‘Mental health first aid’ has been defined as ‘the help provided to a person developing a mental health problem or in a mental health crisis. The first aid is given until appropriate professional help is received or until the crisis resolves’.Reference Langlands, Jorm, Kelly and Kitchener1 More recently, the definition has been broadened to also include the help offered to a person ‘experiencing the worsening of a mental health problem’.Reference Kitchener, Jorm and Kelly2 This concept distinguishes the initial assistance given by a layperson from ongoing carer roles and from professional help.
There is evidence to support the importance of this type of initial assistance. When a person develops a mental health problem, they will frequently turn to others in their social network for help.Reference Jorm, Medway, Christensen, Korten, Jacomb and Rodgers3 Indeed, seeking help from family and friends is often one of the first actions taken to deal with mental health problems, and this frequently occurs before seeking help from a health professional.Reference Jorm, Griffiths, Christensen, Parslow and Rogers4 However, although many people with mental health problems receive positive support from their social network,Reference Reavley and Jorm5 avoidance and discrimination are also common, particularly for people with more severe mental disorders.Reference Reavley, Morgan and Jorm6–Reference Thornicroft, Brohan, Rose, Sartorius and Leese8
The reactions from a person's social network can affect the outcome of their mental health problem. A person is more likely to seek professional help for a mental health problem if someone else suggests that they do this,Reference Cusack, Deane, Wilson and Ciarrochi9, Reference Vogel, Wade, Wester, Larson and Hackler10 and faster treatment is associated with a better outcome.Reference Ghio, Gotelli, Marcenaro, Amore and Natta11, Reference Penttila, Jaaskelainen, Hirvonen, Isohanni and Miettunen12 It is also known that good social support from family can aid recovery,Reference Keitner, Ryan, Miller, Kohn, Bishop and Epstein13 whereas negative interactions can impede it.Reference Hooley14 Positive social support also helps to reduce the impact of traumatic life events.Reference Charuvastra and Cloitre15
Mental health first aid training
Given the potential importance of the public providing mental health first aid, there is a need to improve public knowledge and skills in this area. For this reason, a Mental Health First Aid (MHFA) training course for the public was developed in Australia in 2000 and has been disseminated to many other countries.Reference Jorm and Kitchener16 This course is an adaptation of the first aid training model used for physical health emergencies and it covers developing mental health problems (e.g. depression, psychosis, substance use problems) and mental health crises (e.g. suicidal, self-injuring, exposed to a traumatic event). MHFA training was initially developed to train adults to assist other adults,Reference Kitchener and Jorm17 but has since been extended to adults to assist youth,Reference Kelly, Mithen, Fischer, Kitchener, Jorm and Lowe18 to adolescents to assist their peersReference Hart, Mason, Kelly, Cvetkovski and Jorm19 and to adults to assist older persons.Reference Kitchener, Jorm and Kelly20 There have also been a number of adaptations of the training to cover cultural subgroups.Reference Kanowski, Jorm and Hart21, Reference Minas, Colucci and Jorm22
Early in the development of MHFA training in Australia, it became apparent that there was limited evidence available on how a member of the public should give mental health first aid. The techniques taught in conventional, physical first aid courses are based on international guidelines that have been developed using systematic reviews of the literature and expert consensus.Reference Zideman, Singletary, De Buck, Chang, Jensen and Swain23 There is thus a need to develop similar international guidelines for the provision of mental health first aid. The purpose of this review was to examine the range of guidelines that have been developed, their implementation in practice and to identify any gaps that remain to be filled.
Method
To find relevant research, we carried out a systematic search of databases and guidelines listed on the MHFA Australia website (www.mhfa.com.au), which includes grey literature. The inclusion criteria were: (a) reports on mental health first aid guidelines, with ‘mental health first aid’ defined as by Kitchener et al;Reference Kitchener, Jorm and Kelly2 (b) the primary purpose of guidelines is provision of mental health first aid; and (c) articles that detail the development of guidelines, uses/implementations of guidelines and evaluations of guidelines. Exclusion criteria were: (a) guidelines developed for health professionals (psychiatrists, psychologists, counsellors, physicians, etc.), including clinical practice guidelines; (b) guidelines aimed at carers (involving longer-term caring roles); and (c) guidelines for the provision of medical first aid. Items published in a language other than English were to be translated into English. Records were excluded if reasonable efforts to obtain full-text copies were unsuccessful.
Searches were carried out in PubMed, PsycINFO, Scopus and Web of Science on 4 April 2018. The search terms were ‘mental health first aid’ across all four databases, limiting the results from year 2000 to the present day.
Figure 1 shows the PRISMA flow diagram. A total of 55 records met eligibility criteria and were included in the review. Both authors read through records, extracting main points of information into a summary table of MHFA guidelines. Included records were classified as involving guideline development, guideline evaluation and guideline implementation.
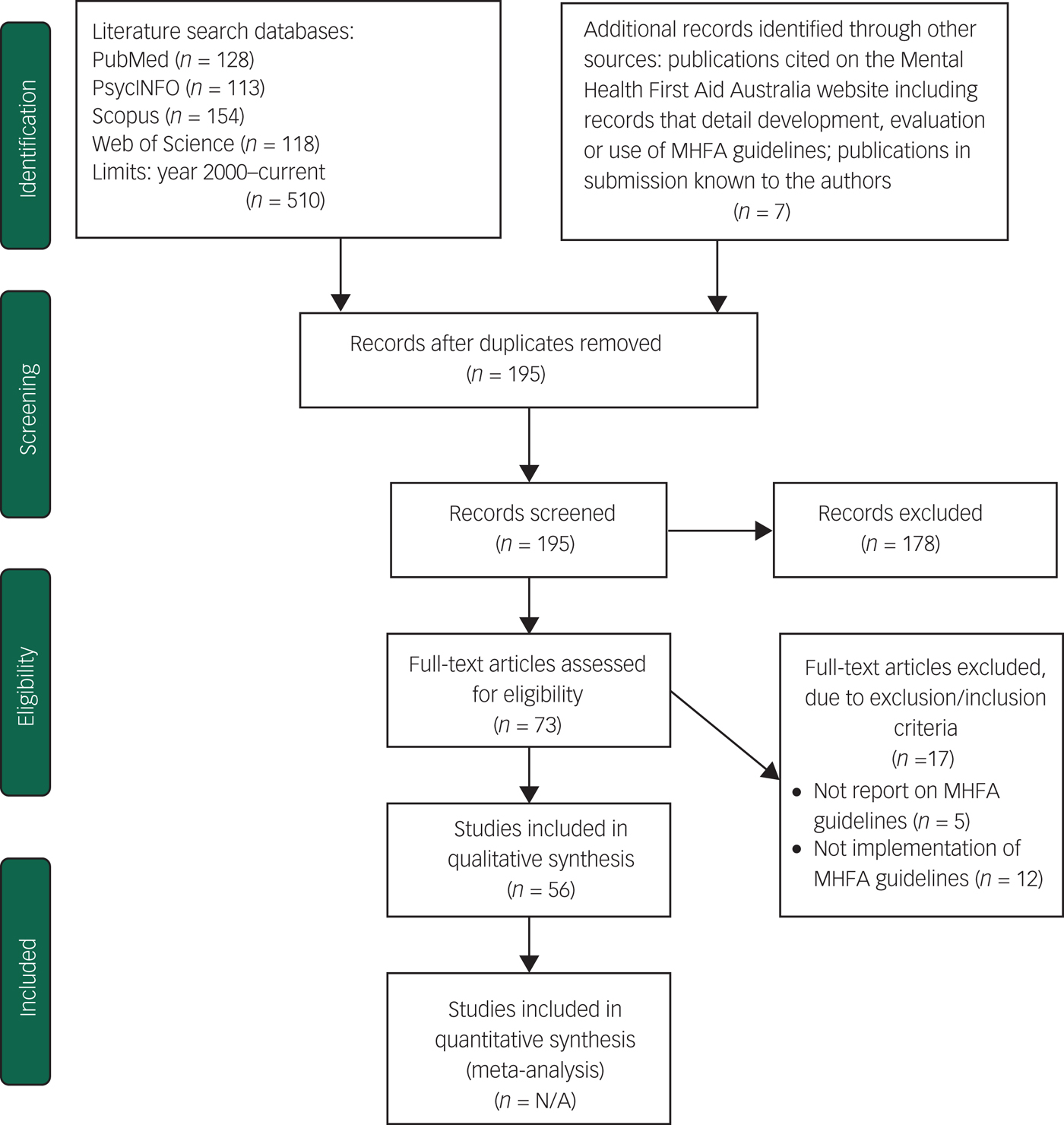
Fig. 1 PRISMA flow diagram.
Results
The 56 studies covered guidelines for assisting people with specific mental health problems in English-speaking countries (13 studies), guidelines for assisting people with mental health problems from high-risk groups and settings in English-speaking countries (six studies), guidelines for assisting Australian Aboriginal and Torres Strait Islander people (six studies), guidelines for assisting people from Asian countries (five studies), cross-cultural generalisability of guidelines (one study) and implementation of the guidelines in practice (25 studies).
Methods used for developing guidelines
Mental health first aid guidelines have been developed based on expert consensus using the Delphi method.Reference Hasson, Keeney and McKenna24–Reference Jorm26 The Delphi method is supported by research on ‘wisdom of crowds’ which shows that aggregated judgements of groups of people with imperfect expertise can lead to better decisions than individual experts.Reference Jorm26 This method involves recruiting a group of individuals with expertise on a topic, compiling a questionnaire with a list of statements that the experts rate for agreement, providing anonymous feedback to individuals on how their responses compare with the rest of the group, giving members the opportunity to revise their responses based on the feedback over a number of survey rounds and using a statistical criterion to define consensus.Reference Hasson, Keeney and McKenna24–Reference Jorm26 There are many ways in which Delphi methodology can be implemented. The application of this method for the development of mental health first aid guidelines has involved the steps described below.
Framing of research questions
The Delphi studies have been guided by a question that defines the scope of the project. The questions covered the type of person who is providing the help (e.g. adult,Reference Langlands, Jorm, Kelly and Kitchener1 adolescent,Reference Fischer, Kelly, Kitchener and Jorm27 workplace colleagueReference Bovopoulos, Jorm, Bond, LaMontagne, Reavley and Kelly28), the type of person who is being helped (e.g. Aboriginal or Torres Strait Islander person,Reference Hart, Jorm, Kanowski, Kelly and Langlands29 adolescent,Reference Ross, Hart, Jorm, Kelly and Kitchener30 LGBTIQ+ personReference Bond, Jorm, Kelly, Kitchener, Morris and Mason31) and the type of mental health issue the person has (e.g. suicidal thoughts and behaviours,Reference Ross, Kelly and Jorm32 psychosis,Reference Langlands, Jorm, Kelly and Kitchener1 panic attackReference Kelly, Jorm and Kitchener33).
Selection of expert panels
The chosen panel members have relevant expertise; this expertise may have been gained through professional experience or from lived experience as a consumer or carer. In all the projects on guidelines, a panel of mental health professionals has been used. Wherever possible, there have also been panels of consumers and carers who have taken on advocacy roles, either through membership of advocacy organisations or by creating peer support resources. The requirement for consumers and carers to also have an advocacy role was to ensure that their expertise was broader than their own individual experience. However, in some areas it was difficult to find lived-experience experts because relevant mental health advocacy organisations are rare or do not exist, for example in Asian countries and for cultural minorities such as Aboriginal Australians and refugees.
Determining expert panel size
Panels consisting of 20 or more members tend to produce stable results.Reference Jorm26 Because there are generally dropouts across rounds of a Delphi study, the aim was to have a minimum of 30 experts on a panel at the start of the study. However, experts on some topics are so scarce that this number has not been possible (e.g. mental health professionals with experience working with Iraqi refugees in AustraliaReference Uribe Guajardo, Slewa-Younan, Santalucia and Jorm34), so smaller panels have been used.
Construction of Delphi questionnaires
The Delphi questionnaires have listed potential actions that a first aider can take to assist a person with a mental health problem as well as potential knowledge they may need to guide their actions. The questionnaires were constructed in such a way as to give a comprehensive list of possibilities to the panel members to consider. For most studies on guidelines, this has been achieved by a systematic search for possible actions in websites, books and journal articles. The text from these sources was qualitatively analysed to arrive at a set of items that clearly express a single action, while trying to remain as faithful as possible to the original wording in the source. One member of the research team carried out a draft content analysis which was presented to the other researchers in the team, who then agree on the final wording of questionnaire items. Additional items have been created from gaps identified by the research team and by panel members when they were responding to the initial questionnaire. Items that have been included in the questionnaire have sometimes been contradictory because of differing opinions in the literature about appropriate first aid actions (for example, ‘the first aider should say whatever they feel they need to help the suicidal person decide against suicide, including the use of guilt and threats, e.g. telling them they will go to hell or they will ruin the lives of others if they die by suicide’ versus ‘the first aider should not use guilt or threats to prevent suicide, e.g. do not tell the person they will go to hell or ruin other people's lives if they die by suicide’).Reference Ross, Kelly and Jorm32
For some guidelines, a systematic search has been a poor source of questionnaire items because of the limited literature on the topic. This was the case for guidelines on how an adult should communicate with an adolescent about a mental health problem or other sensitive topic.Reference Fischer, Kelly, Kitchener and Jorm27 In this case, focus groups of consumers and clinicians were used to generate additional items for the questionnaire.
Administration of Delphi questionnaires
Questionnaires were administered by web survey which made it possible to have panel members from around the world. Panellists were asked to rate items according to whether they should be included in the guidelines using the following scale: ‘essential’, ‘important’, ‘don't know/depends’, ‘unimportant’ or ‘should not be included’. Panellists were provided with comment boxes to provide reasons for their responses, suggest additional items or suggest modifications to wording of items.
Analysis of Delphi rounds and providing feedback to the panel
In most of the Delphi studies, items that were endorsed as essential or important by 80% or more of each panel were accepted, whereas items that were endorsed by 70–79% were put back to the panels to be rerated in the subsequent survey round. Items endorsed by less than 70% of the panel were rejected. For a small number of Delphi studies, the required endorsement rate was increased to 90% or decreased to 70% to reflect differences in overall endorsement rates. For example, Australian Indigenous panels tended to have high endorsement rates across items, so the cut-off for inclusion was raised to 90%.Reference Hart, Jorm, Kanowski, Kelly and Langlands29 By contrast, Japanese experts were less likely to rate items highly and more often used the don't know/depends option, so the cut-off was lowered to 70%.Reference Colucci, Kelly, Minas, Jorm and Suzuki35
When items were rerated, feedback was given to panel members about the ratings of all the panels on each item, as well as their own ratings. They were then given an opportunity to rerate the items in the subsequent survey round. Items that received low ratings (typically under 70%) were not rerated as experience has shown that rerating does not result in such major changes that the endorsement threshold (typically 80%) is reached.
Reliability of Delphi results
Data on the reliability of expert panel judgements could be obtained from Delphi studies that were performed on the same topic at two time points. This was done for suicide first aid by comparing common items from two Delphi studies on how to support a suicidal person.Reference Ross, Kelly and Jorm32, Reference Kelly, Jorm, Kitchener and Langlands36 The correlation across item frequencies was 0.84 between 22 professionals in the earlier study and 41 professionals in the later one. Similarly, there was a correlation of 0.77 between endorsement frequencies for a panel of 16 consumers and carers in the earlier study and 35 consumers from the later study. Given the passage of 6 years between the studies and the small size of some of the panels, this shows a high degree of reliability.
Five of the Delphi studies also looked at agreement between professional, consumer and carer panels within the same Delphi study (summarised in Table 1). Despite considerable variation in source of expertise, the level of agreement across expert panels is very high.
Table 1 Correlations across items in endorsement frequencies for different types of expert panels

Construction of guidelines from endorsed items
Guideline documents were constructed from the endorsed items by connecting them together under headings to make a coherent text. The guidelines were sent back to the expert panellists for comment and final approval before publication.
Guidelines for English-speaking countries
Guidelines have been developed for assisting with a range of mental health problems, as summarised in Table 2. All have involved the use of both professional and lived-experience expert panels, with 80% or greater endorsement required from all panels for inclusion in the guidelines. Given the need to keep guidelines up to date, two of the guidelines – on suicidal thoughts and behaviours and non-suicidal self-injury (NSSI) – have been revised in new studies. Other guidelines have been developed to assist people in high-risk groups or settings (see Table 3).
Table 2 Guidelines for assisting people with specific mental health problems in English-speaking countries

NSSI, non-suicidal self-injury.
a. N varies depending on Delphi round.
Table 3 Guidelines for assisting people with mental health problems from high-risk groups and settings in English-speaking countries

a. N varies depending on Delphi round.
Although there is broad agreement across various types of experts on appropriate first aid actions, the various Delphi studies have noted differences as well, which are summarised in Table 4. The areas of difference are diverse and influenced by the type of first aid situation (e.g. the urgency of action) and the type of person in the role of first aider (e.g. adolescent versus adult). Nevertheless, there are some common themes across a number of these studies. Professionals place a greater emphasis on privacy, confidentiality and on first aiders not straying into professional roles. Consumers place greater emphasis on autonomy in decision making and talking about feelings, whereas carers place greater emphasis on taking action to protect the person.
Table 4 First aid actions given greater emphasis by different types of experts

NSSI, non-suicidal self-injury.
a. This study had a ‘lived-experience’ panel consisting predominantly of consumers.
Guidelines for Asian countries
As summarised in Table 5, guidelines have been developed for assisting a suicidal person in various Asian countries, where professionals from individual countries were used as expert panellists. However, other guidelines for assisting a person with psychosis have been developed using professional experts from a range of Asian countries. All of these Delphi studies required 80% or more endorsement for inclusion in the guidelines, except for the study on first aid for a suicidal person in Japan,Reference Colucci, Kelly, Minas, Jorm and Suzuki35 which used a criterion of 70% or more, due to the greater tendency of Japanese experts to give responses of don't know/depends.
Table 5 Guidelines for assisting Australian Aboriginal and Torres Strait Islander people with mental health problems

a N varies depending on Delphi round.
None of these guidelines have had expert panels of consumers or carers because of the rarity of consumer and carer advocacy organisations in these countries. Another limiting factor was that the Delphi studies were carried out in English due to resource limitations. This has also limited the participation of consumer and carer experts as they were less likely to have the high level of English comprehension required. This may have resulted in bias towards the expertise of clinicians who have had Western training.
Guidelines for Australian Aboriginal and Torres Strait Islander people
A range of guidelines were developed for Aboriginal and Torres Strait Islander people, as summarised in Table 6. All but one of these guidelines used Aboriginal or Torres Strait Islander clinicians as experts; in the case of problem gambling, it was not possible to recruit an all-Aboriginal panel. As with Asian countries, it proved impossible to find sufficient Aboriginal consumer and carer advocates to tap into lived-experience expertise. Nevertheless, it was found in the studies of suicidal thoughts and behaviours and NSSI that most of the Aboriginal professionals had personal experience as well as professional experience, so they could draw on these different sources of expertise.Reference Armstrong, Ironfield, Kelly, Dart, Arabena and Bond37, Reference Armstrong, Ironfield, Kelly, Dart, Arabena and Bond38 All of these Delphi studies required 90% or greater endorsement for inclusion, with the high criterion set because of the high rates of item endorsement by these experts.
Table 6 Guidelines for assisting people from Asian countries with mental health problems

a. N varies depending on Delphi round.
Cross-cultural generalisability
Because Delphi studies to develop suicide first aid guidelines have been carried out for a range of Asian countries and high-income English-speaking countries, it has been possible to compare the results to see whether they are similar across countries and cultures.Reference Jorm, Ross and Colucci39 Comparing results for English-speaking countries, Sri Lanka, Japan, India, the Philippines and for refugees and immigrants, correlations across items in endorsement rates were all 0.60 or above, but were higher for countries that are socioeconomically similar. These results indicate that suicide first aid actions are generalisable across countries and cultures to some degree. These actions include assessing the risk of suicide, listening to the person, showing care and respect and ensuring the person's safety. However, there is also some cultural specificity, indicating a need for local tailoring of the guidelines. For example, differences were found regarding how appropriate it was thought to be for a first aider to dissuade a person from suicide and to try to solve their problems, and there was variation related to availability of services.
Similarly, it was possible to compare the ratings of Aboriginal and Torres Strait Islander professionals with those of experts from English-speaking countries. For ratings of NSSI items, the Aboriginal and Torres Strait Islander panel had a correlation of 0.73 with the English-speaking consumer panel and 0.71 with the English-speaking professional panel.Reference Armstrong, Ironfield, Kelly, Dart, Arabena and Bond37 Similarly, the correlations for items on suicidal thoughts and behaviours were 0.79 and 0.77, respectively.Reference Armstrong, Ironfield, Kelly, Dart, Arabena and Bond38 Again, these results indicate a high degree of cross-cultural generalisability. However, there were also differences, e.g. in communication issues and evaluation of urgency in taking action.
Implementation of the guidelines
The aim of mental health first aid guidelines is to improve the supportive behaviours of the public towards people with mental health problems. However, it has been noted both in the literature on clinical practice guidelines and on Delphi studies that these are not sufficient to produce changes in behaviour and that specific implementation strategies are necessary.Reference Jorm26, Reference Grimshaw, Thomas, MacLennan, Fraser, Ramsay and Vale40 Below is a review of strategies that have aimed to implement the guidelines in practice.
Guiding the content of training courses
The guidelines were primarily developed to inform the content of MHFA training courses. In developing the first edition of the Australian MHFA course,Reference Kitchener and Jorm41 it was recognised that there was little evidence on which to base mental health first aid strategies for the public. As the guidelines in Tables 2 and 3 have been developed over time, they have been used to inform the content of subsequent editions of the Australian Standard MHFA course (for adults helping adults),Reference Kitchener, Jorm and Kelly42–Reference Kitchener, Jorm and Kelly44 the Youth MHFA training course (for adults helping youth),Reference Kelly, Kitchener and Jorm45–Reference Kelly, Kitchener and Jorm47 MHFA for medical and nursing students to support their peersReference Bond, Jorm, Kitchener and Reavley48, Reference Davies, Beever and Glazebrook49 and for developing a new Older Person MHFA course (for adults helping older people)Reference Kitchener, Jorm and Kelly20. The mental health first aid guidelines for Aboriginal and Torres Strait Islander people (see Table 5) have been used to inform the content of an Aboriginal and Torres Strait Islander MHFA course which is taught by instructors from those communities.Reference Hart, Kitchener, Jorm and Kanowski50 The key elements of the various guidelines have been summarised in the form of an action plan, which is taught in the course. The most recent version of the MHFA Action Plan is:
(a) approach the person, assess and assist with any crisis
(b) listen and communicate non-judgementally
(c) give support and information
(d) encourage the person to get appropriate professional help
(e) encourage other supports.Reference Kitchener, Jorm and Kelly43
There have been 18 controlled trials of the Standard and Youth MHFA courses, of which 10 trials of the second and subsequent editions of the courses were informed by the mental health first aid guidelines listed in Tables 2 and 3. A recent systematic review and meta-analysis of MHFA trials showed improvements up to 6 months following training in mental health first aid knowledge, recognition of mental health problems, beliefs about effective treatments, stigma, confidence and intentions to help, and in the amount of mental health first aid provided.Reference Morgan, Ross and Reavley51
The Standard and Youth MHFA courses have been widely implemented in Australia, with over 0.5 million people trained by 2017, which is over 2% of the population. MHFA training has spread from Australia to more than 20 other countries, with over two million people trained globally.Reference Jorm and Kitchener52
A teen MHFA course has also been developed for adolescents aged 15–18 years to learn how to assist their peers,Reference Hart, Kelly, Kitchener and Jorm53 with the content based on a Delphi study.Reference Ross, Hart, Jorm, Kelly and Kitchener30 In this course, the expert-consensus messages have been summarised by an action plan:Reference Hart, Mason, Kelly, Cvetkovski and Jorm19
(a) look for warning signs
(b) ask how they are
(c) listen up
(d) help them connect with an adult
(e) your friendship is important.
A randomised controlled trial comparing teen MHFA with physical first aid showed improvements in mental health first aid intentions and confidence to help a peer, an increase in number of adults rated as likely to be helpful and a reduction in stigmatising attitudes.Reference Hart, Morgan, Rossetto, Kelly, Mackinnon and Jorm54
The revised suicide first aid guidelinesReference Ross, Kelly and Jorm32 have been used to develop a 4-hour training course for the Australian public in how to assist a suicidal person,Reference Kelly, Blee and Claesson55 but at present no evaluation has been published. In Japan, guidelines have been used to develop a 2-hour course on depression and suicide first aid for medical staffReference Kato, Suzuki, Sato, Fujisawa, Uehara and Hashimoto56 as well as a 2.5-hour suicide gatekeeper training course.Reference Hashimoto, Suzuki, Kato, Fujisawa, Sato and Aoyama-Uehara57 Randomised controlled trials of the course for Japanese medical staff have found improvements in suicide first aid competence and confidence,Reference Nakagami, Kubo, Katsuki, Sakai, Sugihara and Naito58, Reference Suzuki, Kato, Sato, Fujisawa, Aoyama-Uehara and Hashimoto59 as did an uncontrolled trial of the gatekeeper training course.Reference Hashimoto, Suzuki, Kato, Fujisawa, Sato and Aoyama-Uehara57
The guidelines on eating disordersReference Hart, Jorm, Paxton, Kelly and Kitchener60 have been used to develop a 4-hour course on mental health first aid for eating disorders.Reference Hart, Jorm and Paxton61 An uncontrolled trial with Australian university students and staff found that knowledge of appropriate mental health first aid strategies increased and was maintained at 6-month follow-up. Some participants reported providing assistance to a person with a suspected eating disorder, with some of those assisted seeking professional help as a result.
Various guidelines for English-speaking countries have informed a Japanese training course for professional caregivers of people with alcohol problems, including psychiatric service providers, mental health welfare workers and nursing-care staff.Reference Aoyama-Uehara62 However, no evaluation data have been reported.
Guidelines on Iraqi refugeesReference Uribe Guajardo, Slewa-Younan, Santalucia and Jorm34 have been used to inform a 7-hour Australian training course for community workers on how to assist Iraqi refugees with depression and post-traumatic stress disorder. An uncontrolled evaluation (with measures at pre-, post- and 6-months follow-up) found a number of improvements, including in mental health first aid knowledge, confidence to help and stigma.Reference Uribe Guajardo, Slewa-Younan, Kitchener, Mannan, Mohammad and Jorm63 However, no change in helping behaviours was found over the follow-up period.
Providing mental health first aid information on the internet and in print
Documents on mental health first aid guidelines have been provided as free downloads on the internet.Reference Hart, Jorm, Paxton and Cvetkovski64 An evaluation has been carried out on the usefulness and impact of these guidelines on people who download them. People using these resources were asked to complete a pop-up questionnaire at the time of the download and were then followed up a month later to ask what use they had made of the guidelines. Most people reported that they downloaded the guidelines because their job involved contact with people with mental illness. Although the response rate at follow-up was only 22%, there were people who reported that they had used the guidelines to assist someone and that the person had sought professional help as a result. The same methodology was used in a study of a French-language version of the eating disorders guidelines that was made available on a website aimed at French college students.Reference Melioli, Rispal, Hart, Chabrol and Rodgers65 Results were similar, with a small minority of people reporting that they used the information to assist someone, including encouraging professional help.
Guidelines have also been used to provide print information. Psychosis first aid guidelines have been included in a book for patients and their families, but no evaluation has been carried out on the impact of this book.Reference Compton and Broussard66
Evaluating the quality of mental health first aid information
Suicide first aid guidelines have been used as a standard to evaluate the quality of information presented on suicide-prevention websites.Reference Jorm, Fischer and Oh67 A checklist was developed from the guidelines to score whether 26 suicide-prevention actions were recommended on each website. The quality of information was found to be highly variable, with scores ranging from 1 to 19. In an effort to improve the quality of the information provided, a randomised controlled trial was carried out on a feedback intervention. A report on a website's quality was sent to a random half of the website administrators, while the other half served as controls. However, the feedback reports were not found to have any effect when the quality of the websites was reassessed 6 months later.
Assessing the quality of mental health first aid responses
Mental health first aid guidelines have been used to assess quality of mental health first aid intentions and actions in surveys of the general public, most of whom have had no mental health training. The assessment on intentions involved presenting a respondent with a vignette describing a person with a mental health problem and then asking the respondent what they would do if this person was someone they knew and cared about. The assessment on actions involved asking what the respondent had done to help an actual person with a problem similar to the one portrayed in a vignette. Schemes for scoring the quality of responses was developed based on the MHFA Action Plan taught in MHFA courses. This approach was used to examine the quality of intentions in Australian adults,Reference Rossetto, Jorm and Reavley68, Reference Rossetto, Jorm and Reavley69 British university students,Reference Davies, Wardlaw, Morriss and Glazebrook70 Sri Lankan university students,Reference Amarasuriya, Reavley, Rossetto and Jorm71 Japanese high school studentsReference Yoshioka, Reavley, Rossetto and Jorm72 and Australian youth and high school students.Reference Yap, Reavley and Jorm73–Reference Mason, Hart, Rossetto and Jorm75 The quality of actions was also examined in Australian adults,Reference Rossetto, Jorm and Reavley68, Reference Rossetto, Jorm and Reavley69, Reference Rossetto, Jorm and Reavley76 Australian youthReference Yap and Jorm77 and Australian high school students.Reference Mason, Hart, Rossetto and Jorm75 In general, these studies have found that the quality of mental health first aid intentions and actions is low.
Discussion
Limitations
There are a number of limitations of the existing guidelines. The first relates to the breadth of the evidence base. In contrast to physical first aid guidelines which uses evidence from trials, case series or animal evidence,Reference Singletary, Zideman, De Buck, Chang, Jensen and Swain78 all of the mental health first aid guidelines are based on expert opinion. There is also a lack of evidence on whether actions based on the guidelines lead to better health and well-being outcomes. A second limitation is that some of the guidelines were based only on professional expertise, as it was not possible to recruit experts with lived experience. Thirdly, all of the Delphi studies for Asian countries were carried out in English rather than the local languages, which may have biased the recruitment of experts towards those with Western training and limited the opportunity for participation by experts with lived experience. Finally, the authors of this review were involved in the studies on the guidelines, so this is not an independent review. Most of the guideline implementation has been carried out by those that developed the guidelines, but there is considerable scope for others to use them to inform training and other educational programs.
Future directions
A major gap is the lack of guidelines that are appropriate for low- and middle-income countries. People in these countries may differ from those in high-income countries in their vocabulary to describe mental health problems and crises, in the emphasis on individualistic versus collectivistic values, in social role constraints on taking action and in the availability of formal mental health services. Wherever possible, such guidelines should be developed in local languages and have diverse panels, including experts with lived experience.
There is a need for further exploration of the cross-cultural generalisability of guidelines. Although the ideal might be to develop a full suite of guidelines for each country and cultural group, this would be a mammoth task that is likely to be beyond the available resources. However, a set of universally applicable guidelines is also unlikely to be realistic, so solutions involving a compromise need to be explored.
There is also a need to extend the evidence informing guidelines beyond expert consensus where possible. Although such evidence is difficult to obtain for mental health first aid situations, there may be opportunities to collect experimental or observational evidence in some crisis circumstances, such as panic attacks and following a traumatic event.
Guidelines need to be regularly updated as evidence accumulates and consensus on best practice evolves. Physical first aid guidelines have been revised on a 5-yearly cycle by the International Liaison Committee on Resuscitation.Reference Singletary, Zideman, De Buck, Chang, Jensen and Swain78 With mental health first aid guidelines, only two have undergone revision and these were 6 years apart. To keep all existing guidelines up to date, Mental Health First Aid International has begun to revise them on a regular cycle.
Funding
A.F.J. is supported by a National Health and Medical Research Council Senior Principal Research Fellowship.
Acknowledgement
Betty Kitchener provided comments to improve the manuscript.











eLetters
No eLetters have been published for this article.