality during the index admission was similar between groups (2.5% v. 3.1%; difference of 0.6%, 95% CI –4.5–6.5; p=0.79).
Of all clinically important events, 42.5% could have been addressed by ACP protocols only (Table 3). The vast majority of these consisted of meeting protocol criteria for fluid boluses for hypotension (34.6% of events overall) (see Table 3). Potential interventions for bradycardia, tachycardia, ACLS, and sedation were far less common. The clinically important events occurring in the ACP-intercept group were then examined to specifically determine whether an intervention was indeed performed by ACPs for these events. Of the events occurring under the care of an ACP, an intervention was performed in 51.6% of cases (see Table 3). Most interventions consisted of giving fluid for hypotension in 52.0% of cases with other interventions being far less common (see Table 3).
Table 3 Potential advanced care paramedic interventions for observed clinically important events
ACLS=advanced cardiac life support; ACP=advanced care paramedic; ACP attending=patient under care of an ACP; bradycardia Rx=atropine or transcutaneous pacing; CIE=clinically important event; hypotension/fluids=patient received fluid bolus for hypotension; PCP=primary care paramedic; PCP attending=patient under care of a PCP; sedation for agitation=intravenous or intramuscular midazolam; tachycardia Rx=synchronized cardioversion; VSA=vital signs absent.
DISCUSSION
The main objective of this study was to determine the safety of PCP-only STEMI bypass and categorize clinically important events occurring during transport. We believe this study helps confirm that PCP-only STEMI bypass is a safe intervention and a strong element in the continuum of prehospital STEMI care.
The goal of PCP-only STEMI bypass is to decrease the time from first medical contact to PCI by allowing all paramedics to take patients directly to the PCI centre without the complication or delay of waiting for an ACP crew, on-scene transfer, or ACP-intercept. It also has important implications for PCP-only EMS services. Previous studies in Ottawa showed a mortality benefit for prehospital STEMI bypass due to decreased time to reperfusion.Reference Le May, Wells and So 10 , Reference Le May, So and Dionne 11 While PCP-only STEMI bypass in Ottawa has been in place since 2005, it is in contrast to expert consensus from the AHA and the European Resuscitation Council (ERC) that suggest care providers be able to provide full ACLS care.Reference O’Connor, Brady and Brooks 4 , Reference Steg, James and Atar 12 We believe that PCP paramedics have the necessary skills to intervene in serious complications, such as cardiac arrest, and that other ACP skills are not frequently required during transport.
In our study, patient and system characteristics were similar between the PCP-only and ACP-intercept group with a few notable exceptions. Nitro was administered more frequently in the ACP-intercept group. This is likely due to the provincial protocol for nitro administration in Ontario, which states that nitro can be administered only if patients have a prior history of nitro use or if intravenous (IV) access is obtained. Because IV access is usually not within the scope of practice for PCPs, many STEMI patients often do not meet inclusion criteria. We also found a higher rate of erroneous STEMI bypass in the PCP-only group compared with the ACP-intercept group, although this result was not statistically significant. Finally, the mean response time was slighter shorter in the ACP-intercept group. This is consistent with the most common path for ACP-intercept in our system being a PCP first response car arriving before the ACP transport ambulance.
Our study shows that clinically important events are common in STEMI bypass patients. The rate of events in our study (54.2% in PCP-only cases) is higher than the 26.9% seen in the Ryan et al. study with ACP-only transports and the 12.4% seen in the Ross et al. study.Reference Ryan, Craig, Turner and Verbeek 5 , Reference Ross, Alsayed and Turner 6 This is likely due to differing definitions of clinically important events. For example, minor events in the Bussières et al. study would be classified as important in both our study and the study by Ryan et al.Reference Bussières, Bégin and Leblanc 7 It is critical to note that clinically important events do not equal adverse events; rather they indicate acuity and potential need for intervention within this patient population. Similar to previous studies, we found that the most common events are hypotension and bradycardia.
Of all clinically important events identified in our study, 42.5% could have been addressed by ACP protocols. Although the duration of events was not captured in our data extraction process, many events appeared to be transient, resolved without any intervention, and were of limited clinical significance. Further evidence supporting that serious clinically important events were infrequent is apparent by the fact that ACPs intervened in only about half of the events occurring in the ACP-intercept group. Of the events that could be addressed by ACP protocols, the vast majority of these consisted of meeting protocol criteria for fluid boluses for hypotension (34.6% of events overall). Although we did not extract the exact volume of fluid infused, overall it appeared to be quite small. Of note, the study by Kwong et al. also found that the most common ACP intervention was a fluid bolus for hypotension, and they found that the median volume infused was only 300 ml.Reference Kwong, Ross and Turner 8 Most importantly, in our population other more serious and advanced interventions were infrequent.
While the majority of the clinically important events observed were related to hypotension, these are arguably the patients that would benefit most from urgent PCI and STEMI bypass.Reference O’Connor, Brady and Brooks 4 Indeed the 2013 AHA guidelines state that primary PCI is the treatment of choice for STEMI patients with cardiogenic shock or severe heart failure.Reference O’Gara, Kushner and Ascheim 2 This is based on the “should we emergently revascularize occluded coronaries for cardiogenic shock” (SHOCK) Trial, which showed a significant mortality benefit to revascularization compared with medical stabilization in patients with cardiogenic shock.Reference Hochman, Sleeper and Webb 13 We believe the more important treatment for STEMI patients with hypotension is not a potential time delay waiting for ACP-intercept and IV fluids but rather expedited access to PCI.
Knowing that STEMI patients are at risk of ventricular dysrhythmias, we examined our cohort for cardiac arrest occurring during transport. Of the 214 patients included, there were two cardiac arrests (0.9%) occurring during transport (one in the PCP-only group and one in the ACP-intercept group). The arrest in the PCP-only group was successfully resuscitated with BLS care. Both arrested patients achieved ROSC and survived to hospital discharge. Previous studies have shown an arrest rate of roughly 2% to 3% within similar EMS systems.Reference Ryan, Craig, Turner and Verbeek 5 , Reference Ross, Alsayed and Turner 6 , Reference Kwong, Ross and Turner 8 PCP paramedics have the skill to rapidly recognize cardiac arrest and deploy an AED and basic airway skills.
We believe our study has several strengths. Our study examines an experienced and mature PCP STEMI bypass program that has been functioning since 2005. We examined a large cohort of PCP-only STEMI bypass transports. Furthermore, our study is independently in agreement with two recent studies supporting the safety of PCP-only STEMI bypass, therefore adding to the mounting evidence of safety for PCP-only STEMI bypass.Reference Bussières, Bégin and Leblanc 7 , Reference Kwong, Ross and Turner 8 Finally, we believe that our inclusion of an ACP-intercept cohort allows some determination of actual ACP intervention in the setting of encountered clinically important events.
We decided to exclude ACP-only STEMI bypass cases because the objective of our study was mainly to determine the prevalence of events occurring among PCP-only transports. Although this may have been useful as a direct comparator, this was not the population of interest for our study as it has been reported in previous studies.Reference Ryan, Craig, Turner and Verbeek 5 , Reference Ross, Alsayed and Turner 6 , Reference Cantor, Hoogeveen and Robert 14 We cannot completely exclude the selection of ACP versus PCP crew related to patient severity and not dispatch proximity without a direct comparison of ACP cases. However, in our EMS system, most STEMI cases come into dispatch as chest pain calls and therefore response is simply based on closest unit availability. Furthermore, in the ACP-intercept group, the most common type of intercept path was from a PCP-only first response car to ACP transport crew (80.2%). This indicates that the majority of ACP-intercept cases in our study were a system function rather than PCPs calling for ACP backup.
There are several limitations to our study. Because this was a health record review, it is limited to charted data, at times making it difficult to infer paramedic decision-making based on written observations and interventions. This was especially challenging when viewing transient events and trying to determine whether the paramedic believed this was clinically significant requiring intervention. Our study took place in an urban setting with relatively short transport times, and it is unclear whether these results would apply to a more rural setting with significantly longer transport times. Like other studies on PCP STEMI bypass, our sample size may not have been adequate to fully discern rare clinically important events. A larger prospective study with appropriate sample size calculations for an expected rate of events would more definitely determine safety. Finally, a small number of cases were excluded due to missing data.
CONCLUSION
Clinically important events are common in STEMI bypass patients; however, the vast majority of events appeared to be transient and of limited clinical significance. The most common clinically important events were bradycardia and hypotension. Although a proportion of these events could be addressed differently by ACP protocols compared with PCP protocols, about half of these were acted upon by ACPs, and intervention mostly consisted of modest fluid boluses for hypotension. In this urban population sample, we did not observe any safety concerns regarding PCP-only STEMI bypass. We believe it to be a safe intervention and a strong element in the continuum of prehospital STEMI care.
Competing interests: None declared.