INTRODUCTION
This statement underwent revision in 2006 and most recently in 2012. 3 , Reference Henneberry, Hanson and Healey 4 The 2006 position statement was the first revision supporting the incorporation of EUS training into emergency medicine (EM) residency programs accredited by the Royal College of Physicians and Surgeons of Canada (RCPSC) as well as the College of Family Physicians of Canada (CFPC). 3 In 2008, the RCPSC included EUS as a core competency to its EM training standards, 5 and, in 2010, the CFPC introduced EUS as a terminal training objective for CFPC-EM programs.Reference Mackey and Steiner 6
The most recent literature demonstrates that EUS training in Canadian EM residency programs is prevalent, with almost all programs providing ultrasound training as part of the residency curriculum as of 2011. However, there is considerable heterogeneity in the scope of ultrasound training, curricula, and determination of proficiency.Reference Kim, Theoret and Liao 7 - Reference Kim, Theoret and Liao 9 Although most programs provide training in focused assessment with sonography for trauma (FAST), intrauterine pregnancy (IUP), abdominal aortic aneurysm (AAA), basic cardiac, and central line placement, there is considerable variability in the delivery of training for other applications such as biliary, renal, soft tissue, thoracic, and other ultrasound-guided procedures. This variability also extends to the determination of competency, with programs using various combinations of ultrasound course certification, direct observation of performance, number of studies, and written exams.Reference Kim, Theoret and Liao 7 Furthermore, the classification of applications as core versus advanced is evolving at a rapid rate. As recently as 2010, a survey of EUS experts, EM residency program directors, and EM residents considered ultrasound for the detection of pneumothorax and hemothorax to be advanced skills.Reference Fischer, Woo and Lee 10 This level of heterogeneity may explain why, in one national survey, 97% of senior EM residents agreed or strongly agreed that there should be established national guidelines for residency training in EUS.Reference Kim, Theoret and Liao 9
With this in mind, the CAEP Emergency Ultrasound Committee (EUC) formed the EUS Curriculum Working Group, consisting of EUS experts and educators from every EM training site in Canada. This group strives to combine best EUS evidence with contemporary curriculum design processesReference Grant 11 , Reference Atkinson, Bowra and Lambert 12 to create an implementable, evidence-guided core EUS curriculum for 2017 while also setting targets and recommendations for a second iteration in 2020.
Integral to this approach was a review of EUS applications with regard to impact on patient care and ED flow as well as a review of the current state of EUS training in Canada. The International Federation of Emergency Medicine (IFEM) has recommended that, when designing an EUS curriculum, consideration should be given to “disease prevalence, impact of disease, potential for patient benefit and resources when deciding what core applications to include” in the curriculum.Reference Atkinson, Bowra and Lambert 12 The working group members also identified and acknowledged regional differences in EUS resources, infrastructure, and support for training. With the goal of striking a balance between priorities and challenges, working group members collaborated both electronically and in-person.
Contemporary curriculum design processes include widespread consultation to ensure support and successful implementation. The General Medical Council, based in the United Kingdom, defines a curriculum as “a statement of the intended aims and objectives, content, experiences, outcomes and processes of a program, including a description of the structure and expected methods of learning, teaching, feedback and supervision.”Reference Grant 11 As such, a curriculum proposal must address each of the aforementioned items. Through this first report, the CAEP EUS Curriculum Working Group presents the rationale behind establishing a national postgraduate curriculum, and a consensus on which EUS applications should be included. In the future, the EUS Curriculum Working Group plans to further define the curriculum in terms of learning experiences, supervision and feedback, and management of curriculum implementation, including curriculum review and updating. This will occur in consultation with program directors, educators, and other stakeholders.
METHODS
The CAEP EUS Curriculum Working Group was established in the summer of 2015 as a working group of the CAEP EUC and is chaired by authors DK and PO (Appendix A lists members and their respective institutions). There was a deliberate effort to recruit EUS educators from throughout Canada to ensure representation from all Canadian EM residency training sites and both training streams (CFPC and RCPSC). After providing an opportunity to review relevant clinical and training literature, the group used a modified Delphi methodReference Keeney, Hasson and McKenna 13 , Reference Stansfield, Woo and Tam 14 to determine content of learning (objectives and outcomes of training), models of learning, learning experiences, and supervision.
A shared online workspace was established on Dropbox (San Francisco, CA) to share relevant literature on existing EUS curricula, learning curves, and evidence supporting current EUS applications. This space was made accessible to all working group members. Subsequently, the working group leads (authors DK and PO) used FluidSurveys (Ottawa, ON) to distribute a series of anonymous questionnaires to the members of the EUS Curriculum Working Group. Group leads DK and PO developed the surveys through collaboration whereby differences in opinion were resolved through discussion (with a general preference to include items rather than remove them so as to offer the participating members as much choice as possible). Each survey was available for 7–10 days, and at least two reminders were sent out. The first round of six surveys was completed over 4 months from February 2, 2016, to June 4, 2016.
In the first survey, participants were asked to state whether the applications listed should be considered as “core,” “elective,” or “not applicable” when considering a Canadian point-of-care ultrasound (POCUS) EM curriculum. We used a modified Delphi method whereby 80% represented sufficient support for any given EUS application to be included in the core EUS curriculum. The 80% cutoff was based on Lynn’s suggestion that at least 80% of experts must agree on an item to achieve content validity when there are at least 10 experts participating in consensus development.Reference Lynn 15 To determine specific objectives and learning outcomes for these core applications, five subsequent surveys were developed where participants were asked whether the listed objectives should be included as part of a core EUS curriculum, with possible responses consisting of “yes,” “no,” and “maybe.” As with the determination of applications, an 80% cut-off was applied to these specific objectives (see Appendix B).
All of the survey results were presented to the CAEP EUC membership at CAEP16 (Quebec City, June 5, 2016), and a widespread discussion occurred. There was a particular focus on the applications that had received 60%–79% support for inclusion in the core EUS curriculum, with arguments made for and against their inclusion ranging from infrastructure and feasibility concerns to impact on patient care and departmental flow. After this discussion, a final anonymous survey was sent out and open from June 7 to June 14, 2016 as to whether these remaining items should be included in the core EUS curriculum.
The initial surveys also included a preliminarily exploration of the ways in which the core EUS curriculum should be delivered in terms of learning experiences, supervision, and assessment. The results of these items are included as secondary items in this report.
RESULTS
The EUS Curriculum Working Group was made up of 35 members representing institutions from every EM residency program across the country. The survey response rate varied between 18 (51%) and 32 (91%) members, with the highest response rate on the first survey. For this study, the 80% level of agreement was based on the number of respondents to the respective survey.
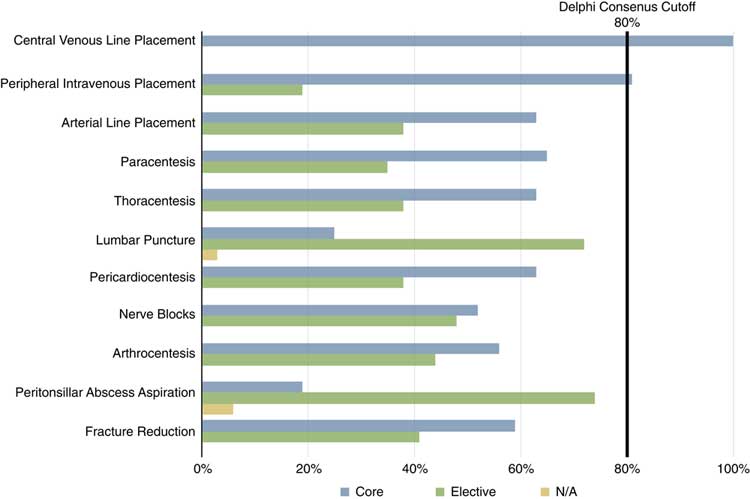
The following EUS applications met 80% support after the first round: FAST, identification of AAA, identification of IUP by transabdominal approach, thoracic ultrasound, focused cardiac ultrasound, and ultrasound-guided vascular access (Figures 1 and 2).
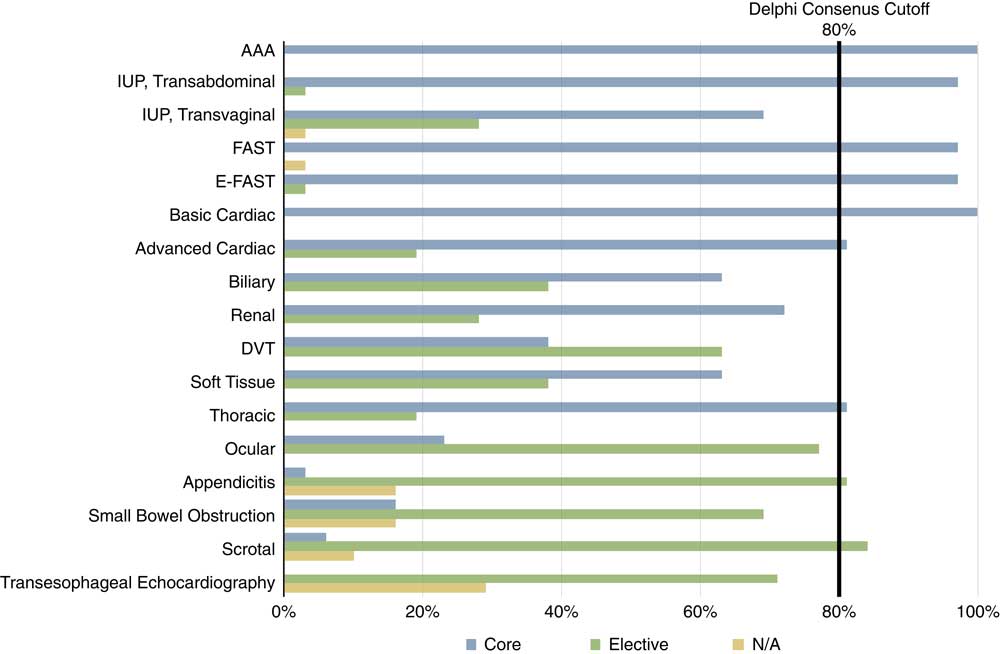
Figure 1 Diagnostic emergency ultrasound applications into core, elective, and inapplicable applications when considering a national Canadian emergency ultrasound curriculum.
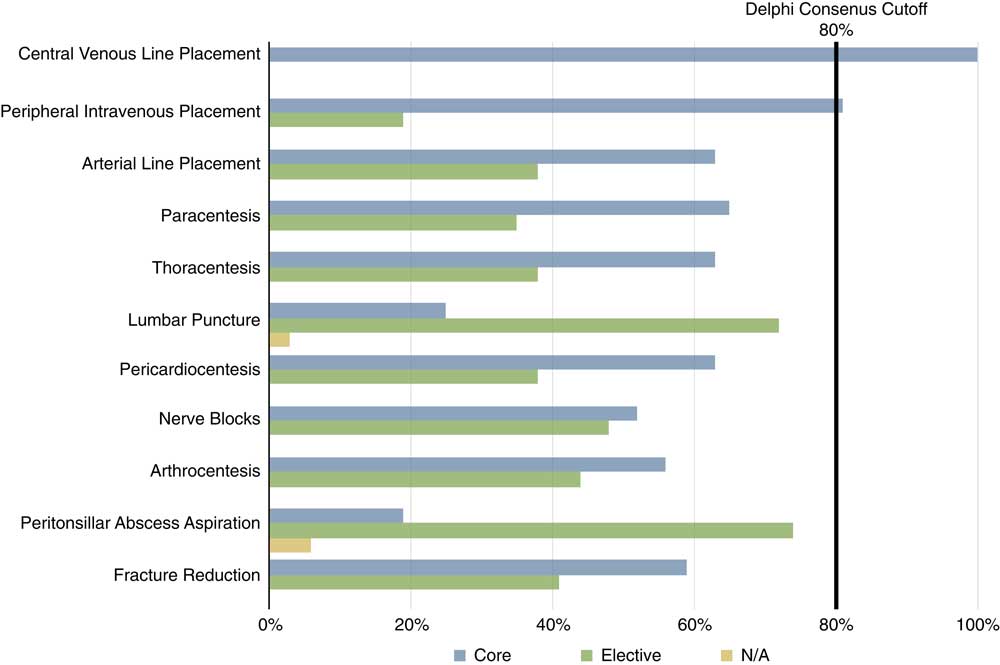
Figure 2 Procedural emergency ultrasound applications into core, elective, and inapplicable applications when considering a national Canadian emergency ultrasound curriculum.
Four applications that initially received 60%–79% support still failed to reach 80% support after a second round of voting, despite in-person and online discussion of identification of cholelithiasis and cholecystitis, hydronephrosis, abscess and foreign body, and IUP by transvaginal approach (Figure 3).
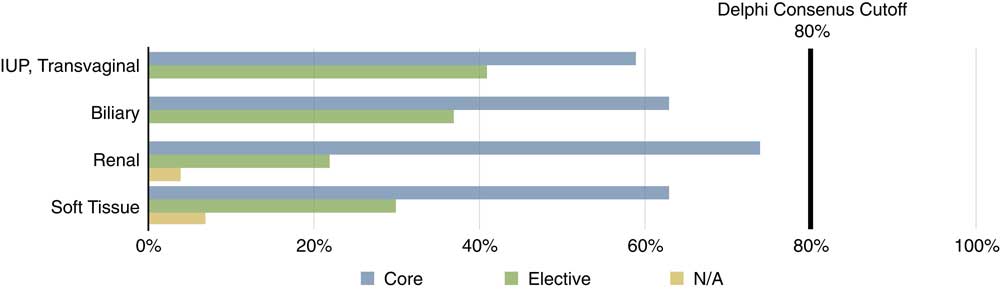
Figure 3 Diagnostic emergency ultrasound applications initially receiving 60-79% support as core applications into core versus not core applications when considering a national Canadian emergency ultrasound curriculum. N=27.
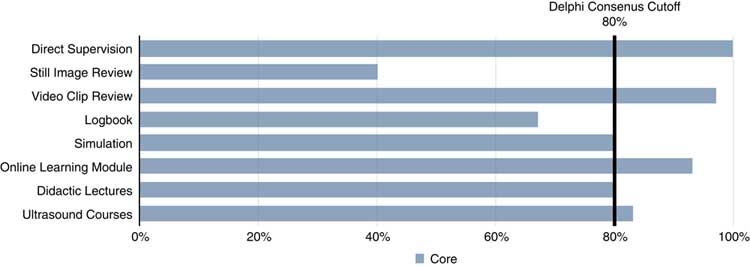
Figure 4 breaks down acceptable methods of delivering EUS training and teaching to Canadian EM residents. Using the 80% cut-off, acceptable methods of training include direct supervision, video clip review, simulation, online learning modules, didactic lectures, and ultrasound courses.
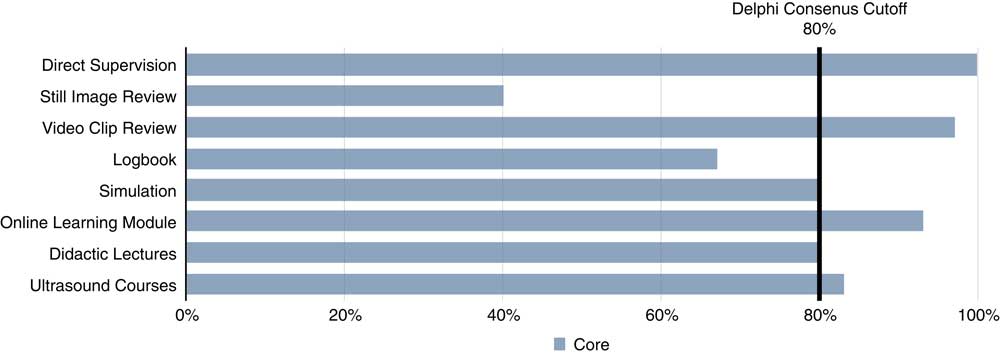
Figure 4 Acceptable methods of delivering emergency ultrasound training and teaching to Canadian emergency medicine residents.
The working group also recognizes the need for frequent review and updating of the core EUS curriculum given the increasing adoption of POCUS in undergraduate training; 97% (29 of 30) agreed that an EUS curriculum will need to rapidly evolve over the next 5 to 10 years.
DISCUSSION
The proposed core EUS curriculum lays a strong foundation for quality and growth of EUS in Canadian EM training programs. Similar to other established EUS curricula, this first iteration centers on emergent and potentially life-saving applications.Reference Akhtar, Theodoro and Gaspari 16 Although FAST, identification of AAA, identification of IUP by transabdominal approach, basic cardiac ultrasound for identification of pericardial effusion, and ultrasound-guided vascular access are already commonly taught throughout Canadian EM training programs, the addition of thoracic and focused cardiac ultrasound represents substantial growth in what are considered core applications. Indications for thoracic ultrasound include the detection of pneumothorax, pleural effusion/hemothorax, and interstitial lung syndrome. Indications for focused cardiac ultrasound include the detection of marked left or right ventricular enlargement, global cardiac systolic function, and volume status. The working group members acknowledged that the adoption of these additional applications may pose logistical challenges (related to time and resource constraints) but believe that through cooperation and support from training programs, these challenges can be overcome.
Additionally, the Curriculum Working Group has identified important EUS applications that, although not included in this initial core curriculum, have been shown to have high accuracy and may have a positive impact on patient care and ED flow (identification of cholelithiasisReference Ross, Brown and McLaughlin 17 and cholecystitis,Reference Summers, Scruggs and Menchine 18 hydronephrosis,Reference Smith-Bindman, Aubin and Bailitz 19 abscess and foreign body,Reference Subramaniam, Bober and Chao 20 and IUP by transvaginal approach.Reference Mateer, Valley and Aiman 21 ) The working group endorses these applications as important to the practice of EM in Canada. These applications will be taken into strong consideration for the second iteration of the Core EUS Curriculum. While it is likely that each institution will want to determine which, if any, additional applications can be taught on an elective basis, the working group strongly felt that the proposed core EUS curriculum could and should be implemented as a minimum standard for both EM training streams (see Appendix C for supporting evidence for each application).
Given the increased number of proposed core EUS applications, and with the concept of patient zero in mind, 22 the working group members felt it important that all EM trainees begin developing EUS skills as early as possible in their postgraduate training. This has implications for both EM training programs, but perhaps will be most challenging for CFPC trainees who already face a dense curriculum in their third year of training. It is the working group’s recommendation that residents of CFPC-EM programs be introduced to EUS prior to their third year of residency. This could be accomplished by encouraging all successful CFPC-EM applicants to undertake EUS training immediately after receiving confirmation of their third residency match.
The next steps will be to further define learning experiences as well as supervision and feedback methods. Emerging evidence on the nature of EUS learning curvesReference Blehar, Barton and Gaspari 23 combined with expert opinionReference Costantino, Burton and Tayal 24 and further consultation with the working group will assist in developing these components of the curriculum.
Our exploration of acceptable methods of training resulted in a surprisingly broad range of methods, including direct supervision, video clip review (indirect supervision), simulation, online learning modules, didactic lectures, and ultrasound courses. This is encouraging because regional disparities and differences will be best addressed through a flexible teaching model that uses a variety of instructional and supervisory methods.
The increasing role of ultrasound in undergraduate medical trainingReference Steinmetz, Dobrescu and Oleskevich 25 will have a direct impact on the core EUS curriculum, because many trainees entering residency will already possess some of the previously identified core skills. Several working group members belong to such institutions, with several being directly involved in this exciting work. Furthermore, as illustrated by the adoption of thoracic, advanced cardiac, and inferior vena cava assessment from the advanced or fellowship-trained userReference Fischer, Woo and Lee 10 to a core residency training expectation, EUS is in a state of rapid evolution. This reality highlights the need for regularly scheduled curriculum reviews and updates during the next 5 to 10 years. Through consultation with program directors and educators, the Curriculum Working Group hopes to deliver its first competency-based EUS curriculum in 2017.
LIMITATIONS
The EUS Curriculum Working Group attempted to include as broad of a national participation as possible, but it is plausible that certain institutions or regions were more represented than others, possibly biasing the results in favor of certain institutions over others. Furthermore, participation rates for each of the survey rounds ranged from 51% to 91%. This is likely due to various factors, including survey fatigue and ambivalence about the application in question. The working group leads believe this was counterbalanced by the well-attended in-person meeting at CAEP16 where the majority of working group members were present. It is also unclear to what extent that working group members reviewed the provided literature on the topics of EUS learning curves and curriculum design.
CONCLUSIONS
The Core EUS curriculum should include the following applications: FAST, identification of AAA, identification of IUP by transabdominal approach, thoracic ultrasound, focused cardiac ultrasound, and ultrasound-guided vascular access. The RCPSC and the CFPC should explore the adoption of these training objectives into the broader objectives and competency-based assessment of their EM residency training.
RECOMMENDATIONS
Given the increase in the number of proposed core EUS applications, the working group members felt it important that all EM trainees begin developing EUS skills early in their postgraduate training, ideally in their first year. At the very least, residents of CFPC-EM programs should be introduced to EUS prior to their third residency year.
Training sites should share their teaching resources for the aforementioned curriculum, to expedite adoption and minimize duplication. In such a partnership, all work should be attributed to the creators of the learning material (and their respective institutions).
Training sites should continue to advance patient care and push the boundaries of EUS beyond the aforementioned core curriculum. This can be accomplished through the addition of elective EUS applications that are deemed important to the local context. Future iterations of this position statement will need to be undertaken frequently to keep pace with the likely expanding set of EUS skills required in residency training.
Keywords: emergency ultrasound, curriculum, residency
Acknowledgements: We sincerely thank all of the members of the Curriculum Working Group of the CAEP Emergency Ultrasound Committee.
Competing interests: None declared.
SUPPLEMENTARY MATERIAL
To view supplementary material for this article, please visit https://doi.org/10.1017/cem.2017.44