The disease burden from stroke is one of the most significant, worldwide. According to a recent study, stroke continues to be the second leading cause of death globally and the third leading cause of death and disability(Reference Feigin, Stark and Johnson1). In 2019, 6·55 million people died from stroke globally(Reference Roth, Mensah and Johnson2), compared with 2·19 million deaths and 45·9 million disability-adjusted life years in China(Reference Ma, Li and Wang3). It is estimated that there are approximately 2·4 million new strokes and 1·1 million stroke-related deaths in China each year, with 11·1 million stroke survivors alive at any given time(Reference Wang, Jiang and Sun4). Of these, 87·9 % of ischaemic stroke (IS)’ disability-adjusted life years and 89·5 % of haemorrhagic stroke (HS)’ disability-adjusted life years are due to potentially modifiable risk factors, demonstrating the great potential for reducing the burden of stroke by reducing risk factor exposure(Reference Feigin, Nichols and Alam5).
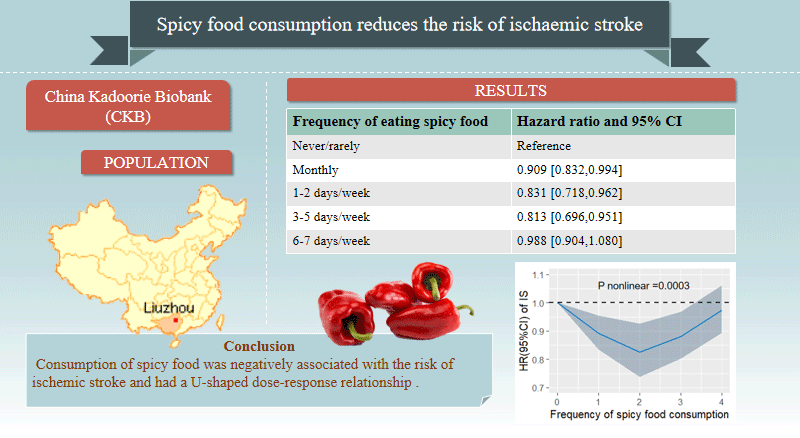
Spices not only enhance the flavour, aroma and colour of food and beverages but also have preventive effects on acute and chronic diseases(Reference Jiang6–Reference Li, Cui and Jin9). Previous studies have demonstrated that spices possess antioxidant, antiviral, antihypertensive, anti-diabetic and other beneficial effects(Reference Singh, Rao and Nandal10,Reference Nilius and Appendino11) . Several previous studies have investigated the association between spicy food and specific metabolic diseases, indicating that increased consumption of spicy food is inversely correlated with obesity(Reference Shi, Riley and Taylor12), hypertension(Reference Wang, Chen and Shen13), diabetes(Reference Zhao, Li and Li14) and serum cholesterol(Reference Xue, He and Yu15). Additionally, the consumption of spicy food can reduce the risk of death from CVD, including stroke mortality(Reference Lv, Qi and Yu16–Reference Bonaccio, Di Castelnuovo and Costanzo19). A cohort study conducted in western China discovered an association between spicy food consumption and a reduced risk of stroke among individuals with lower Dietary Approaches to Stop Hypertension (DASH) scores(Reference Chen, Tang and Wu20), and another study conducted by the China Kadoorie Biobank (CKB) revealed that the consumption of spicy food was independently linked to a decreased incidence of adverse cardiovascular events among Chinese adults with diabetes(Reference Li, Chang and Lai21). However, both studies were limited to a specific population, and the frequency of spicy food consumption and the incident stroke were not thoroughly examined.
Therefore, to further explore the relationship between the frequency of spicy food consumption and the risk of stroke in the general population, we prospectively followed approximately 50 000 people for 10 years in Liuzhou, China.
Methods
Study population
The CKB is one of the largest chronic disease cohorts in China, to investigate the impact of various lifestyle, genetic and environmental factors on the process of developing and dying from chronic diseases. The CKB study design, survey technique and demographic have all been detailed elsewhere(Reference Chen, Chen and Collins22,Reference Li, Lv and Guo23) . The current study used data collected in Liuzhou City, one of ten areas assessed by the CKB cohort. In summary, the study included 50 174 people aged 30–79 years between August 2004 and January 2008. All investigation operations were carried out in accordance with standardised processes and with the assistance of skilled and competent experts. In this study, individuals with cancer (n 386), stroke (n 1357) and heart disease (n 2294) at baseline, as well as participants lost to follow-up (n 329), were excluded from the analysis. With follow-up through 31 December 2017, 45 908 participants were included in the overall stroke analysis (Fig. 1). The study was conducted in accordance with the guidelines of the Declaration of Helsinki, and all procedures involving participants were approved by the Ethics Committee of the University of Oxford, UK (approval number: 025–04, 3.2.2005; University of Oxford, the UK), and the Ethics Committee of the Chinese Centre for Disease Control and Prevention (approval number: 005/2004, 9.7.2004; Beijing, China)(Reference Hou, Li and Zhu24). Written informed consent was obtained from all participants.
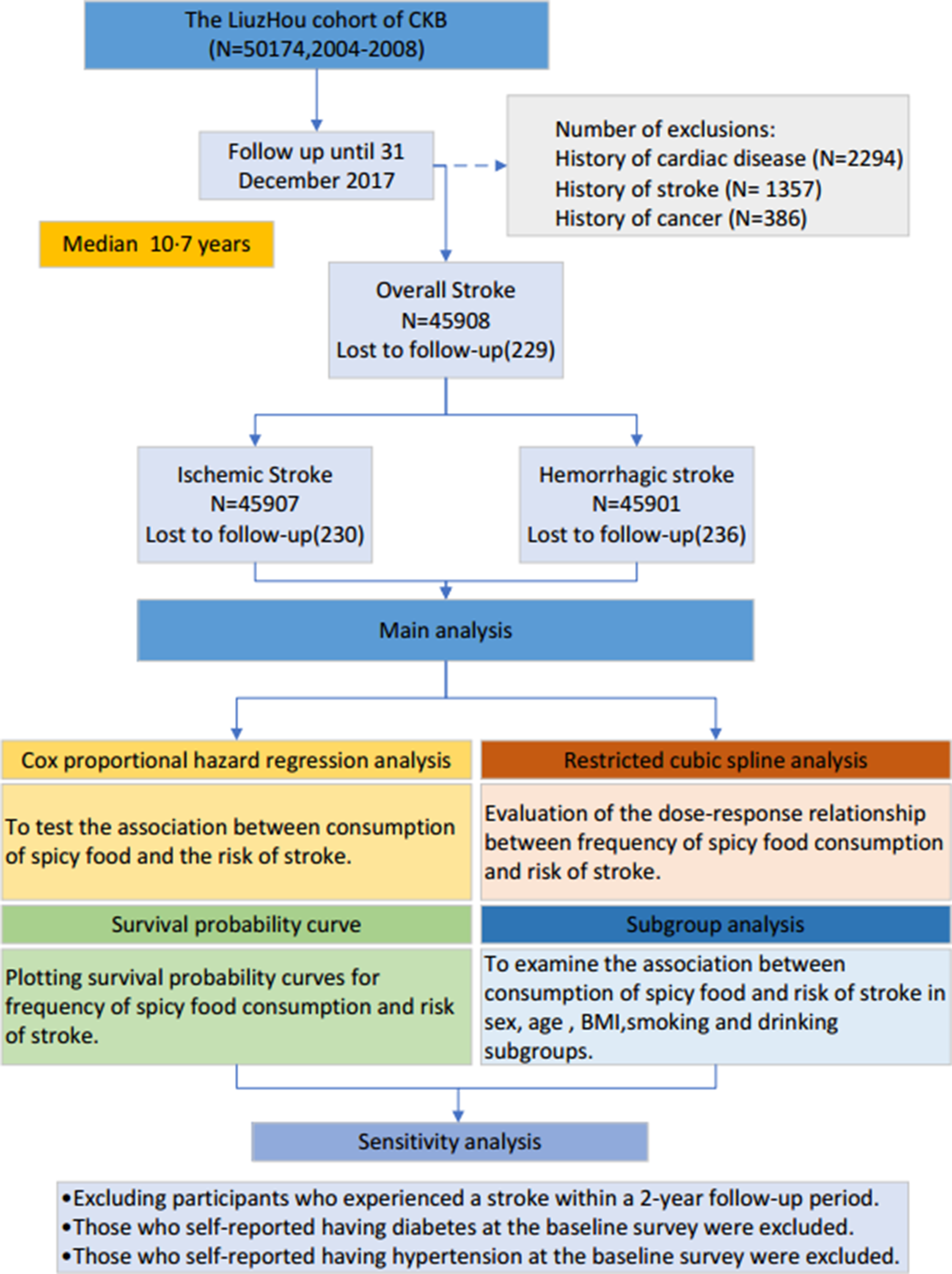
Fig. 1. Flow chart of Liuzhou cohort participants included in the analysis.
Assessment of spicy food consumption
Spicy food intake referred to the direct consumption of fresh chilli peppers; the addition of fresh/dried chilli peppers, chilli oil/sauce/paste, curry or other ‘hot’ spices when cooking; or the addition of chilli oil/sauce/paste to food when eating(Reference Chan, Millwood and Kartsonaki8). During the baseline survey, participants were asked ‘During the past month, about how often did you eat hot spicy food?’ Answers include ‘never/almost never’, ‘only occasionally’, ‘1–2 days/week’, ‘3–5 days/week’, and ‘6–7 days/week’.
Follow-up and outcome measures
In the Liuzhou cohort of the CKB study, the vital status of each participant was identified chiefly by using linkage with the local disease and death registries and the health insurance system(Reference Chen, Lee and Chen25). The primary diseases examined in this study were stroke (ICD-10: I60-I61, I63-I64), and the secondary outcomes were IS (ICD-10: I63) and HS (ICD-10: I61). Participants were enrolled from the date of enrolment until the earliest occurrence of the outcome, death (from any cause), failure to follow-up or the end date of the study (31 December 2017).
Assessment of covariates
We obtained covariates through baseline surveys, including socio-demographic characteristics (sex, age, education level, occupation, marital status and household income), lifestyle behaviours (smoking, alcohol consumption, meat, fresh fruits, dairy products, fresh vegetables and eggs) and personal disease history (CHD, diabetes). Total physical activity can be quantified as MET hours per day, which is calculated by multiplying the MET value assigned to each activity by its duration, and then summing the results across all activities(Reference Bennett, Du and Bragg26). Overweight was defined as BMI ≥ 24·0 kg/m2 and obesity as BMI ≥ 28·0 kg/m²(Reference Chen and Lu27).
Statistical analysis
We calculated the baseline characteristics of study participants according to their frequency of spicy food consumption, categorising it into five groups. Continuous variables were described using means and standard deviations, while categorical variables were presented as percentages. Cox proportional hazard regression models were employed to estimate hazard ratios (HR) and 95 % CI for the association between spicy food consumption and incident stroke. The models were adjusted for covariates: model 1 was adjusted for sex and age (30∼, 40∼, 50∼, 60∼, 70∼). Model 2 was based on model 1, additionally adjusted for education background (illiterate and elementary, middle school, high school and above), household income (< 20 000 Yuan, ≥ 20 000 Yuan), occupation (non-retired, retired), marital status (married, widowed, separated/divorced/unmarried), BMI (underweight/normal, overweight, obesity), smoking (never smoker, ex-regular smoker/smoker), drinking (never drinker, ex-regular drinker/drinker) and total physical activity (quartile grouping) adjusted. On the basis of model 2, model 3 further adjusted for meat (daily, non-daily), fresh vegetable (daily, non-daily), fresh fruit (daily, 1–6 d/week, rarely), dairy product (1–7 d/week, rarely) and eggs intake (4–7 d/week, 1–3 d/week, rarely). Survival probability curves and log-rank tests were used to assess the survival probability of outcomes based on the frequency of spicy food consumption. Restricted cubic spline analysis was used to examine the dose–response relationship between the frequency of spicy food intake and the risk of stroke. Additionally, we conducted a stratified analysis of sex, age and BMI to further investigate this relationship. We conducted two sensitivity analyses: (I) excluding participants who experienced a stroke within a 2-year follow-up period; (II) those who self-reported having diabetes at the baseline survey were excluded. (III) Those who self-reported having hypertension at the baseline survey were excluded. All statistical analyses were conducted using R software (version 4.2.1). All statistical significance was set at P < 0·05.
Results
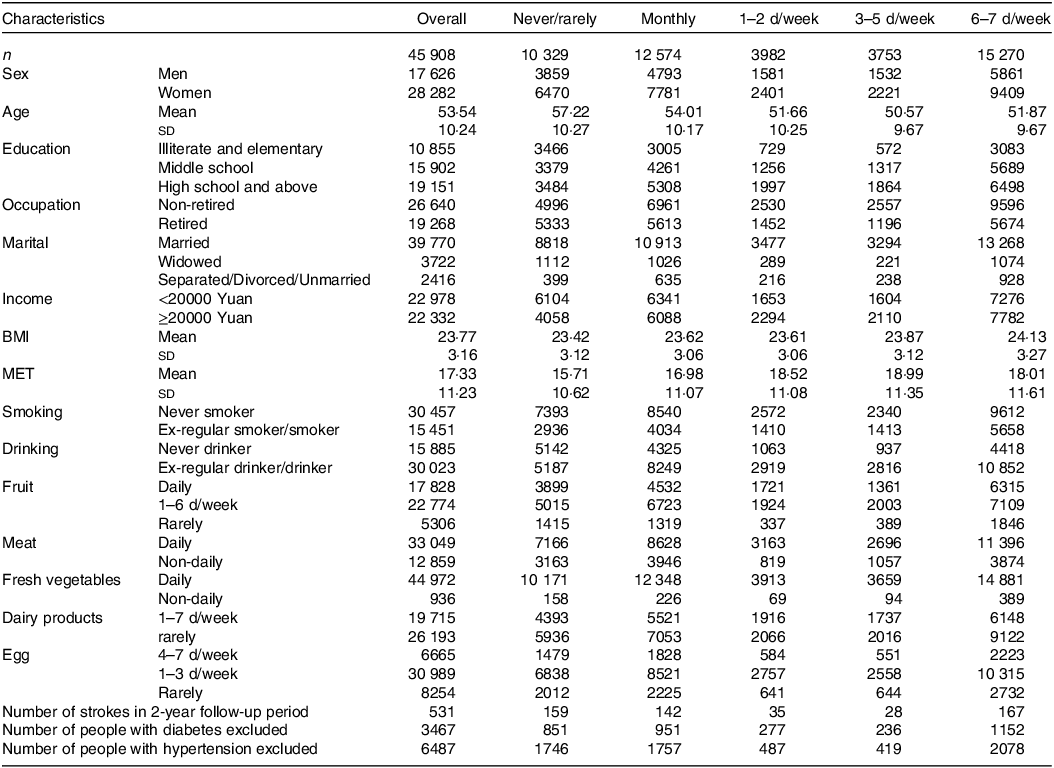
This study included a total of 45 908 participants. The mean age at baseline was 53·54 (sd 10·24) years, and 61·61 % of the participants were women. Compared with non-consumers of spicy food, individuals who regularly consumed spicy food were more likely to be women, younger, educated, not retired, married, non-smokers, frequent drinkers and have a higher BMI (Table 1). Over an approximate follow-up period of 450 000 person-years (median duration = 10·7 years), a total of 3967 strokes, 3494 IS and 516 HS, were observed.
Table 1. Distribution of baseline characteristics and frequency of spicy food consumption
(Mean values and standard deviations)
As shown in Table 2, participants who consumed spicy food monthly had a lower risk of stroke than those who did not consume spicy food (model 1: HR: 0·904, 95 % CI 0·832, 0·982, model 2: HR: 0·910, 95 % CI 0·836, 0·989, model 3: HR: 0·914, 95 % CI 0·841, 0·995) after adjusting for covariates. Similarly, participants who consumed spicy food 1–2 d per week had a lower risk of stroke (model 1: HR: 0·831, 95 % CI 0·726, 0·950, model 2: HR: 0·858, 95 % CI 0·749, 0·983, model 3: HR: 0·869, 95 % CI 0·758, 0·995) after adjusting for covariates. Similarly, participants who consumed spicy food 3–5 d per week had a lower risk of stroke (model 1: HR: 0·816, 95 % CI 0·707, 0·942, model 2: HR: 0·830, 95 % CI 0·717, 0·960, model 3: HR: 0·826, 95 % CI 0·714, 0·956) after adjusting for covariates. Results for IS were consistent with overall stroke, but the same results were not observed for HS.
Table 2. HR for stroke and subtypes adjusted for frequency of spicy food consumption
(Hazard ratios and 95 % confidence intervals)
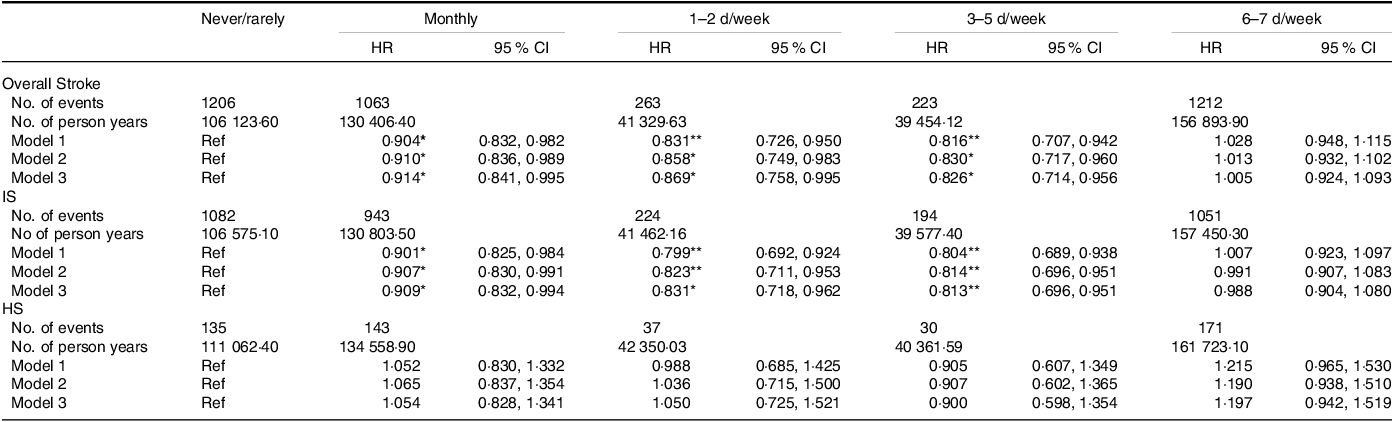
HR, hazard ratio; IS, ischaemic stroke; HS, haemorrhagic stroke.
P < 0·05 *
P < 0·01 **
P < 0·001 ***
As shown in Fig. 2, as the follow-up time increases, participants who never/rarely consumed spicy food had the lowest probability of survival, followed by those with monthly consumption, 6–7 d/week consumption and 1–2 d/week consumption, and the highest probability of survival was observed in the 3–5 d/week consumption group (P < 0·0001) (Fig. 2(a)). Similar findings were observed in incidence of IS (P < 0·0001) (Fig. 2(b)), but there was no significant association for consumption of spicy food and incidence of HS (P = 0·1100) (Fig. 2(c)). In addition, restricted cubic spline analysis showed that the frequency of spicy food consumption and the risk of stroke have a U-shaped dose–response relationship (Fig. 3) (P nonlinear = 0·0003 for overall stroke and IS). Similar findings were observed in three sensitivity analyses, which excluded participants with stroke during a 2 years follow-up period and participants with self-reported diabetes at baseline (online Supplementary Table S1–S3).
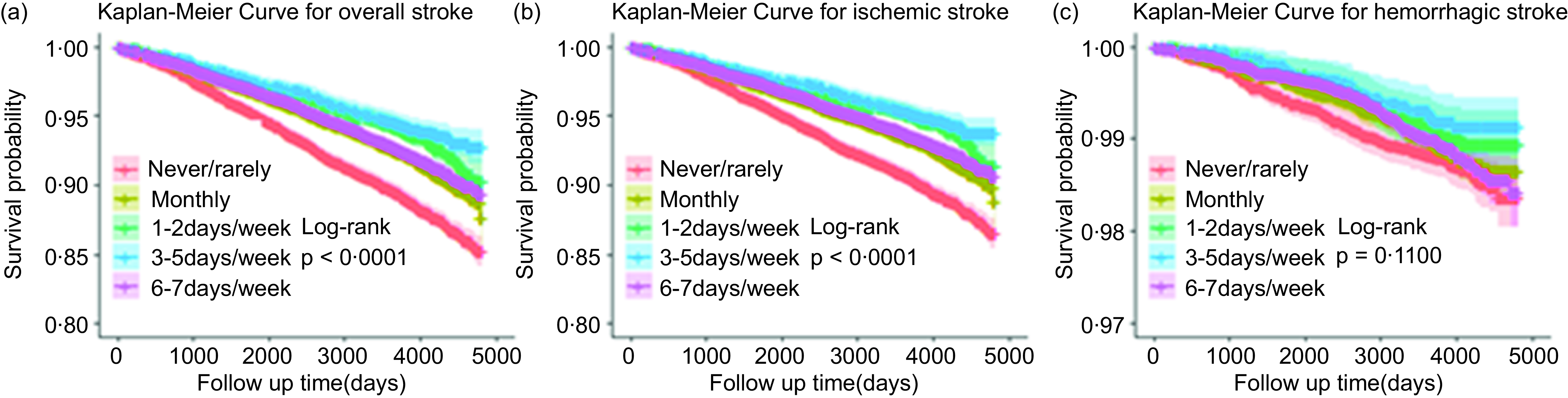
Fig. 2. Survival probability curves between the frequency of spicy food consumption and the risk of stroke occurrence.
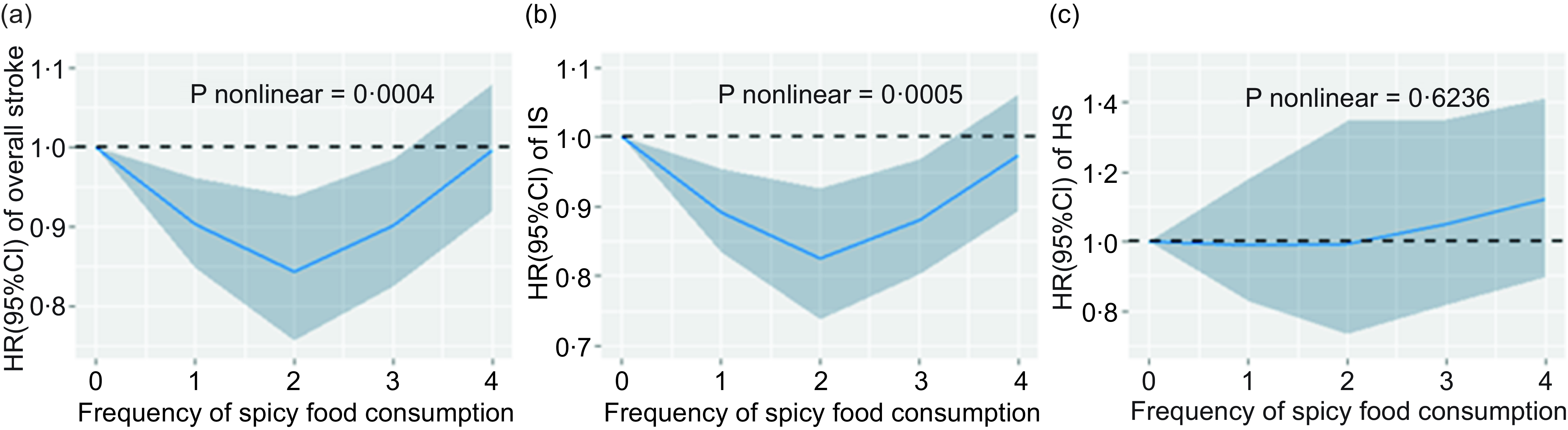
Fig. 3. Dose–response relationship between the frequency of spicy food consumption and the risk of stroke, 0: never/rarely, 1:1: monthly, 2:1–2 d/week, 3:3–5 d/week and 4:6–7 d/week
Figure 4 shows the results of the subgroup analysis. Regarding overall stroke, the HR for individuals consuming spicy food 3–5 d/week was 0·767 (95 % CI 0·620, 0·949) for men, compared with those who never/rarely consumed spicy food. In addition, the HR for individuals consuming spicy food 1–2 d/week was 0·796 (95 % CI 0·653, 0·971) for women compared with those counterparts. For participants under 60 years old, the HR for consuming spicy food monthly, 3–5 d per week, were 0·785 (95 % CI 0·681, 0·904) and 0·632 (95 % CI 0·507, 0·788), respectively, compared with participants who never/rarely consumed spicy food. For participants ≥ 60 years of age, the HR for consuming spicy food 1–2 d per week was 0·810 (95 % CI 0·671, 0·977) compared with those who never/rarely consumed spicy food. For underweight/normal and obese participants, the HR for consuming spicy food 3–5 d per week were 0·758 (95 % CI 0·600, 0·950) and 0·593(95 % CI 0·387, 0·911), respectively, compared with those who never/rarely consumed spicy food. Among participants who smoked, the HR for eating spicy food 3–5 d per week was 0·726 (95 % CI 0·577, 0·912) compared with those who never or rarely ate spicy food. Among participants who never drank alcohol, the HR for eating spicy food 1–2 d per week was 0·707 (95 % CI 0·545, 0·918) compared with those who never or rarely ate spicy food. In contrast, among participants who drank alcohol, the HR for those who ate spicy food monthly and those who ate spicy food 3–5 d per week was 0·880 (95 % CI 0·785, 0·986) and 0·792 (95 % CI 0·660, 0·951), respectively.
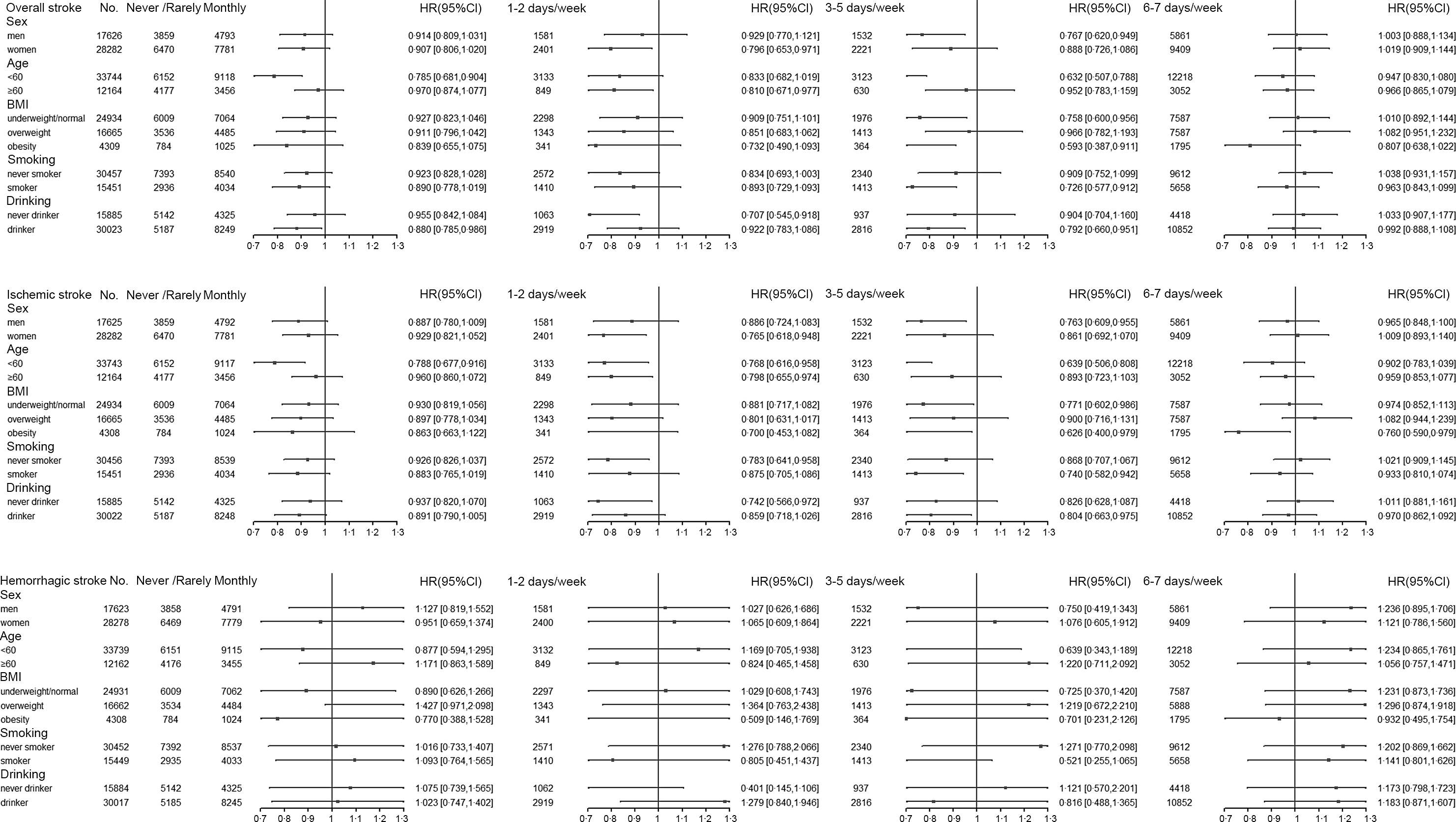
Fig. 4. Subgroup analysis of strokes.
In the case of IS, the HR for consuming spicy food 3–5 d/week was 0·763 (95 % CI 0·609, 0·955) for men compared with those who never/rarely consumed spicy food, and 0·765 (95 % CI 0·618, 0·948) for women who consumed 1–2 d/week compared with those who never/rarely consumed spicy food. The HR for monthly, 1–2 d per week and 3–5 d per week consumption of spicy food were 0·788 (95 % CI 0·677, 0·916), 0·768 (95 % CI 0·616, 0·958) and 0·639 (95 % CI 0·506, 0·808), respectively, for participants aged < 60 years compared with those who never/rarely consumed spicy food. The HR for participants aged ≥ 60 years who consumed spicy foods 1–2 d per week was 0·798 (95 % CI 0·655, 0·974) compared with those who never/rarely consumed spicy food. The HR for consumption of spicy food 3–5 d per week was 0·771 (95 % CI 0·602, 0·986) for participants who were underweight/normal weight compared with those who never/rarely consumed spicy food. The HR for obese participants consuming spicy food 3–5 d per week and 6–7 d per week compared with those who never/rarely consumed spicy food were 0·626 (95 % CI 0·400, 0·979) and 0·760 (95 % CI 0·590, 0·979), respectively. Among never-smoking participants, the HR for eating spicy food 1–2 d per week was 0·783 (95 % CI 0·641, 0·958) compared with participants who never or rarely ate spicy food. In contrast, among participants who smoked, the HR (95 % CI) for those who ate spicy food 3–5 d per week was 0·740 (95 % CI 0·582, 0·942). Among participants who never drank alcohol, the HR for eating spicy food 1–2 d per week was 0·742 (95 % CI 0·566, 0·972) compared with participants who never or rarely ate spicy food. In contrast, among participants who drank alcohol, the HR for those who ate spicy food 3–5 d per week was 0·804 (95 % CI 0·663, 0·975).
Discussion
The study estimates the associations between the consumption of spicy food and the risk of stroke. We found the consumption of spicy food was negatively associated with the risk of IS and had a U-shaped dose–response relationship with the risk of IS. In addition, individuals who consumed spicy food 3–5 d/week had a significantly lowest risk of IS. For obese participants, consuming spicy food ≥ 3 d per week was inversely associated with the risk of IS.
In this study, the proportion of people who ate spicy food 6–7 d/week was 33·26 % (15270/45908), lower than the proportion in Hunan Province (99·4 %, n 50 192) but higher than the proportion in Zhejiang Province (2·7 %, n 1276)(Reference Sun, Lv and Chen28). The reasons may be due to the subtropical monsoon climate, which is rainy and humid and more suitable for spicy food(Reference Wang, Cheng and He29). For example, previous meta-analysis of four prospective cohort studies from the USA, Italy, Iran and China found that regular consumption (≥ 1 d/week) of spicy food was associated with a 12 % reduction in the risk of all-cause mortality and was negatively associated with the risk of death from ischaemic heart disease(Reference Ofori-Asenso, Mohsenpour and Nouri30). In a prospective cohort study of 22 160 people from western China with a mean follow-up of 45·5 months, the consumption of spicy food appeared to be associated with a lower risk of stroke only in those with lower DASH scores(Reference Chen, Tang and Wu20). Another CKB cohort of 26 163 diabetic patients with a median follow-up of 8·5 years found that the consumption of spicy food was independently associated with a reduced incidence of adverse cardiovascular events in Chinese adults with diabetes(Reference Li, Chang and Lai21). The results of these two studies are consistent with our finding. The probable cause is the action of capsaicin.
The transient receptor potential capsaicin 1 receptor (TRPV1), also known as the capsaicin receptor, is widely distributed in tissues such as the brain, cardiovascular system, vascular endothelial cells and macrophages. It is a non-selective cation channel with a preference for Ca2+(Reference Reyes-Escogido Mde, Gonzalez-Mondragon and Vazquez-Tzompantzi31). Activation of TRPV1 by dietary capsaicin may directly reduce stroke events through its anti-atherogenic effects. For example, activation of TRPV1 induced autophagy through the APM-activated protein kinase signalling pathway, thereby inhibiting foam cell formation in vascular smooth muscle cells(Reference Li, Yin and Liu32). This process also involved the activation of other signalling pathways, including the divalent cation calcium (Ca2+)/phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt)/endothelial nitric oxide synthase (eNOS)/nitric oxide (NO) /rescue of SIRT1 and inhibition of the NF-κB signalling pathway(Reference Randhawa and Jaggi33–Reference Zhang, Zhou and Chen36). Meanwhile, TRPV1 also reduces mitochondrial reactive oxygen species (ROS) production through the protein kinase A (PKA)/uncoupling protein 2 (UCP2) pathway(Reference Munjuluri, Wilkerson and Sooch37). Activation of these pathways helps to inhibit the inflammatory response of endothelial cells and promotes vasodilation and angiogenesis, thereby slowing the progression of atherosclerosis. In addition, TRPV1 can also regulate the expression of atp-binding cassette transporter A1 and LDL-related protein 1, reduce the increase in cholesterol efflux and decrease in uptake in cells, thereby delaying the generation of plaques(Reference Ma, Zhong and Zhao38). However, prolonged or repeated application of capsaicin may induce channel dephosphorylation of calmodulin phosphatase and channel phosphorylation of PKA, thereby causing desensitisation of TRPV1, resulting in insensitivity of TRPV1 to capsaicin(Reference Mohapatra and Nau39,Reference Iftinca, Defaye and Altier40) . This may explain why eating spicy food 6–7 d per week did not prevent stroke and why the dose–response relationship was U-shaped.
Eating spicy food 1–2 d/week was negatively associated with stroke in women, while men needed to eat 3–5 d/week, which may be related to the action of sex hormones in women. Previous studies have found that oestradiol exerts a protective effect against atherosclerosis by preventing monocytes from adhering to the vascular system, inhibiting the recruitment of inflammatory cells, promoting cholesterol efflux from endothelial cells and decreasing the number of vascular endothelial cell-derived foam cells(Reference Bolego, Cignarella and Staels41,Reference Gasbarrino, Di Iorio and Daskalopoulou42) . It may be that oestrogen and capsaicin work together in women to exert a protective effect against IS even when they eat less spicy food. We found a significant negative association between eating spicy food and IS in people aged < 60 years. A person’s energy expenditure is most stable between the ages of 20 and 50 and does not begin to decline until after age 60(Reference Pontzer, Yamada and Sagayama43). This difference could influence how their bodies process and respond to the bioactive compounds in spicy food, such as capsaicin. Further research is needed to determine the underlying mechanisms behind this discrepancy.
Obesity is an independent risk factor for stroke(Reference Lu and Hajifathalian44). The HR for stroke increased by 1·18 (1·14, 1·22) for every 5 kg/m2 increase in BMI(Reference Lu, Hajifathalian and Ezzati45). An imbalance of adipokines, caused by the production of pro-inflammatory adipokines from visceral adipose tissue, is one of the causes of atherosclerosis induced by obesity(Reference Lovren, Teoh and Verma46). Capsaicin successfully reduced adipokine production and modulated macrophage behaviour in the adipose tissue of mice with obesity by activating TRPV1 channels to induce Ca2+ influx and inhibiting the down-regulation of TRPV1 expression(Reference Zhang, Yan Liu and Ma47,Reference Hsu and Yen48) . Population studies have shown that capsaicin controls obesity by increasing energy expenditure, promoting fat oxidation, reducing fat formation, suppressing appetite and enhancing satiety(Reference Whiting, Derbyshire and Tiwari49). A nationwide prospective study involving 12 970 Chinese adults revealed a negative association between chilli intake and the risk of overweight/obesity(Reference Shi, Riley and Taylor12). Furthermore, our study confirmed that consuming spicy food ≥ 3 d/week provided protection against IS in individuals with a BMI ≥ 28·0, indicating that individuals with obesity may benefit from increasing their intake of spicy food to reduce the risk of IS.
Our study has several strengths. It was prospective cohort study with a median follow-up time of 10·7 years, a large sample size and a low rate of loss to follow-up, adjusted for known and potential confounders, including socio-demographic characteristics (sex, age, etc.), lifestyle (smoking, alcohol consumption, etc.) and dietary factors (meat, eggs, etc.). Several limitations should be acknowledged in our study. First, the use of FFQ for assessing spicy food intake may introduce potential inaccuracies in quantifying actual consumption, as the FFQ primarily captured frequency rather than precise quantities consumed. Furthermore, we were unable to directly account for variations in the amount of spicy food consumed per body weight, particularly between men and women, due to data limitations. Additionally, spiciness is a subjective perception, making it challenging to establish precise causal relationships. In addition, our study did not directly investigate salt intake, which is a dietary factor associated with stroke risk, nor did it further investigate the effects of egg and meat consumption on CVD. In conclusion, further research is warranted to explore the mechanisms underlying the potential effects of capsaicin on stroke risk, considering these limitations.
Conclusions
Spicy food consumption was negatively associated with the risk of IS in a southern Chinese population, with a U-shaped dose–response relationship with risk of IS. However, there was no significant association observed between the consumption of spicy food and the incidence of HS. The consumption of spicy food ≤ 5 d/week was associated with a reduced risk of IS, showing the strongest protective effect in frequency of 3–5 d/week consumption. Obesity people may benefit from a higher frequency of consuming spicy food. More future research is needed to reveal the protective mechanisms of spicy food.
Acknowledgements
The most important acknowledgement is to the participants in the study and the members of the survey teams in Liuzhou regional centre, as well as to the project development and management teams based at Beijing and Oxford.
This work was supported by grants (82192900, 82192901, 82192904, 81390540, 91846303) from the National Natural Science Foundation of China, grants (2016YFC0900500) from the National Key Research and Development Program of China, grants from the Kadoorie Charitable Foundation in Hong Kong and grants (202922/Z/16/Z, 088158/Z/09/Z, 104085/Z/14/Z) from Wellcome Trust in the UK.
P. P. and D. S.: Methodology, project administration, funding acquisition and conceptualisation. J. L., J. T., X. T., N. C., L. W., J. L., R. P. and T. Z.: Investigation, data curation and validation. J. L.: Software, formal analysis, visualisation, writing – original draft and writing – review and editing. C. X.: Formal analysis, investigation, visualisation and writing – original draft. L. S.: Conceptualisation, methodology, formal analysis, writing – review and editing and resources. L. Z.: Conceptualisation, methodology, formal analysis, investigation, resources, writing – review and editing, supervision, project administration and funding acquisition.
The authors declare that there is no conflict of interest.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114524000229