CLINICIAN’S CAPSULE
What is known about the topic?
Oral anticoagulation (OAC) reduces stroke risk in patients with atrial fibrillation or flutter; however, initiation rates in patients discharged from the ED are low.
What did this study ask?
Can a simple quality improvement intervention increase the initiation of appropriate OAC in the ED?
What did this study find?
The rate of OAC initiation was increased by 8.5%.
Why does this study matter to clinicians?
This simple intervention is transferrable and therefore can improve patient care.
Rates of oral anticoagulation (OAC) initiation in patients with atrial fibrillation (AF) or atrial flutter (AFL) directly discharged from the emergency department (ED) are low. We implemented a quality improvement intervention consisting of a reminder statement prompting OAC initiation, manually added to electrocardiograms with a preliminary AF/AFL interpretation. There was an 8.5% absolute increase in the rate of appropriate OAC initiation. This support package is transferrable and can be readily implemented in other EDs to improve OAC rates for AF/AFL.
INTRODUCTION
Atrial fibrillation (AF) and atrial flutter (AFL) are independent risk factors for stroke and systemic embolism, increasing risk by fivefold in all age groups.Reference Wolf, Abbott and Kannel 1 The percentage of strokes attributable to AF/AFL increases from 1.5% at 50 to 59 years of age to more than 20% in patients ages 80 to 89 years.Reference Macle, Cairns and Leblanc 2 Furthermore, strokes attributed to AF/AFL are associated with a higher recurrence rate, disability, and mortality.Reference Miller, Andersson and Kalra 3 Multiple studies have demonstrated the benefit of oral anticoagulation (OAC) for stroke prevention in AF/AFL patients.Reference Giugliano, Ruff and Braunwald 4 - Reference Granger, Alexander and McMurray 7 The current Canadian Cardiovascular Society (CCS) guidelines endorse use of the “CHADS65” risk scoring system, with OAC being recommended for all patients ages≥65 years or having one or more risk factors (congestive heart failure, hypertension, diabetes, or stroke/transient ischemic attack/systemic embolism).Reference Macle, Cairns and Leblanc 2
AF/AFL are the most common arrhythmias presenting to the emergency department (ED).Reference Atzema, Austin and Miller 8 - Reference Miyasaka, Barnes and Gersh 10 Many patients are discharged directly from the ED, placing ED physicians in a unique position to initiate guideline-directed OAC therapy for these patients. In fact, ED initiation of OAC is associated with improved long-term adherence.Reference Atzema, Austin and Chong 11 Despite this, the rate of appropriate initiation of OAC in patients discharged from EDs remains consistently low, as shown by a multicentre prospective study conducted in 124 Spanish EDs and a retrospective assessment of two EDs in Vancouver, where only 45% and 47% of patients, respectively, were initiated on OAC.Reference Coll-Vinent, Martin and Malagon 12 , Reference Scheuermeyer, Innes and Pourvali 13 In a recent study conducted in three EDs in Winnipeg, the rate of newly filled OAC prescriptions for appropriate anticoagulation of actionable AF was 32% at a 90-day, post-ED visit.Reference Scott-Herridge, Seifer and Steigerwald 14 Suboptimal rates of initiating appropriate OAC therapy represent a missed opportunity in the ED; however, there are few studies exploring the efficacy and safety of interventions aimed to increase the appropriate use of OAC therapy for AF/AFL detected in the ED.
We investigated the impact of an OAC reminder, coupled with a simple decision-making support package, on the rate of initiating appropriate OAC therapy in patients with AF/AFL discharged from the ED.
METHODS
Study setting and study population
The study was performed in the four adult EDs in Calgary, Alberta, which serve a population of approximately 1.2 million people. All of these EDs are part of teaching hospitals with access to consulting specialists, including internists and cardiologists. Between January 1, 2015, and December 31, 2016, all patients with a 12-lead electrocardiogram (ECG) documenting AF/AFL performed in the ED were identified using the MUSE database (GE Healthcare, Wauwatosa, WI). Patient comorbidities (including congestive heart failure, hypertension, diabetes, ischemic, or hemorrhagic stroke) were determined through linkage with the Calgary Health Region discharge abstract database, as previously described.Reference Southern, Norris and Quan 15 Additionally, patients’ electronic medical records were reviewed manually to confirm the accuracy of extracted data and to determine the status of hospital admission or direct discharge from the ED. Patients with valvular AF/AFL, defined as the presence of rheumatic mitral stenosis, prosthetic heart valve, or mitral valve repair,Reference Di Biase 16 , Reference Verma, Cairns and Mitchell 17 were excluded from the analysis. Patients with non-valvular AF/AFL were considered eligible for anticoagulation with a CHADS65 score of ≥1, consistent with current CCS AF/AFL guidelines.Reference Verma, Cairns and Mitchell 17 The primary study cohort consisted of patients who were discharged directly from the ED with ECG-documented AF/AFL, not previously prescribed OAC therapy, despite eligibility or not previously known to have AF/AFL.
Study design
The reminder study had a prospective design, using an observational cohort to obtain baseline data, and an interventional cohort to test the effects of a quality improvement intervention. During the pre-intervention observational phase (January 1 to December 31, 2015), we determined existing rates of OAC use prior to ED presentation and within 90 days of discharge. The intervention was implemented in two of the EDs (ED-intervention), with each serving an average annual patient volume of 82,000 and 79,000 on May 1, 2016, with a planned 1-month run-in phase and prospective data collection starting on June 1. To account for possible temporal changes in OAC prescription rates, data were also collected from the remaining two EDs, where no intervention was performed (ED-control), each serving an approximate annual patient volume of 78,000 and 65,000. The ED pairings were chosen based on usual staff work patterns to minimize the chance of individual ED physicians working at both ED-intervention and ED-control sites. This study was approved by the Conjoint Health Research Ethics Board of the University of Calgary and conducted in accordance with the Declaration of Helsinki. Individual patient consent was waived due to the nature of the study design.
Intervention
Any 12 lead-ECG with a preliminary, machine-generated, interpretation of AF/AFL had a sticker manually applied, stating: “If physician-confirmed AF, consider initiation of oral anticoagulation as indicated based on CCS 2014 guidelines” (see Supplemental Figure 1). Additionally, a one-page AF/AFL decision-support package containing the CCS algorithm for deciding on antithrombotic therapy in non-valvular AF/AFL, and risk factors for bleeding, was attached to the ED chart (see Supplemental Figure 1). Additionally, the package contained a simplified referral form to two previously established outpatient cardiology clinics with a focus on management of patients with AF/AFL to facilitate outpatient consultation (see Supplemental Figure 2). Other than directly attaching the referral forms to the appropriate ED charts, the process of outpatient referral was not altered. To validate the preliminary ECG machine rhythm interpretation, 200 ECGs were randomly selected and reviewed by a cardiac electrophysiologist F. Russell Quinn [FRQ].
Primary outcome
The primary outcome was the rate of pharmacy-filled OAC prescriptions among patients with AF/AFL and CHADS65 score of≥1 within 90 days of the index ED visit. The rate of filled OAC prescriptions (i.e., warfarin, rivaroxaban, dabigatran, or apixaban) was determined through linkage to the provincial Pharmacy Information Network, which prospectively collects dispensed medication information from more than 95% of all pharmacies in the province of Alberta. Pre-existing OAC therapy was defined as a filled OAC prescription within the 180 days preceding ED presentation. We also examined prescription rates of OACs in low-risk patients (i.e., CHADS65 score of zero) to assess for a possible change in OAC prescription rates as a result of the intervention. Specifically, we wanted to assess whether rates of inappropriate anticoagulation in low-risk patients increased inadvertently as a product of the intervention.
Statistical analysis
Continuous variables are presented as a median and standard deviation. Categorical data are expressed as absolute numbers and percentages. Analysis of variance (parametric) and the Kruskal-Wallis test (non-parametric) were used to compare continuous variables, whereas the Pearson χ2 test was used to compare categorical variables. We compared differences in our primary outcome, OAC initiation within 90 days, prior to and after implementation of our intervention. Analyses were pre-specified and performed in the cohort of patients surviving beyond 90 days of an ED encounter. Factors associated with a prescription of guideline-appropriate OAC in AF/AFL patients discharged from the ED were assessed using bivariate and multivariable logistic regression analysis from which odds ratios and 95% confidence intervals (CI) were obtained.
Based on previous studies with an expected baseline OAC prescription rate of 47%,Reference Scheuermeyer, Innes and Pourvali 13 and the intervention population representing 0.36 of the total population (7 months intervention v. 12 months pre-intervention), a sample size of 892 patients (571 pre-intervention, 321 post-intervention) would have a power of 80% to detect a 10% absolute increase in appropriate OAC rates, with an alpha level of 0.05. We anticipated that enrolment would be completed by December 31, 2016. However, upon stopping the study, it became apparent that more patients were admitted or were already on OAC than we expected during the intervention phase. Analyses were completed with those enrolled during the planned study period. All analyses were performed using Stata 15.1 (Stata Corp., College Station, Texas). All statistical tests were two-sided, with p values<0.05 considered significant.
RESULTS
Baseline rates of anticoagulation amongst patients with AF/AFL discharged from the ED
During the observational phase (January 1 to December 31, 2015), there were 4,948 patients with documented AF/AFL during an ED visit across the four sites; 2,130 (43.0%) patients were discharged directly from the ED. Of the patients discharged from the ED, 713 (33.5%) patients were previously not on OAC and had a CHADS65 score of≥1. Within 90 days of discharge from the ED, only 265 (37.2%) patients were initiated on OAC therapy. In a random sample of 200 ECGs with an initial computer interpretation of AF/AFL, the rhythm interpretation was correct in 199 (99.5%) when reviewed by a cardiac electrophysiologist (FRQ).
Effect of intervention on rates of a new OAC prescription within 90 days of ED discharge
Table 1 summarizes the characteristics of subjects before and after the intervention in the ED-control and ED-intervention sites. No significant differences were present in any of the baseline characteristics. Following implementation of the intervention, the rate of appropriate initiation of OAC increased from 38.7% to 47.2%, an absolute increase of 8.5% (95% CI, 0.3% to 16.7%, p=0.041; Table 2, Figure 1). In the ED-control sites, over the same study period, there was no change in the rates of OAC prescription (see Table 2, Figure 1). During the intervention period, the rate of appropriate initiation of OAC in the ED-intervention sites was significantly higher than at the ED-control sites (p=0.020). Rates of OAC initiation in patients with a CHADS65 score of 0 did not change in any site during the intervention period (see Table 2). Among patients initiated on OAC therapy, direct OACs constituted 60% of prescriptions filled (i.e., rivaroxaban 27%, apixaban 25% and dabigatran 8%).
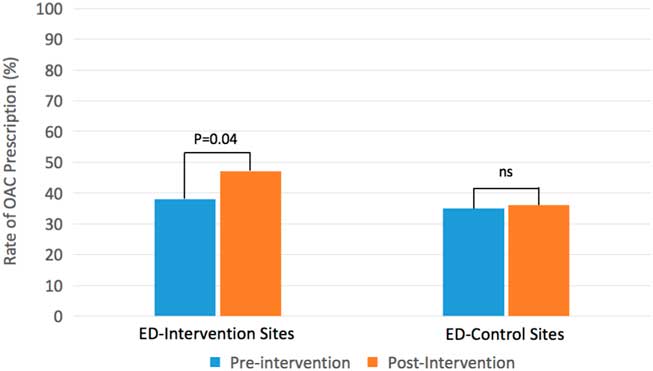
Figure 1 Rates of new OAC prescription in patients with non-valvular AF/AFL, discharged from the ED, with a CHADS65 score of≥1 and alive at 90 days. Legend: ED-Intervention – emergency departments where the intervention was implemented. ED-Control – emergency departments that did not undergo implementation of the intervention. Abbreviations: AF/AFL=atrial fibrillation/atrial flutter; ED=emergency department; OAC=oral anticoagulation.
Table 1 Characteristics before and after an intervention of patients with non-valvular AF/AFL discharged from the emergency department (ED-intervention) with CHADS65 score of≥1, not previously on OAC and alive at 90 days
AF=atrial fibrillation; AFL=atrial flutter; ED=emergency department; No.=number; OAC=oral anticoagulation; SD=standard deviation.
Table 2 Rates of anticoagulation within 90 days of ED discharge among patients with non-valvular AF/AFL, not previously on OAC and alive at 90 days
AF=atrial fibrillation; AFL=atrial flutter; ED=emergency department; OAC=oral anticoagulation.
To evaluate the impact of mortality on the results, a secondary analysis was performed that included patient deaths within 90 days (i.e., deaths prior to assessment of the primary outcome at 3 months). The mortality at 3 months in the ED-intervention group was similar at pre- and post-implementation of the reminder intervention (6.8% v. 8.2%, p=ns). Similarly, the 3-month mortality in the ED-control group were also comparable pre- and post-implementation (8.8% v. 13.8%, p=ns). The magnitude of effect post-implementation intervention was similar to the primary analysis; the rate of appropriate initiation of OAC increased from 36.8% to 45.9%, p=0.02. Further, in our secondary analysis, there was no change in the rates of OAC in the ED-control site. In summation, the inclusion or exclusion of patient deaths prior to outcome assessment at 3 months did not affect the magnitude of benefit that the reminder intervention conferred.
An exploratory analysis was conducted to assess whether the CHADS65 score had an impact on the rates of OAC initiation. Among OAC-naïve patients with lower CHADS65 scores of 1 or 2 in the ED-intervention sites, there was a significant increase in the rate of OAC initiation (37.4% to 50.3%, p=0.008). However, there was no significant change in anticoagulation rates among patients with CHADS65 scores greater than 2 (42.0% to 37.7%, p=0.6).
Predictors of OAC initiation in eligible patients discharged from the ED
Table 3 compares characteristics of those eligible patients who were or were not started on OAC within 90 days of ED discharge during the entire study period. Patients who were initiated on OAC therapy were younger, more likely to have AF/AFL as their primary diagnosis, and less likely to have a history of heart failure or hemorrhagic stroke. We performed a multivariate analysis to determine the independent predictors of OAC initiation (Table 4). Patients presenting with a primary diagnosis of AF/AFL were three times more likely to be initiated on OAC compared to those where it was a secondary diagnosis. The reminder intervention was independently associated with a 1.5-fold increase in appropriate OAC therapy when adjusted for age, history of heart failure, prior hemorrhagic stroke, and AF as the primary ED discharge diagnosis. A history of heart failure was associated with lower rates of OAC initiation.
Table 3 Characteristics of patients with non-valvular AF/AFL discharged from the ED with CHADS65 score of≥1 and not previously on OAC, stratified by a new OAC start within 90 days

AF=atrial fibrillation; AFL=atrial flutter; ED=emergency department; No.=number; OAC=oral anticoagulation; SD=standard deviation.
Table 4 Predictors of OAC initiation within 90 days after ED discharge among patients with non-valvular AF/AFL and CHADS65 of≥1 (N=1,118)
* Multivariable model includes age (per 10 years), female gender, heart failure, AF as primary diagnosis, hemorrhage stroke, and reminder intervention.
AF=atrial fibrillation; AFL=atrial flutter; ED=emergency department; NS=not significant; OAC=oral anticoagulation.
To assess the impact of the ED facility on OAC initiation, we performed a separate analysis limited to the pre-intervention, observational phase (N=713). The ED facility was not predictive of OAC initiation among OAC-naïve AF/AFL patients following an ED discharge.
DISCUSSION
Among patients with AF/AFL discharged directly from the ED, the initiation of guideline-recommended OAC therapy remains low. In this study, a simple intervention, consisting of a reminder statement and decision-support package resulted in a significant increase in the rate of appropriate OAC therapy.
Barriers to OAC therapy initiation in the ED
As a frequent point of contact for many AF/AFL patients, ED physicians are in a unique position to facilitate appropriate guideline-directed OAC therapy for AF/AFL patients. Further highlighting the importance of the ED physician is the finding that an initiation of OAC therapy prior to discharge from the ED can lead to a greater long-term adherence.Reference Atzema, Austin and Chong 11 It remains unclear why the rates of initiation of OAC therapy in patients with AF/AFL discharged from EDs remain consistently low. In a survey of emergency physicians in Spain who explored reasons for not prescribing OAC, almost 50% of ED physicians cited the “lack of indications” (due to the perception of a low risk of stroke), despite patients meeting criteria for anticoagulation as per guideline recommendations.Reference Coll-Vinent, Martin and Malagon 12 Thirty-three percent of ED physicians deemed antiplatelet monotherapy an adequate stroke prophylaxis, and only 5.6% of physicians referred to other care providers to assess the need for OAC.
Several potential barriers to OAC initiation in the ED have been raised, such as inadequate time to discuss the risks and benefits of anticoagulation, inability to ensure adequate follow-up, or pedagogical differences in ED physicians’ practice of stroke prevention.Reference Atzema 18 , Reference Barrett, Vermeulen and Self 19 Furthermore, reluctance to prescribe OAC may stem from the practice behaviours when warfarin was the sole oral anticoagulant option. Given the complexity of initiating warfarin and ensuring ongoing monitoring, OAC initiation in the ED can be challenging and unpalatable, especially considering regional variability in the accessibility of multidisciplinary supports (e.g., anticoagulation clinic and AF clinic).Reference Barrett and Marill 20 Additionally, addressing an issue of long-term risk may become a secondary consideration when there are other acutely ill patients to manage.
Nevertheless, if not directly initiating anticoagulation, ED physicians still have a pivotal role in facilitating outpatient referrals to optimize management of patients with AF/AFL. In our study, we assessed OAC initiation within 90 days of an index visit, which would capture OAC initiation directly within the ED or facilitated via a consultant referral (i.e., assessment and management of stroke prevention in AF/AFL delegated to a family physician, internist, or cardiologist). Interestingly, despite the availability of consultant services, only 38.8% of OAC-naïve patients with AF/AFL were started on appropriate OAC therapy within 90 days of an ED discharge. This rate is similar to previous studies that had examined the rate initiation of OAC in the ED prior to discharge.Reference Coll-Vinent, Martin and Malagon 12 - Reference Scott-Herridge, Seifer and Steigerwald 14 Therefore, there still remains a significant care gap and potential lost opportunity in the management of AF/AFL with regards to stroke prevention.
Few studies have directly assessed the impact of interventions on OAC prescription within the ED setting. Skolarus et al. found that there was no difference in rates of warfarin use after implementing their intervention of mailing letters to patients and their family physicians following an ED evaluation.Reference Skolarus, Morgenstern and Scott 21 The negative results are not unexpected; prior meta-analyses demonstrate that printed educational letters have limited efficacy.Reference Grudniewicz, Kealy and Rodseth 22 Coll-Vinent et al. showed a significant increase in the rate of warfarin prescriptions by ED physicians following an implementation of an AF-treatment protocol consisting of a pocket brochure and physician education sessions.Reference Coll-Vinent, Pacheco and Junyent 23 However, due to the nature of the study design, including lack of an adequate control, there are limitations in the generalizability of the study.
In our study, the implementation of a simple quality improvement strategy resulted in a significant improvement in appropriate OAC therapy in patients directly discharged from EDs. Our findings align with previous evidence demonstrating improved patient care through the implementation of standardized order sets or checklists.Reference Chin and Wallace 24 , Reference Milani, Lavie and Dornelles 25 The impact of our intervention, which included a paper-based reminder, was larger compared with previous attempts using automated electronic reminders in a family practice setting,Reference Robson, Dostal and Mathur 26 or an inpatient setting.Reference Silbernagel, Spirk and Hager 27 Therefore, the implementation of decision-making algorithms either as a stand-alone paper-based system or integration into computer-based order sets can lead to improved care of patients with AF/AFL in EDs.
Risk-treatment paradox
In our cohort, patients with an older age and patients with a history of heart failure were less likely to be initiated on OAC following their discharge from the EDs. Reasons for underutilization of OAC in this population are unclear. One possibility is that these patients were frailer and had additional comorbidities that would preclude OAC initiation. It is important to note that therapy should be tailored to each individual patient by assessing the risk of stroke and balancing that to the risk of major bleeding.Reference Macle, Cairns and Leblanc 2 The use of administrative databases in our study is unlikely to capture the nuances of physician decision-making, which may account for the underutilization of OAC prescription in the heart failure population with AF/AFL.
Another explanation may reflect the discord between the bleeding risk estimated using validated risk scores and physician-assigned risk. In our study, the increased OAC initiation rates resulting from the intervention were limited to patients with lower CHADS65 scores (i.e., scores of 1 to 2) compared with higher CHADS65 scores (i.e., CHADS65 of > 2). Although our study was not powered to differentiate OAC initiation rates stratified by the CHADS65 score, the results of this exploratory analysis are consistent with the so-called “risk-treatment paradox.”Reference Sandhu, Bakal, Ezekowitz and McAlister 28 Unfortunately, our current stratification tools of stroke risk and complications from anticoagulation are imprecise, and clinical judgement may result in an overestimation of risk compared with benefit; that is, physicians may underutilize appropriate anticoagulation in patients with the highest stroke risk due to an exaggerated perception of fall or bleed risk.Reference Tan and Ellenbogen 29 More precise risk stratification tools could help address this issue and improve rates of anticoagulation in populations that would derive the greatest benefit.
Limitations
Our study has several important limitations. This study was observational and therefore inherently susceptible to confounding factors. Furthermore, due to the non-randomized nature of the study, there may be prognostic differences between the intervention and control groups. During the intervention phase of the study, we relied on a preliminary interpretation of rhythm based on an automated ECG machine algorithm. A review of these ECGs by a cardiac electrophysiologist revealed that the machine algorithm correctly identifies AF/AFL more than 99% of the time. Our intervention also stated that the diagnosis of AF/AFL should be confirmed by a physician. We identified patients with AF/AFL by relying solely on ECG documentation of such rhythm while they were in the ED and did not identify patients without an ECG performed or those with paroxysmal AF/AFL who were in sinus rhythm while in the ED. Our intervention was labour intensive because it required the manual addition of a reminder sticker to ECGs at the time that they were obtained as well as attachment of the decision-making algorithm, potentially limiting the generalizability to other EDs with more limited resources. However, most modern ECG machines could be programmed to automatically include the reminder statement used in this study. It is possible that the temporal increase in OAC prescriptions in the ED-intervention groups was due to factors in addition to than the reminder intervention, which we were not able to control for, given the study design. However, the similar baseline (pre-intervention) rates of anticoagulation between ED-intervention and ED-control groups would argue against any substantive differences. Lastly, we relied on an external database to identify OAC prescriptions within 90 days. This database captures prescriptions that are dispensed only, so it may underestimate the total number of OAC prescriptions written by ED physicians and does not account for patient adherence. We did not explore the patient factors that may lead patients to fill or not fill an OAC prescription, nor did we examine patient adherence beyond 90 days.
CONCLUSION
In our study, implementation of a quality improvement intervention, consisting of a simple reminder and a decision-support tool, significantly increased the appropriate initiation of OAC within 90 days in high-risk AF/AFL patients discharged from the ED. Additional study is warranted to explore the potential barriers to OAC initiation in the ED.
Acknowledgements: We would like to thank all of the cardiology technologists in the Calgary Health Region for their participation in this project. We also thank Mingkai Peng for assistance with the statistical analysis. Drs. Chew and Rezazadeh are members of the Cardiac Arrhythmia Network of Canada (CANet) HQP Association for Trainees (CHAT), and Dr. Quinn is a CANet Network Investigator.
Financial support: This study was supported by the Canadian Cardiovascular Society Bayer Resident Award.
Competing interests: None declared.
SUPPLEMENTARY MATERIALS
To view supplementary material for this article, please visit https://doi.org/10.1017/cem.2018.415









