Nutrient intake assessment is essential for planning dietary interventions at an individual level and is a major component of public health and nutrition policy. However, epidemiological research related to dietary surveys or nutrient intake adequacy has largely been focused on the overconsumption of certain nutrients, especially fat, SFA, trans-fatty acids, sugars, Na or cholesterol, according to nutrition goals and obesity or prevalent diet-related diseases( 1 , Reference Freeland-Graves and Nitzke 2 ).
Micronutrient deficiencies constitute a health challenge in the WHO Regional Office for Europe( 3 ). In fact, epidemiological research confirms that the prevalence of suboptimal micronutrient intakes across Europe is an emerging concern in terms of public health( Reference Roman Viñas, Ribas Barba and Ngo 4 ), but the different methods applied have led to different estimates of the prevalence of micronutrient intake inadequacy( Reference Tabacchi, Wijnhoven and Branca 5 ).
Dietary patterns( Reference Estruch, Ros and Salas-Salvadó 6 ) and specific micronutrients have an important role in the development of chronic and degenerative diseases( Reference Zheng, Boyle and Willett 7 – Reference Rees, Dyakova and Ward 11 ). Dietary variety and dietary indices have shown fair-to-moderate validity for measuring micronutrient intake adequacy( Reference Foote, Murphy and Wilkens 12 – Reference Moore, Singer and Qureshi 14 ). As adherence to the Mediterranean diet (MeDiet) increases, the probability of not fulfilling micronutrient recommendations sharply decreases( Reference Serra-Majem, Bes-Rastrollo and Román-Viñas 15 , Reference Maillot, Issa and Vieux 16 ).
In relation to the role of macronutrients in micronutrient intake adequacy, certain levels of fat and carbohydrate (CHO) intakes (28–30 % and 50–54 % of total energy, respectively) have been proposed as the ‘optimal’ intake levels for pregnant women( Reference Blumfield, Hure and MacDonald-Wicks 17 ) .
Previous investigations have reviewed the associations between CHO quantity and micronutrient intake adequacy, but the evidence on CHO quality is sparse( Reference Gibson 18 – Reference Louie, Markovic and Ross 21 ). As recognised for fat( Reference Hooper, Summerbell and Thompson 22 ), CHO are also a heterogeneous class of nutrients, and refining recommendations for improving the quality of CHO intake from a public health perspective has been suggested( Reference Roberts and Liu 23 ).
However, to our knowledge, there are no studies that have examined, at the same time, the relationship between the overall dietary quality of CHO or other indices of macronutrient quality and nutritional adequacy. We tested the following hypothesis: higher CHO quality is associated with higher micronutrient intake adequacy. Thus, the aims of the present study were to define a framework for assessing the quality of CHO intake and to investigate the association between the CHO quality index (CQI) and the intake adequacy of nineteen micronutrients in the Seguimiento Universidad de Navarra (SUN) cohort study. Additionally, the association between the fat quality index (FQI) and the MeDiet pattern and nutritional adequacy was assessed.
Subjects and methods
Study population
The SUN Project is a multipurpose and dynamic cohort project designed to study the prospective association between diet and the occurrence of major chronic diseases( Reference Martinez-Gonzalez, Sanchez-Villegas and De Irala 24 ). The details of cohort design, recruitment strategy and follow-up methods are available elsewhere( Reference Segui-Gomez, de la Fuente and Vazquez 25 ). Briefly, the recruitment of participants started in December 1999, and it is permanently open. All the participants are Spanish university graduates, with a high educational level. Information is collected using self-administered questionnaires sent by post or electronic mail every 2 years. The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all the procedures involving human subjects were approved by the Institutional Review Board of the University of Navarra. Voluntary completion of the baseline questionnaire was considered as informed verbal consent. Participants with data obtained through FFQ at baseline or who answered the baseline questionnaire before March 2012 were eligible for the present study (n 21 478). Among them, we excluded subjects who had intake levels outside the predefined limits of total energy intake: < 3349 kJ/d (800 kcal/d) for men and < 2093 kJ/d (500 kcal/d) for women; >16 747 kJ/d (4000 kcal/d) for men and >14 654 kJ/d (3500 kcal/d) for women (n 2034), and subjects whose intake levels were outside the predefined intake values of any micronutrient (at three or more standard deviations from both sides of the mean) (n 2583). Participants who reported implausibly high or low energy intake levels were not included in the study because these levels are unlikely to be true( Reference Willett and Willet 26 ). Subjects reporting extreme values of micronutrient intakes were also not included to avoid underestimation or overestimation of the prevalence of inadequacy. Therefore, the final sample comprised 16 841 participants.
The estimated sample size for a two-sample comparison of proportions (highest v. lowest quintile of CQI) was based on the following assumptions: α = 0·05 (two-sided) and statistical power = 90 %; a proportion of participants with an inadequacy value of 0·15 in the highest inadequacy category and a proportion with an inadequacy value of 0·1 in the best adequacy quintile. Under these assumptions, the sample size needed was 918 participants in each quintile.
Exposure assessment
Dietary intake was assessed using a baseline semi-quantitative FFQ repeatedly validated in Spain( Reference Martin-Moreno, Boyle and Gorgojo 27 , Reference De la Fuente-Arrillaga, Ruiz and Bes-Rastrollo 28 ). It exhibited reasonably good validity for assessing fat intake and also CHO intake( Reference Fernández-Ballart, Piñol and Zazpe 29 ). Nutrient intakes of 136 food items were calculated as frequency multiplied by the nutrient composition of the specified portion size for each food item, using an ad hoc computer program developed for this purpose. There were nine options for the average frequency of consumption (from never/almost never to at least six times per d). Trained dietitians updated the nutrient data bank using the available information from the food composition tables for Spain( Reference Mataix Verdú 30 , Reference Moreiras, Carbajal and Cabrera 31 ). Furthermore, the average intake of micronutrients from dietary supplements was added to the intake from foods, taking into account the consumption frequency over the past year.
We used baseline dietary intake data to construct a new index. The CQI was defined summing the following four criteria: dietary fibre intake (g/d); glycaemic index; whole grains:total grains ratio; solid CHO:total CHO ratio (Table 1). For the last criterion, we considered only the amount of CHO from each food. The intake of total grains was calculated by summing the intakes of whole grains, refined grains and their products. For each of these four components, participants were categorised into quintiles and were given a value (ranging from 1 to 5) according to each quintile. Finally, by summing all the values, we constructed the CQI (ranging from 4 to 20), and it was also categorised roughly into quintiles.
Table 1 Criteria used to calculate carbohydrate quality and fat quality
* Proportional dietary indices were computed for intakes ranging between the maximum and minimum criteria.
On the other hand, we used two indices to compare the results in relation to the CQI and micronutrient intake adequacy: the FQI and a priori MeDiet score. To calculate the FQI, we used the ratio MUFA+PUFA:SFA+trans-fatty acids (Table 1). According to this score (ranging from 0·62 to 5·92), the participants were categorised into quintiles. Finally, we used an a priori score to appraise adherence to the MeDiet as proposed by Trichopoulou et al. ( Reference Trichopoulou, Costacou and Bamia 32 ) to assess the association between the adherence to this dietary pattern and nutritional adequacy. With the exception of alcohol, sample sex-specific median cut-off points for eight items were used. For beneficial components (fruits and nuts, cereal, fish, vegetables and legumes), subjects whose consumption was below the median were assigned a value of 0 and subjects whose consumption was at or above the median were assigned a value of 1. For components presumed to be detrimental (meat, poultry and dairy products), subjects whose consumption was below the median were assigned a value of 1 and subjects whose consumption was at or above the median were assigned a value of 0. Finally, for ethanol, a value of 1 was assigned to men who consumed between 10 and 50 g/d and to women who consumed between 5 and 25 g/d.
We also used the MeDiet score to assess the association between the adherence to this dietary pattern and nutritional adequacy. The range was from 0 points for minimum adherence to 9 points for maximum adherence. Finally, we categorised all the participants into quintiles according to the MeDiet score.
Outcome assessment
We aimed to determine micronutrient intake adequacy for the following nineteen micronutrients with known public health relevance: Zn; I; Se; Fe; Ca; K; P; Mg; Cr; vitamin B1; vitamin B2; vitamin B3; vitamin B6; vitamin B12; vitamin C; vitamin A; vitamin D; vitamin E; folic acid. The probability of intake adequacy was calculated by comparing the intakes of these nutrients with the estimated average requirements (EAR) when these were available or adequate intake levels, if not, as proposed by the Institute of Medicine( 33 ).
On the other hand, intake adequacy for sixteen nutrients (all, but Cr, K and Fe) was also evaluated using the probabilistic approach( Reference Anderson, Peterson and Beaton 34 ). With this approach, the probability of adequacy for the usual intake of a nutrient was calculated from a z-score, as follows: z-score = (estimated nutrient intake − EAR)/sd of the EAR. Besides, when we calculated the probability of adequacy for the intake of Fe, the distribution intake was log transformed.
Assessment of other variables
During the baseline assessment, information was also gathered on sociodemographic and anthropometric variables, lifestyle and health-related habits and medical history. Self-reported BMI was calculated as weight (in kg)/the square of height (in m). Self-reported anthropometrics had been validated previously in a subsample of the cohort( Reference Basterra-Gortari, Bes-Rastrollo and Forga 35 ). Information regarding physical activity during leisure time was gathered at baseline with a specific questionnaire previously validated in Spain( Reference Martinez-Gonzalez, Lopez-Fontana and Varo 36 ). We obtained a value of overall weekly MET (metabolic equivalents)-h/week for each participant by taking into account the time spent on each activity weekly.
Statistical analyses
We compared the baseline characteristics of the participants according to five categories of dietary quality scores. We calculated means and standard deviations or percentages for each variable across the five categories. χ2 Tests or ANOVA were used to assess the statistical significance of the differences among proportions or means, respectively. Pearson's correlation coefficients were calculated to identify the relationship between three dietary quality scores and between each dietary index and its components.
We used non-conditional logistic regression models to assess the relationship between the CQI, FQI or MeDiet score and the risk of inadequate nutrient intakes using the EAR cut-point approach and the probabilistic approach. In all the analyses, the lowest quintile was used as the reference category. Crude OR and multivariate-adjusted OR were estimated in the following analyses: (1) failing to comply with four or more recommendations and (2) with eight or more unmet recommendations. For each dietary quality score, we fitted three multivariable-adjusted models controlling for the following potential confounders or sources of bias: (1) age (continuous); sex and educational level (four categories); (2) additionally adjustment for total energy intake and total CHO or fat intake (continuous); (3) additionally adjusted for the MeDiet score (continuous)( Reference Moreiras, Carbajal and Cabrera 31 ), BMI (continuous), physical activity (continuous), smoking status (three categories) and dietary supplement use (yes/no). Tests of linear trend across successive quintiles of the three dietary quality scores were conducted assigning the median value to each quintile category and treating the variables as continuous.
The analyses were carried out using STATA version 12 (STATA Corporation). All P values were two tailed, and statistical significance was set at the conventional cut-off of P< 0·05.
Results
The baseline characteristics of the study participants according to the extreme quintiles of CQI and FQI are summarised in Table 2 and Supplementary Table S1 (available online), respectively. Subjects with a higher CQI (fifth quintile, Q5) were more likely to be women, to be physically active and to have a history of hypertension or diabetes (Table 2). The CQI was also found to be directly associated with higher adherence to a MeDiet pattern and consumption of fruits, vegetables, legumes, fish, olive oil and nuts. However, the differences in macronutrient intakes were minimum for all of them. Besides, all the values for micronutrient intakes increased with the increasing quintiles of CQI (P< 0·001).
Table 2 Baseline main characteristics of the 16 841 participants of the Seguimiento Universidad de Navarra (SUN) Project according to carbohydrate quality (Mean values and standard deviations; number of participants and percentages)
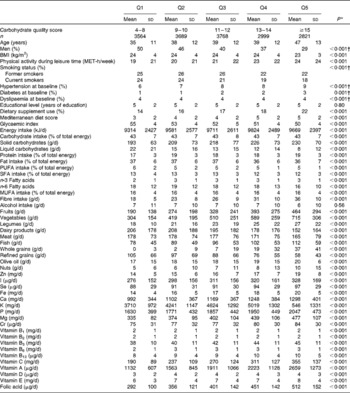
Q, quintiles; MET, metabolic equivalents.
* P values reported are those obtained in ANOVA adjusted for sex and age (P <0·001).
† P values reported are those obtained in the χ2 test (P <0·001).
Supplementary Table S1 (available online) demonstrates that the FQI was positively associated with being older and more active, having a history of hypertension, diabetes or dyslipaemia, adherence to the MeDiet, and CHO and fat intake, and consumption of fruits, vegetables, fish, grains, olive oil and nuts. For all the micronutrients under study, except for I, Ca, P and vitamin B3, a higher dietary intake was observed among subjects with a higher FQI.
The prevalence of inadequate intake below the EAR for each nutrient according to each score is summarised in Supplementary Table S2, available online. Subjects in the highest quintile of CQI or MeDiet score had the lowest prevalence of inadequate dietary intake for every vitamin and mineral. Contrarily, the number of participants with non-compliance to the EAR for I, Ca, P and vitamins B2, B3 and B12 was highest in the fifth quintile of FQI. The mean prevalence of inadequacy was between 19 and 58 % for Ca, P, Mg and folic acid and above 93 % for vitamins D and E.
Tables 3 and 4 present the risk of not meeting ≥ 4 or ≥ 8 dietary recommended intakes (DRI) according to the quintiles of CQI or FQI using the probabilistic approach. Participants in the quintile of poorest quality of CQI had a 17·5-fold risk of failing to meet ≥ 8 DRI (Table 3). A higher CQI showed a strong inverse association with the risk of not meeting the DRI levels. In the adjusted model, the OR for successive quintiles of CQI were 1·00 (reference), 0·49 (95 % CI 0·33–0·73), 0·31 (95 % CI 0·19–0·48), 0·15 (95 % CI 0·08–0·29) and 0·06 (95 % CI 0·02–0·16) for failing to meet ≥ 8 DRI after adjusting for the main potential confounders (P for trend < 0·001). When we repeated the analyses for failing to meet ≥ 4 DRI, the results were basically the same.
Table 3 Risk of failing to meet ≥4 and ≥8 dietary reference intakes (DRI) according to the quintiles (Q) of carbohydrate quality in 16 841 participants of the Seguimiento Universidad de Navarra (SUN) Project using the probabilistic approach (Odds ratios and 95 % confidence intervals)
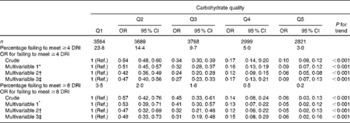
Ref., reference.
* Multivariable 1: adjusted for age, sex and educational level.
† Multivariable 2: additionally adjusted for total energy intake and total carbohydrate intake.
‡ Multivariable 3: additionally adjusted for the Mediterranean diet score, BMI, physical activity during leisure time (metabolic equivalents-h/week), smoking status and dietary supplement use.
Table 4 Risk of failing to meet ≥4 and ≥8 dietary reference intakes (DRI) according to the quintiles (Q) of fat quality in 16 841 participants of the Seguimiento Universidad de Navarra (SUN) Project using the probabilistic approach (Odds ratios and 95 % confidence intervals)
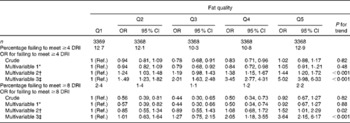
Ref., reference.
* Multivariable 1: adjusted for age, sex and educational level.
† Multivariable 2: additionally adjusted for total energy intake and total fat intake.
‡ Multivariable 3: additionally adjusted for the Mediterranean diet score, BMI, physical activity during leisure time (metabolic equivalents-h/week), smoking status and dietary supplement use.
When we assessed the association between the FQI and not achieving ≥ 4 or ≥ 8 DRI, we found a direct association after both the models had been adjusted for age, sex, educational level, energy intake, total fat intake and MeDiet score, BMI, physical activity, smoking status and dietary supplement use (Table 4). Thus, the OR for the fifth quintile for failing to meet ≥ 8 was 3·64 (95 % CI 2·15, 6·17 and P for trend < 0·001).
We repeated the analyses using deciles to calculate the CQI and the a priori MeDiet score (Figs. 1 and 2, respectively), and they supported the robustness of our findings.
Fig. 1 Risk of failing to meet ≥ 4 dietary recommended intakes according to the deciles of carbohydrate quality in 16 841 participants of the Seguimiento Universidad de Navarra (SUN) Project using the probabilistic approach. Values are odds ratios, with 95 % confidence intervals represented by vertical bars. P for trend < 0·001. (A colour version of this figure can be found online at http://www.journals.cambridge.org/bjn).
Fig. 2 Risk of failing to meet ≥ 4 dietary recommended intakes according to deciles of Mediterranean diet score in 16 841 participants of the Seguimiento Universidad de Navarra (SUN) Project using the probabilistic approach. Values are odds ratios, with 95 % confidence intervals represented by vertical bars. P for trend < 0·001. (A colour version of this figure can be found online at http://www.journals.cambridge.org/bjn).
The OR and 95 % CI for unmet EAR for eight or more nutrients across the quintiles of CQI are shown in Supplementary Fig. S1 (available online). A lower risk of inadequate intake was observed among participants in the highest quintile of CQI after adjusting for several potential confounders (OR 0·10, 95 % CI 0·06, 0·19). On the other hand, a higher FQI was found to be significantly associated with a higher risk of not achieving the EAR for nine or more micronutrients in comparison with the lowest category of FQI (OR 3·26, 95 % CI 2·22, 4·77) (Supplementary Fig. S2, available online). On the contrary, a higher MeDiet score was found to be associated with a higher likelihood of meeting the EAR for nine or more micronutrients (Supplementary Fig. S3, available online). In the three analyses, the P value for trend was significant (P< 0·001).
The number of nutrients with intakes not meeting the EAR was lower in the extreme quintile of CQI or MeDiet score and higher in the fifth quintile of FQI (Figs. 3 and 4 and Supplementary Fig. S4, available online, respectively).
Fig. 3 Average number of nutrients with intakes not meeting the estimated average requirement across the quintiles (Q) of carbohydrate quality index. (A colour version of this figure can be found online at http://www.journals.cambridge.org/bjn).
Fig. 4 Average number of nutrients with intakes not meeting the estimated average requirement across the quintiles (Q) of Mediterranean diet score. (A colour version of this figure can be found online at http://www.journals.cambridge.org/bjn).
Fig. 5 shows relative risks for nutrients not meeting the EAR according to the joint classification by CQI and FQI. A higher quality of CHO intake was found to be associated with a lower risk of unmet requirements for nine or more micronutrients in comparison with the lowest category of FQI in the three intake groups of FQI.
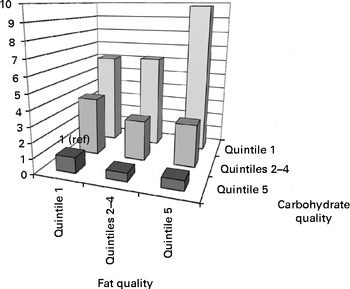
Fig. 5 OR and 95 % CI for unmet estimated average requirement for at least 50 % of nutrients according to the quintiles of carbohydrate quality and fat quality in 16 841 participants of the Seguimiento Universidad de Navarra (SUN) Project. OR were adjusted for age, sex, educational level, total energy intake, BMI, physical activity during leisure time (metabolic equivalents-h/week), smoking status and dietary supplement use.
Correlation coefficients between the glycaemic index, fibre intake, whole grains:total grains ratio and solid CHO:total CHO ratio were − 0·34,+0·58,+0·63 and +0·33. Correlation coefficients between MUFA, PUFA, SFA and trans-fatty acids and FQI were +0·19,+0·29, − 0·35 and − 0·42. Finally, correlation coefficients between the dietary quality scores were as follows: 0·12 between the CQI and FQI; 0·36 between the CQI and MeDiet score; 0·48 between the MeDiet score and FQI.
Discussion
To the best of our knowledge, the present study is the first to investigate the association between two new scores of CHO or fat quality and the adequacy of micronutrient intake. The members of the young Mediterranean cohort examined in the present study who had a high CQI or adhered to a MeDiet were found to be at a lower risk of having micronutrient intake inadequacy. These findings could contribute to the development of prevention and nutritional education strategies focused not only on the levels of macronutrient intake( Reference Pennington, Kandiah and Nicklas 37 , Reference Nicklas 38 ), but also on the quality of macronutrients, particularly CHO. Moreover, in this context, this seems to be more important than the quality of fat.
Previous studies( Reference Foote, Murphy and Wilkens 12 – Reference Moore, Singer and Qureshi 14 ) have focused on assessing how diet quality, dietary patterns and food variety are validated measures to determine micronutrient intake adequacy. In the SUN cohort, it has been confirmed earlier that higher adherence to a MeDiet pattern is associated with a lower prevalence of inadequacy for the intake of Zn, I, Mg, Fe, Se and vitamins E, B1, A, C and folic acid( Reference Serra-Majem, Bes-Rastrollo and Román-Viñas 15 ). In the present study, we also found that a better profile of micronutrient intake is associated with adherence to the MeDiet measured by using an a priori MeDiet score. In fact, we found that the global prevalence of nutrient intake inadequacy is higher for Ca, K, Mg and vitamins D and E and lower for P and vitamin B3. In general, these results are consistent with the evidence obtained from Spain( Reference del Pozo, Cuadrado and Moreiras 39 – Reference Molina-Montes, Sanchez-Cantalejo and Martinez 42 ) and Europe( Reference Roman Viñas, Ribas Barba and Ngo 4 , Reference Mensink, Fletcher and Gurinovic 43 , Reference Kleiman, Ng and Popkin 44 ).
As expected, participants with better CHO intake quality reported higher consumption of fruits, vegetables, legumes and nuts and lower consumption of grains. Furthermore, those in the higher quintile of CQI were more likely to meet micronutrient recommendations. In absolute terms, the intake of CHO (percentage of total energy) was quite similar across the quintiles of CQI, ranging from 42·7 to 43·4 %, suggesting that it is not the quantity of CHO but quality that is really important when assessing micronutrient intake adequacy. In fact, the quantities of protein and fat were very similar across all the groups. A possible explanation for this result is that whole grains and low-glycaemic index foods are particularly rich in micronutrients, while major sources of liquid CHO, particularly sugar-sweetened beverages, are mostly less nutritious foods. These drinks have been linked to obesity and other cardiometabolic problems, and recently, global legislative initiatives and prizing instruments have been recommended as public policies to change consumption patterns( Reference Araujo, Bezerra and Barbosa Fdos 45 , Reference Powell, Chriqui and Khan 46 ).
Systematic reviews offer no conclusive evidence for the relationship between added sugar and micronutrient intakes( Reference Rennie and Livingstone 19 ) and do not allow establishing an optimal level of added sugar intake for micronutrient intake adequacy( Reference Gibson 18 , Reference Ruxton, Gardner and McNulty 47 ). With respect to dietary glycaemic load, two interesting works have recently demonstrated that a higher-glycaemic index diet predicts a greater risk of not meeting the recommendations for several micronutrients in pregnant women( Reference Louie, Markovic and Ross 21 ), children and adolescents( Reference Louie, Buyken and Brand-Miller 20 ).
There is very limited evidence for the association between fat quality and DRI compliance, although low-fat diets could increase the risk of inadequate intakes of essential fatty acids and fat-soluble vitamins( Reference Aranceta and Perez-Rodrigo 48 ). Several mechanisms might be proposed to explain the strong and positive association between fat quality and nutritional inadequacy. Protein intake was found to be significantly low among participants with better fat quality in comparison with those with worse quality, probably because the consumption of dairy products and meat was also significantly low. In fact, when we additionally adjusted for protein intake (percentage of total energy), no association was found between the FQI and nutritional adequacy (OR for the fifth quintile: 0·95, 95 % CI 0·52, 1·76; P for trend = 0·883). This outcome is in agreement with the findings of other investigations in adolescents, which demonstrated the importance of consuming meat and dairy products to meet a broad range of micronutrient recommendations( Reference Moore, Singer and Qureshi 14 ).
On the other hand, we found higher adherence to a MeDiet pattern to be associated with a higher likelihood of meeting the dietary recommendations for micronutrients and with a lower number of nutrients with dietary intake levels unmet. The main explanation for these findings might be that the traditional MeDiet, rich in minerals, vitamins, antioxidants, fibre (from vegetable food), n-3 fatty acids (from fish and sea food) and unsaturated fatty acids (from olive oil and nuts), has an appropriate balance of both macronutrients and essential micronutrients, while having relatively low levels of energy-dense or nutrient-poor foods, such as processed meat, processed meals and fast food( Reference Martínez-González, de la Fuente-Arrillaga and Nunez-Cordoba 49 ).
We acknowledge that the present study has some limitations. First, we used a self-reported FFQ, which has measurement errors and might not be the best method to assess the intake of some micronutrients (e.g. Se, Fe and folic acid). For example, the Se contents of foods vary according to soil contents, so FFQ assessments of Se intake typically have a fair degree of measurement errors( Reference Serra-Majem, Pfrimer and Doreste-Alonso 50 ). However, FFQ is the most practical and feasible tool to evaluate food habits in large epidemiological studies. Besides, the present study sample comprised highly educated volunteers, so the data are of fairly adequate quality. Second, to translate food consumption into micronutrient intakes, we used two well-known Spanish food composition tables, which might be a source of variation in our findings. Third, as in any observational study, some residual confounding might not have been totally excluded. However, we carried out the analyses adjusting for the main known confounders of nutritional adequacy, and for this reason, we do not consider residual confounding as a likely important cause of the observed findings. Fourth, the total dietary intake of micronutrients could have been probably underestimated, as we did not calculate the average intake of vitamins and minerals from all sources of the nutrients. Thus, to assess the risk of inadequate intake, we included the intake from foods and from dietary supplements in the data analysis, without considering the intake from fortified foods or medication that participants might be consuming. Fifth, the present results demonstrate the probability of adequacy, but do not indicate nutrient deficiencies or whether the diet of this population is adequate. In fact, real nutritional deficiency should be confirmed by biomarkers of nutrient intake. Lastly, a potential weakness of using the SUN cohort was that all the participants were university graduates and, therefore, cannot be considered in any way as representative of the general population. The participants of the present study were more likely to be homogeneous in terms of their background diet than participants would be if a similar study were conducted in a representative sample of the general population. Homogeneity among the participants of the SUN study regarding their background diet can limit the generalisability of our findings and may also have reduced the between-subject variability in dietary exposures, because they belong to a single educational and socio-economic stratum. On the other hand, this fact can also be viewed as an advantage because this homogeneity regarding the background diet of the study participants could also have actually enhanced the validity of the study, because this homogeneity reduced the potential confounding related to socio-economic status, educational level and background diet variability. In any case, we adjusted the present results for total energy intake and other confounders related to this background diet. In addition, analyses assessing the CQI and FQI were also adjusted for the overall dietary pattern (MeDiet) and CHO or fat intake levels, respectively.
The strengths of the present study are that we used data obtained from a well-known Mediterranean cohort (the SUN study cohort) with a relatively large sample size and a high response rate. In addition, we were able to adjust for numerous potential confounders. Moreover, dietary intake was measured using a previously validated FFQ in a highly educated cohort with self-reported data of high quality( Reference Martin-Moreno, Boyle and Gorgojo 27 , Reference De la Fuente-Arrillaga, Ruiz and Bes-Rastrollo 28 ). Results obtained using two different methods to estimate nutrient intake adequacy were very similar: the probabilistic approach and the EAR cut-point approach. The use of the latter approach as a reference for estimating nutritional adequacy compared with the DRI value will not lead to an overestimation of the prevalence of dietary inadequacy. Finally, to our knowledge, the two new dietary quality scores used in the present study, the CQI and FQI, have not been used before, including several of the proposed recommendations, to assess nutrient intake adequacy( Reference García-Alvarez, Blanquer and Ribas-Barba 51 ).
In conclusion, a higher CQI was found to be strongly associated with better micronutrient intake adequacy in the young Mediterranean cohort examined in the present study. The findings suggest the usefulness of measuring CHO quality taking into account fibre and proportion of whole grains and liquid CHO. Furthermore, the present results could be translated to a universal dietary advice: increasing the consumption of whole grains and fibre and decreasing that of dietary added sugars and liquid CHO will not only reduce the negative effects of liquid CHO on health, but also improve micronutrient intake adequacy.
Supplementary material
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/S0007114513004364
Acknowledgements
The authors thank the SUN cohort members for their enthusiastic collaboration and participation. They also thank the other members of the SUN study group: A. Alonso; S. Benito; J. J. Beunza; J. de Irala; M. Delgado-Rodriguez; A. Gea; F. Guillén-Grima; J. Llorca; C. Lopez del Burgo; A. Marti; J. M. Nuñez-Cordoba; A. Pimenta; M. Ruiz-Canela; D. Sanchez; A. Sanchez-Villegas; M. Serrano-Martinez; E. Toledo; Z. Vazquez. They are also grateful to the members of the Department of Nutrition of Harvard School of Public Health (A. Ascherio, W. Willett, and F. B. Hu) for helping design the SUN study.
The SUN study received funding from the Instituto de Salud Carlos III, Official Agency of the Spanish Government for biomedical research (grants PI01/0619, PI030678, PI040233, PI042241, PI050976, PI070240, PI070312, PI081943, PI080819, PI1002293, PI1002658, RD06/0045 and G03/140), the Ministerio de Sanidad, Política Social e Igualdad through the Plan Nacional de Drogas (2010/087), the Navarra Regional Government (36/2001, 43/2002, 41/2005, 36/2008, 45/2011) and the University of Navarra. E. Toledo is supported by a Rio Hortega post-residency fellowship of ISCIII, Ministry of Economy and Competitiveness, Spanish Government.
The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review and approval of the manuscript.
The authors' contributions are as follows: I. Z., S. S., J. A. M. and M. A. M.-G. designed the research; I. Z., A. S.-T., S. S. and M. A. M.-G. conducted the research; C. d. l. F.-A., M. B.-R. and M. A. M.-G. provided essential materials; I. Z., A. S.-T., S. S. and M. A. M.-G. analysed the data and carried out the statistical analyses; I. Z. and S. S. had primary responsibility for the final content. All authors read and approved the final manuscript.
The authors declare that there are no conflicts of interest.











