Fast food is food that can be prepared quickly and easily and is sold in restaurants and snack bars as a quick meal or to be taken out(Reference De Vogli, Kouvonen and Gimeno1,Reference Sturm and Datar2) and often consists of meals such hamburgers and chips(3). However, it should be noted that fast-food products likely vary considerably across countries and cultures.(3). Currently, fast-food consumption is on the rise globally, especially among adolescents in both low- and middle-income countries (LMIC) and high-income countries (HIC)(Reference Janssen, Davies and Richardson4,Reference Bauer, Larson and Nelson5) . Fast food often consists of poor nutrition. For example, one study carried out by Heart UK identified that many UK high street restaurants and fast-food chains serve meals with four times the UK’s national maximum daily recommended levels of saturated fat in a single meal(6). Furthermore, fast-food consumers are known to have higher intakes of energy, fat, SFA, trans fatty acids, added sugar and Na, as well as lower intakes of fibre, macronutrients and vitamins(Reference Jaworowska, Blackham and Davies7).
Research has shown that fast-food consumption is associated with increased risk for physical conditions such as obesity, insulin resistance and elevated total cholesterol(Reference Jaworowska, Blackham and Davies7), while some studies have shown that it can also negatively impact mental health. For example, one study in 13 486 Iranian children and adolescents found that fast-food consumption may increase the risk for psychiatric distress and violent behaviours(Reference Zahedi, Kelishadi and Heshmat8). Other research has identified a link between fast-food consumption and depression(Reference Sánchez-Villegas, Toledo and De Irala9) or suicide attempts(Reference Jacob, Stubbs and Firth10). Owing to these detrimental health outcomes, it is important to identify risk factors of fast-food consumption in order to implement effective strategies to reduce this behaviour.
One potentially important but understudied correlate of fast-food consumption is food insecurity. Food insecurity is a condition in which households lack access to adequate food because of limited money or other resources(Reference Gundersen and Ziliak11). Although not all individuals in food-insecure households experience hunger, severe food insecurity can lead to hunger. The prevalence of food insecurity has been reported to be high in both LMIC and HIC. For example, the prevalence of food insecurity in the USA in 2019 has been estimated to be 10·5 %(12). Food insecurity may lead to fast-food consumption as people tend to shift to more energy-dense but less nutritious food when food is scarce(Reference Pilgrim, Barker and Jackson13). Specifically, food-insecure people may prefer energy-dense food to compensate for times when food is scarce. Alternatively, increasing cravings for high-energy foods may be induced as a coping strategy for stress associated with food insecurity(Reference Yau and Potenza14).
However, to date, there are only a few studies specifically on this topic across all age groups and all have been conducted in HIC. For example, in one study including 4746 multi-ethnic middle- and high-school students in the USA, it was found that food-insecure youths reported eating more fast food but fewer family meals and breakfasts per week than did youths who are food secure(Reference Widome, Neumark-Sztainer and Hannan15). In another study including 2564 Australian households, it was found that having run out of money to buy food was associated with increased likelihood of purchasing fast food from chain restaurants on a weekly basis(Reference Burns, Bentley and Thornton16).
The co-occurrence of food insecurity and fast-food consumption in young people is of particular concern as both are detrimental to health and both have been shown to track across the lifespan leading to an increased risk for adverse health outcomes even in adulthood(Reference Movassagh, Baxter-Jones and Kontulainen17,Reference Lee, Gundersen and Cook18) . Moreover, studying this association among adolescents is of particular importance as adolescence is a crucial life stage characterised by dramatic modifications in lifestyle patterns. These modifications include unhealthier food choices and eating outside the home (mainly at fast-food restaurants), amongst others(Reference AL Faris, Al-Tamimi and Al Jobair19–Reference Nielsen, Siega-Riz and Popkin21). Therefore, the aim of the present study was to investigate the association between food insecurity and fast-food consumption in adolescents aged 12–15 years from sixty-eight countries, representing all economic settings.
Methods
Publicly available data from the Global School Health Survey were analysed. Details on this self-administered survey can be found at http://www.who.int/chp/gshs and http://www.cdc.gov/gshs. Briefly, the Global School Health Survey was jointly developed by the WHO and the US Centers for Disease Control and Prevention, and other UN allies. The core aim of this survey was to assess and quantify risk and protective factors of major non-communicable diseases. The survey draws content from the Centers for Disease Control and Prevention Youth Risk Behavior Survey for which test–retest reliability has been established(Reference Brener, Collins and Kann22). The survey used a standardised two-stage probability sampling design for the selection process within each participating country. For the first stage, schools were selected with probability proportional to size sampling. The second stage involved the random selection of classrooms which included students aged 13–15 years within each selected school. All students in the selected classrooms were eligible to participate in the survey regardless of age. Data collection was performed during one regular class period. The questionnaire was translated into the local language in each country and consisted of multiple choice response options; students recorded their response on computer scannable sheets. All Global School Health Surveys were approved, in each country, by both a national government administration (most often the Ministry of Health or Education) and an institutional review board or ethics committee. Student privacy was protected through anonymous and voluntary participation, and informed consent was obtained as appropriate from the students, parents and/or school officials. Data were weighted for non-response and probability selection.
From all publicly available data, we selected all nationally representative data sets that included the variables used in the current analysis. If there were more than two data sets from the same country, we chose the most recent data set. Thus, a total of sixty-eight countries were included in the current study. The characteristics of each country or survey are provided in Table 1. For the included countries, the survey was conducted between 2009 and 2017 and consisted of seven low-income (n 12 462), twenty-seven lower middle-income (n 67 333), twenty upper middle-income (n 72 861) and fourteen high-income (n 27 508) countries based on the World Bank classification at the time of the survey for the respective countries.
Table 1. Survey characteristics and prevalence of fast-food consumption and severe food insecurity by country
(Numbers and percentages)

* Restricted to those aged 12–15 years.
Fast-food consumption
Fast-food consumption was assessed with the question ‘During the past 7 d, on how many days did you eat food from a fast-food restaurant?’ with country-specific examples on fast-food restaurants. Those who consumed fast food on at least 1 d in the past 7 d were considered to be consumers of fast food(Reference Jacob, Stubbs and Firth10). The examples of fast food included in the questionnaire of each country are provided in online Supplementary material Table S1. However, it should be noted that the validity of the question on fast-food consumption has not been examined and thus is unknown.
Food insecurity (hunger)
Food insecurity (hunger) was assessed by the question ‘During the past 30 days, how often did you go hungry because there was not enough food in your home?’. Answer options were ‘never’, ‘rarely’, ‘sometimes’, ‘most of the time’ and ‘always’. A brief hunger screening tool based on a similar single question showed 85 % sensitivity and 80 % specificity compared with the Household Food Security Scale(Reference Kleinman, Murphy and Wieneke23). For some analyses, a dichotomised variable on severe food insecurity (hunger) was used (i.e. most of the time/always or else)(Reference Koyanagi, Stubbs and Oh24).
Control variables
The control variables included sex, age and BMI. Trained survey staff conducted measurement of weight and height. BMI was calculated as weight in kg divided by height in metres squared. Obesity and overweight were defined as >2 sd and >1 sd above the median for age and sex based on the 2007 WHO Child Growth reference, respectively, and adolescents who were below -2 sd were considered to be underweight(Reference Caleyachetty, Thomas and Kengne25). All other subjects were considered to be normal weight.
Statistical analysis
Statistical analyses were performed with Stata 14.2 (Stata Corp LP). We restricted the analysis to those aged 12–15 years as data on the exact age outside of this age range were not available and because most students were within this age range. Using the overall sample, we used logistic regression analysis to estimate the association between different levels of food insecurity (hunger) (independent variable) and fast-food consumption (dependent variable), while adjusting for age, sex, BMI and country. Adjustment for country was done by including dummy variables for each country in the model as in previous Global School Health Survey publications(Reference McKinnon, Gariépy and Sentenac26,Reference Vancampfort, Stubbs and Firth27) . We also conducted interaction analysis by including a product term (food insecurity × sex) in the regression analysis in order to assess whether associations differ by sex. Next, we conducted country-wise logistic regression analysis to assess the association between severe food insecurity (i.e. most of the time/always hungry) and fast-food consumption, while adjusting for age, sex and BMI. We focused on severe food insecurity (hunger) for this analysis as preliminary analysis showed that this level of food insecurity (hunger) is associated with particularly high odds for fast-food consumption. In order to assess between-country heterogeneity, we calculated the Higgins’s I 2 which represents the degree of heterogeneity that is not explained by sampling error with a value of <40 % often considered as negligible and 40–60 % as moderate heterogeneity(Reference Higgins and Thompson28). A pooled estimate (overall and by country-income level) was obtained based on country-wise estimates using meta-analysis with random effects. All variables were included in the regression analysis as categorical variables with the exception of age (continuous variable). Sampling weights and the clustered sampling design of the surveys were taken into account to obtain nationally representative estimates. Results from the logistic regression analyses are presented as OR with 95 % CI. The level of statistical significance was set at P < 0·05.
Results
A total of 180 164 adolescents aged 12–15 years (mean age 13·8 (sd 1·0) years; 50·8 % boys) were included in the analysis. The prevalence of fast-food consumption in the past 7 d overall was 50·1 %. Overall, the proportion of adolescents who went hungry due to lack of food at home in the past 30 d by frequency was: rarely 17·6 %; sometimes 24·5 %; most of the time 3·5 % and always 2·7 %. There was a wide range in the prevalence of fast-food consumption and severe food insecurity (i.e. most of the time/always hungry) by country with the ranges being 21·0 % (Pakistan) to 85·9 % (Qatar) and 0·9 % (Vietnam) to 17·1 % (Afghanistan), respectively, while the prevalence of severe food insecurity was particularly high in low-income countries (Table 1). The prevalence of fast-food consumption increased with greater frequency of food insecurity (hunger) (Fig. 1). Based on a multivariable logistic regression analysis, compared with no food insecurity (hunger), being hungry most of the time and always were associated with significant 1·25 (95 % CI 1·09, 1·44) and 1·31 (95 % CI 1·11, 1·54) times higher odds for fast-food consumption, respectively (Fig. 2). No significant interaction by sex was observed. The country-wise association between severe food insecurity (hunger) and fast-food consumption is shown in Fig. 3. Overall, the pooled estimate based on all sixty-eight countries was OR = 1·17 (95 % CI 1·08, 1·26) with a moderate level of between-country heterogeneity (I 2 = 50·2 %). The estimates pooled by country-income levels were significant in low-income countries (OR = 1·30; 95 % CI 1·05, 1·60), lower middle-income countries (OR = 1·15; 95 % CI 1·02, 1·29) and upper middle-income countries (OR = 1·26; 95 % CI 1·07, 1·49), but not in HIC (OR = 1·04; 95 % CI 0·88, 1·23), although a moderate level of between-country heterogeneity was present for all income levels (I 2 = 44·3–58·3 %) with the exception of low-income countries (I 2 = 0·0 %).
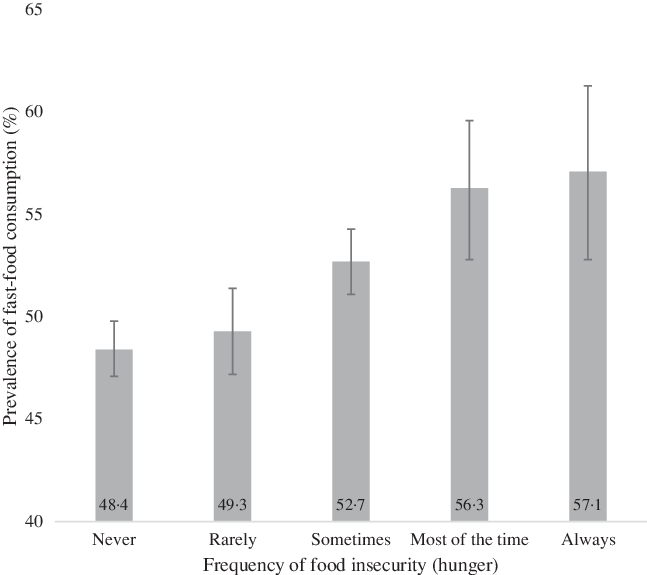
Fig. 1. Prevalence of fast-food consumption by frequency of food insecurity (hunger). Bars denote 95 % CI. P-value < 0·001 (χ 2 test).

Fig. 2. Association between frequency of food insecurity (hunger; exposure) and fast-food consumption (outcome) estimated by multivariable logistic regression. Reference category is no food insecurity. Model is adjusted for age, sex, BMI and country.

Fig. 3. Country-wise association between severe food insecurity (hunger) (exposure) and fast-food consumption (outcome) estimated by multivariable logistic regression. Models are adjusted for age, sex and BMI. Overall estimates were obtained by meta-analysis with random effects.
Discussion
In this large sample of children and adolescents from sixty-eight countries representative of all economic settings, it was found that the prevalence of fast-food consumption increases linearly with increasing severity of food insecurity (hunger). Based on a meta-analysis, it was found that severe food insecurity (i.e. hungry most of the time or always due to not enough food at home) was associated with 1·17 (95 % CI 1·08, 1·26) times higher odds for fast-food consumption compared with those without severe food insecurity. This association was significant in low-income countries (OR = 1·30), lower middle-income countries (OR = 1·15) and upper middle-income countries (OR = 1·26) but not in HIC.
The finding that food insecurity is associated with higher odds for fast-food consumption is in line with previous literature that has identified a positive association between food insecurity and fast-food consumption(Reference Widome, Neumark-Sztainer and Hannan15,Reference Burns, Bentley and Thornton16) . There may be several plausible pathways that explain why food-insecure adolescents are more likely to consume fast food. First, research has suggested that food-insecure families tend to choose more energy-dense food and this may be because energy-dense foods composed of refined grains, added sugars or fats may represent the lowest-cost option to the consumer(Reference Drewnowski and Specter29). Alternatively, this behaviour may be explained by a preference for energy-dense food owing to compensation for periods with scarcity of food or poor health literacy. Second, dietary habits and food insecurity track across the lifespan. Therefore, parents of food-insecure households may be more likely to have been food insecure in their childhood and have been consuming fast food often, and ingrained this habit in their offspring(Reference Movassagh, Baxter-Jones and Kontulainen17,Reference Lee, Gundersen and Cook18) . Third, those who are food insecure are more likely to suffer from mental health complications(Reference Koyanagi, Stubbs and Oh24), and mental health complications are associated with fast-food consumption(Reference Mohr, Wilson and Dunn30). For example, previous studies have shown that food insecurity may lead to higher levels of stress(Reference Yau and Potenza14), and it is possible that increasing cravings for high-energy foods may be induced as a coping strategy for this stress(Reference Yau and Potenza14). Finally, literature suggests that those who are from a lower socio-economic status (and thus more likely to be food insecure) live in closer proximity to fast-food outlets. Thus, it is possible that food-insecure people are more likely to consume fast food owing to convenience and greater availability(Reference Thornton, Lamb and Ball31).
It is important to note that although the pooled estimate showed a significant association between food insecurity and fast-food consumption in the overall sample and in LMIC, such an association was not observed for HIC although a moderate level of between-country heterogeneity was observed within HIC. The findings from HIC are not in line with previous studies from this setting (i.e. USA and Australia)(Reference Widome, Neumark-Sztainer and Hannan15,Reference Burns, Bentley and Thornton16) , but it is important to note that the HIC included in our study were not Western countries with a large variation in terms of geographical location. Moreover, there are some important differences between our study and those previous studies that may explain the discrepant findings. For example, the previous study in the USA used data now over two decades old(Reference Widome, Neumark-Sztainer and Hannan15), and the previous study carried out in Australia collected data from the main food shopper in each household and thus did not focus on adolescents per se (Reference Burns, Bentley and Thornton16). At least in our study, the observed differences between country-income levels may be related to national actions to combat food insecurity. For example, in some HIC, food banks are readily available(Reference Loopstra, Lambie-Mumford and Fledderjohann32) and have been found to reduce levels of food insecurity(Reference Bazerghi, McKay and Dunn33). Moreover, in many HIC, children and young people are provided with free and healthy school meals(Reference Kitchen, Tanner and Brown34,35) . However, both of these kinds of initiatives are rare in LMIC. Finally, although speculative, it is possible that food-insecure adolescents and their parents in some countries included in our study may be more aware of the deleterious health effects of fast food or that fast food is not readily available or affordable in some settings, and this might explain some of the between-country heterogeneity observed. However, clearly, further studies are necessary to understand the reason for the moderate level of between-country heterogeneity observed in our study.
The large multi-country sample of children and adolescents is a clear strength of the present study. However, findings must be interpreted in light of its limitations. First, the study was cross-sectional in nature, and thus the direction of the association is not known. However, it is highly unlikely that fast-food consumption per se leads to food insecurity. Moreover, the mere co-occurrence of these two conditions is of importance as they are both associated with adverse physical and mental health outcomes. Second, the study relied on self-reported data which could have been affected by factors such as recall and social desirability biases. Third, our measure on food insecurity (hunger) was based on a single question based on hunger due to lack of food at home, which can be considered a rare and extreme manifestation of food insecurity, and we were thus unable to assess all aspects of food shortage and inadequacy. Moreover, our measure of fast food did not ask about the type of fast food being consumed. Indeed, certain types of fast food may be more detrimental to both physical and mental health than others. Future research should aim to investigate the present association using fast-food type as an outcome. It should also be noted that the validity of our question on fast-food consumption has not been examined and thus is unknown. Fourth, there is much overlap between poverty and food insecurity. Thus, it is possible that the association observed in our study may also partly be explained by other aspects of poverty that could not be adjusted for in our analysis due to lack of data. Fifth, information on factors such as parent’s SES, family structure and other environmental factors (e.g. availability of fast food in the neighbourhood) were not available in the data set. Thus, the influence of these factors in the association between food insecurity and fast-food consumption could not be assessed. Sixth, the countries included in our study are not representative of all countries that belong to the country-income level. For example, the high-income countries included in our study were all from non-Western settings. Sixth, some students aged 15 years in our study may have major national examinations where they will likely have extended study hours. This may influence students to consume snacks/foods that are high in energy and affordable. However, the present study did not collect data on this and was thus unable to account for its potential influence. Finally, our study only focused on one aspect of dietary intake and behaviour. Thus, future studies should examine the association between food insecurity and other aspects of dietary behaviour such as intakes of nutrients (e.g. Na, saturated fats, added sugar), breakfast skipping and overall dietary quality.
In conclusion, in the present large sample of children and adolescents from sixty-eight countries representing all economic settings, food insecurity was associated with fast-food consumption in LMIC but not in HIC, although a moderate level of between-country heterogeneity was present. The mere co-occurrence of food insecurity and fast-food consumption is of public health importance and to tackle this issue requires a strong governmental and societal approach potentially utilising effective methods as demonstrated in some HIC such as the implementation of food banks and the adoption of free school meals. However, whether such methods would be feasible and effective in LMIC is not known, and future research is thus required to identify the efficacy of implementing such approaches in low economic settings. Finally, interventions to increase knowledge on the deleterious health effects of fast food may be important especially for food-insecure households.
Acknowledgements
This paper uses data from the Global School-Based Student Health Survey (GSHS). GSHS is supported by the WHO and the US Centers for Disease Control and Prevention.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
All authors listed have made a substantial, direct and intellectual contribution to the work and approved it for publication.
There are no conflicts of interest.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114521001173






