Introduction
Emergency department thoracotomy (EDT) or resuscitative thoracotomy (RT) is often seen as a heroic measure and can be a life-saving procedure. There are few studies on the incidence and success of this procedure in Canadian trauma centres, largely due to our infrequent encounter with penetrating trauma.
Overall survival from EDT ranges from 2.4% to 21.5%. Rhee et al. published one of the largest reviews on the success of EDT and found overall survival to be 7.4%.Reference Rhee, Acosta and Bridgeman 1 Survival from penetrating injuries was higher (8.8%) as compared to blunt injuries (1.4%), and survivors typically had normal neurological outcomes.Reference Rhee, Acosta and Bridgeman 1 In addition, the American College of Surgeons Committee on Trauma published a systematic review on outcomes of EDT, which comprised 42 cohort studies (12 of which reported on neurological sequelae in survivors). 2 The overall survival was 7.8% with survival for penetrating trauma being higher (11.2%) than for blunt trauma (1.6%). 2 The previous two systematic reviews report U.S. trauma centre survival data. Moriwaki et al. recently reported on a cohort of 477 blunt trauma arrests over a 10-year period in Yokohama City, Japan.Reference Moriwaki, Sugiyama and Yamamoto 3 Four hundred and eight patients (86%) had an EDT performed with 131 (27.3%) achieving return of spontaneous circulation (ROSC).Reference Moriwaki, Sugiyama and Yamamoto 3 In the entire cohort, only 14 patients (3%) survived to discharge.Reference Moriwaki, Sugiyama and Yamamoto 3 An EDT performed under wartime condition may yield even higher survival rates, with survival up to 21.5% in one study.Reference Morrison, Poon and Rasmussen 4 Analysing 5 years of data from Afghanistan, Morrison et al. reported on 65 patients undergoing RT.Reference Morrison, Poon and Rasmussen 4 There were nearly equal numbers of gunshot wound (GSW) and blast injuries in the study with survival from GSW being 18.5% and explosion being 23.7%.Reference Morrison, Poon and Rasmussen 4 ROSC was achieved in 51% of the patients in this cohort when RT was performed.Reference Morrison, Poon and Rasmussen 4 Likewise, Edens et al. reported on the survival of patients undergoing an EDT over 4 years at a combat hospital in Iraq.Reference Edens, Beekley and Chung 5 One hundred and one EDTs were performed over this period with the vast majority (93%) being done due to penetrating trauma.Reference Edens, Beekley and Chung 5 Overall survival was 12% with no blunt trauma EDT patients surviving.Reference Edens, Beekley and Chung 5
Although there are relatively few studies on EDT performance outside of the United States and military, a few recent European centres have reported these data. Van Waes et al. reported on 56 patients undergoing an EDT for penetrating trauma over a 10-year period in the Netherlands.Reference Van Waes, Van Riet and Van Lieshout 6 Only 12 patients underwent an EDT in this study with 3 (25%) survivors.Reference Van Waes, Van Riet and Van Lieshout 6 Likewise, Lustenberger et al. reported the experience of a level 1 trauma centre in Switzerland over a 12-year period and found 10 survivors (20%) from 49 EDTs.Reference Lustenberger, Labler and Stover 7 The survival for penetrating trauma was 70% (7 of 10 patients), and the survival for blunt was 7.7% (3 of 39 patients).Reference Lustenberger, Labler and Stover 7
Practice management guidelines for EDT have previously been published. 2 , Reference Burlew, Moore and Moore 8 - Reference Cothren and Moore 10 There are no position statements or guidelines for performance of EDT from the Canadian Association of General Surgeons (CAGS) or Trauma Association of Canada (TAC), but the Western Trauma Association has published a 2012 consensus-based guideline suggesting current accepted indications for EDT (Table 1).Reference Burlew, Moore and Moore 8
Table 1 Indications for Emergency Department Thoracotomy8
* Signs of life include: detectable blood pressure, respiratory or motor effort, cardiac electrical activity, or pupillary reactivity
The merit of EDT has been questioned. A recent publication by Passos et al. examined the performance of EDTs over a 17-year period at Sunnybrook Health Sciences Centre in Toronto, Ontario.Reference Passos, Engels and Doyle 11 In total, 123 patients underwent an EDT with 3 patients surviving (2.4%).Reference Passos, Engels and Doyle 11 Although four patients who received an EDT inappropriately made it to the operating room (OR), no patient survived when the EDT was performed outside of the previously mentioned indications.Reference Passos, Engels and Doyle 11
Given the paucity of data on outcomes of EDT in Canadian tertiary care trauma centres, the primary objective of this study was to define survival rates of EDT due to blunt and penetrating trauma at a Canadian regional trauma centre in Hamilton, Ontario. In addition, as a secondary objective, we sought to evaluate the number of guideline compliant EDTs using the Western Trauma Association practice guidelines. This guideline represents an accepted consensus-based guideline of indications for EDT and is a summary of previously published recommendations.Reference Rhee, Acosta and Bridgeman 1 , 2
Methods
The Hamilton General Hospital is a regional level 1 trauma centre that serves a population of 2.5 million people in Southwestern Ontario. It is staffed 24 hours a day with certified emergency physicians and is an academic teaching centre. The trauma team consists of a trauma team leader who is a staff emergency physician, anesthesiologist, or general surgeon; a trauma fellow; and residents from anesthesia, general surgery, and orthopedic surgery. The emergency department sees an annual census of approximately 45,000 patients. For 2011/2012, there were 309 trauma team activations with an injury severity score (ISS)>12. The majority (373 of 393 or 95.2%) of these patients had blunt mechanisms of injury. The trauma program maintains an up-to-date database of all adult patients>16 years of age with an ISS>12.
The research ethics board of Hamilton Health Sciences and McMaster University approved this medical record review. The trauma database was reviewed for all patients undergoing an EDT over a 20-year period from April 1, 1992 to April 1, 2012. For the period from 2000 onward, charts were available online through our electronic records databases (Sovera and Meditech). For patient records prior to 2000, data were extracted from the film library (microfiche) or directly from the patient’s chart. One author (AC) performed extraction of all of the following data from the trauma database: age, sex, ISS, medical record number, admission and discharge dates, injury type (penetrating v. blunt) and mechanism, hemodynamic variables (systolic blood pressure [SBP], heart rate [HR], respiratory rate [RR]) at presentation in the emergency department—prior to EDT and after EDT, neurological status (Glasgow Coma Scale) before EDT, results of diagnostic studies (bedside ultrasound, computed tomography [CT]), time to EDT, other procedures performed (chest tube[s], cricothyrotomy, central line, etc.), disposition (OR v. intensive care unit [ICU]), time to OR, operative intervention(s) required, definitive injuries sustained, and hospital and ICU length of stay. Additional data not found in the database were extracted by another author (JJO) from primary chart review, including type of physician performing the EDT, number of years of experience of physician performing the EDT, blood product requirements in the first 24 hours, time from arrival to performance of the EDT, and time from arrest (if applicable) to the EDT. Using the Western Trauma Association guidelines for EDT indications, we categorized each EDT as indicated or not indicated.
For all descriptive statistics, 95% confidence intervals (CIs) are recorded where appropriate. For comparisons involving nominal data, the Fisher’s exact test or chi-square has been used, and, for all parametric data, a Student’s t-test has been used.
Results
During the study period, 65 patient charts were identified as having undergone an EDT. Seven of these charts were excluded. Six (9.2%) did not undergo an EDT, and 1 record could not be found, leaving 58 patients (89.2%) for analysis (Figures 1 and 2). The mean age of patients undergoing an EDT was 37.1 years with 43 of 58 (74.1%) being male. The mean ISS was 34.7 (95% CI 30.4 to 39.0). The majority of patients (34 of 58 patients or 59%) underwent an EDT for blunt trauma with only 1 (2.9%) survivor (Table 2). There were 24 patients who underwent an EDT for penetrating trauma with 5 survivors (20.8%). Overall, 18 patients (31%) survived to OR, and 6 patients (10.3%) survived to hospital discharge (Figure 1 and Table 2). Patients undergoing an EDT without cardiac arrest had a significantly higher rate of survival (3 of 6 or 50%) compared with those who underwent an EDT in cardiac arrest (3 of 52 or 5.8%) (p=0.01, Table 3). Those with a shorter time to an EDT (1.7 min, 95% CI 0.1 to 3.3 min v. 15.8 min, 95% CI 11.6 to 20.0 min) also had a significantly higher rate of survival (p=0.001, Table 3).
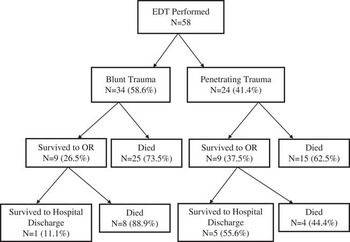
Figure 1 Emergency Department Thoracotomy Survival Stratified by Mechanism of Injury.

Figure 2 Timeline of Emergency Department Thoracotomies Performed at the Hamilton General Hospital.
Table 2 Emergency Department Thoracotomy Survival Stratified by Mechanism of Injury
Table 3 Comparison of Survivors and Non-Survivors for Patients Undergoing EDT
* Statistically significant. For mean time from arrest to EDT, a Student’s T-test was used. For EDT performed for refractory shock, Fischer’s Exact Test was used.
^ Data only available for 50 patients
# Data only available for 47 patients
Survivors required a mean of 23 (±16.8) units of blood products in the first 24 hours and stayed a mean of 21.2 (±23.7) days in the hospital (Table 4). Although no formal neurological assessment data could be obtained from the records reviewed, all six survivors were discharged home, with two of them requiring some personal support by a personal caregiver/family member (assistance with instrumental activities of daily living) but were independent with most daily activities.
Table 4 Secondary Outcomes of Emergency Department Thoracotomy
^ 1 blood product =1 unit pRBC, 1 unit FFP, 1 unit adult dose plts, or 10 units cryoprecipitate. Does not include recombinant Factor VIIa.
Seventy nine percent of EDTs at our institution were performed using accepted indications, as set out by the Western Association of Trauma (see Table 4). Of the non-indicated EDTs, five were in the setting of penetrating trauma and seven were due to blunt trauma. No patient survived an EDT when performed outside of these accepted criteria. One patient had ROSC and was transferred to the OR but, after a second cardiac arrest in the OR, was unsuccessfully resuscitated. No organs were donated for non-surviving patients undergoing an EDT.
A majority of EDTs were performed by staff physicians, but nearly one quarter (11 of 47 or 23.4%) were performed by residents or fellows. General surgeons performed most EDTs (36 of 50 or 72%), but emergency room physicians were responsible for almost one fifth (9 of 50 or 18%). The physicians performing EDTs, their specialties, and years of experience were not associated with survival (see Table 2).
Discussion
The present study is an important one because it describes appropriateness and outcomes of an EDT at a tertiary care trauma centre in Canada. Our study reports on the outcomes of 58 patients undergoing an EDT at our institution with a combined survival of 10.3% (6 patients). The majority of survivors (5 of 6 or 83.3%) suffered penetrating trauma.
There are currently no published guidelines from the CAGS or TAC, so Canadian emergency physicians and trauma team leaders might consider guidelines, such as those published by the Western Trauma Association, in deciding when to perform an EDT. It is important that outcomes at Canadian trauma centres are similar when these published guidelines are applied to our population. Our study is an important one because there have been only three studies to date that describe the outcome of an EDT at Canadian trauma centres.Reference Passos, Engels and Doyle 11 - Reference Alanezi, Milencoff and Baillie 13 Karmy-Jones et al. published data on penetrating cardiac injury in Edmonton over a 2-year period with only eight patients identified, of which three (38%) survived.Reference Karmy-Jones, van Wijnggaarden and Talwar 12 Six of these (75%) underwent an EDT, of which two (33.3%) survived.Reference Karmy-Jones, van Wijnggaarden and Talwar 12 Both had presented in shock and arrested after ED arrival.Reference Karmy-Jones, van Wijnggaarden and Talwar 12 Alanezi et al. reported on major cardiac injuries over a 9-year period and found 27 cases, of which 11 (40.7%) underwent an EDT.Reference Alanezi, Milencoff and Baillie 13 Only one patient (9.1%) who underwent an EDT survived.Reference Alanezi, Milencoff and Baillie 13 As previously mentioned, Passos et al. reported on outcomes of EDTs at a large level 1 trauma centre in Toronto, Ontario.Reference Passos, Engels and Doyle 11 The authors reported a survival rate of just 2.4% for 123 EDTs performed.Reference Passos, Engels and Doyle 11 Our current data add to the growing body of literature on outcomes of EDTs at Canadian trauma centres.
In contrast to Passos et al.’s study in which 51% of EDTs were considered inappropriate, only 12 of the 58 EDTs (20.7%) in our series were performed outside of the criteria set out by the Western Trauma Association. Often when patients present to the ED, the exact time of arrest is unknown, and the decision to perform an EDT must be made immediately. This is expected to produce some inappropriate EDTs and is reflected in the fact that 10 of the 12 (83.3%) inappropriate EDTs in our database occurred in patients who had an arrest in the field and received an EDT as soon as they arrived at our facility. No patient who underwent an EDT outside of the Western Trauma Association’s recommendations survived to hospital discharge.
One of the reported outcomes from an EDT is organ donation, as suggested by Schnurger et al.Reference Schnurger, Inaba and Branco 14 Similar to Passos et al.’s study, there were no organs donated from non-survivors undergoing an EDT. This remains a potential outcome to evaluate in trauma registries, and a consideration for any patient in whom survival is not expected or a declaration of brain death occurs after an EDT.
This study has several limitations. As a retrospective medical record review, there are biases of retrospectively collected data, specifically case selection bias. Our trauma database inappropriately coded six patients as having undergone an EDT when in fact they had undergone a tube thoracostomy. All data in our trauma registry are entered prospectively, and information is kept as accurately as possible, but it is possible that information was entered incorrectly or was illegible on the emergency department record. For this medical record review, one author (JJO) abstracted all data missing from the trauma registry, and there is potential for those data to have been entered incorrectly. Ideally, two abstractors could extract the missing data and have their performance compared with use of the kappa statistic.
Although almost all medical records were complete, there were incomplete data on median time from scene to hospital and median years of experience and specialty of the physician performing an EDT, which limit the generalizability of these variables.
Perhaps the greatest limitation in the present data relates to the small numbers of patients. Despite using 20 years of data, we were able to identify only 58 patients undergoing an EDT at our trauma facility. These low numbers are reflective of the rarity of the procedure, and most studies of EDT have similar patient numbers.
Conclusions
Survival from an EDT at our smaller regional trauma centre falls within the range of survival reported in the larger datasets of EDT around the world. Patients undergoing an EDT for refractory shock prior to cardiac arrest had the highest rates of survival. For those in cardiac arrest, short times to performance of an EDT were associated with a higher rate of survival. No survivor in this dataset survived when the EDT was performed outside of accepted guidelines. Adherence to guidelines, such as those produced by the Western Trauma Association, may avoid unnecessary EDT. Future studies should evaluate predictors of survival and outcome of EDT using pooled data from other Canadian centres.
Competing interests: None declared.










