Approximately 18% of adults with intellectual disabilities (lifelong limitations in adaptive functioning evident in early life) living in the community display aggression, self-injury, property destruction or other socially inappropriate behaviours (e.g. sexual disinhibition, screaming or hitting out, etc.) in their lifetime.Reference Bowring, Totsika, Hastings, Toogood and McMahon1,2 Some 24 000 adults with intellectual disabilities are at risk of being admitted to specialist psychiatric assessment and treatment units, often because of the display of such behaviours.2,3
Research suggests that these individuals are subject to unnecessary long-term psychotropic medication use, poorer health, abuse and social exclusion.Reference Bowring, Totsika, Hastings, Toogood and McMahon1,Reference Cooper, Smiley, Jackson, Finlayson and Allan4 International studies indicate that adults with intellectual disabilities are more likely to visit the emergency department for psychiatric issues,Reference Durbin, Balogh, Lin, Wilton and Lunsky5 return to the emergency department within 30 days of discharge,Reference Durbin, Balogh, Lin, Wilton, Selick and Dobranowski6 be in long-term in-patient care and experience premature mortality.Reference Lin, Balogh, Chung, Dobranowski, Durbin and Volpe7 Failure to effectively address behaviours that challenge before a crisis arises causes significant distress and burden to families and consequent breakdown of placements,Reference Taggart, McMillan and Lawson8,Reference Painter, Ingham, Trevithick, Hastings and Roy9 in addition to significant healthcare and societal costs. A recent census of the Transforming Care Programme10 in England, a national initiative to drive improvements in the care of people with intellectual disabilities who display behaviours that challenge, indicated minimal change in relation to the number of in-patient admissions, length of hospital stay, out-of-area placements and antipsychotic medication use, confirming concerns about the lack of progress in the care of this population group across the country.11 Intensive support teams (ISTs) are community services that complement the community intellectual disability services and have been in operation since the early days of community care.Reference Davison, Mcgill, Baker and Allen12,Reference Hassiotis13 However, there is little evidence to recommend a preferred IST model, and there are no nationally specified outcomes for IST care. The National Institute for Health and Care Excellence (NICE)14 recognised the importance of such specialist treatment services, but did not find sufficient evidence that they were clinically effective or that they reduced costs. Hassiotis et al have reported the typology of ISTs, which led to the identification of two models, independent and enhanced.Reference Hassiotis, Walsh, Budgett, Harrison, Jones and Morant15 The aim of the present study was to examine the clinical and cost-effectiveness of the two IST models at 9 months follow-up.
Method
Study design
The primary and secondary outcomes were collected at baseline and 9 months follow-up. At the time of study completion, there were UK-wide public health measures implemented because of the COVID-19 pandemic, and in-person assessments could not take place between March 2020 and January 2021.
Service and participant recruitment
The research team prepared a matrix of all identified IST services in England stratified by model type, case-load size and area. The service managers of ISTs representing the two models were randomly invited to take part in the study. If they refused or did not respond, the next service in the matrix was approached until the required number of ISTs and participants were enrolled. The study inclusion criteria for services were as follows: ISTs operational for at least a year and ISTs funded for the duration of the study; for patient participants, the inclusion criteria were as follows: adults aged 18 years or over with a clinical diagnosis of mild to profound intellectual disabilities, and being under the care of an IST (either model) including new referrals. Those with a primary diagnosis of personality disorder or substance misuse, or a clinical decision that taking part in the study would be inappropriate because of risks, were excluded. Potential participants and their family/paid carers were approached by researchers and, where available, staff from the Clinical Research Networks to seek expressions of interest to take part in the study.
Consent statement
Participants provided written and/or audio-recorded verbal consent for in person or online assessments, respectively. For participants with intellectual disabilities who did not have capacity to make an informed decision about taking part in this study, we obtained written and/or audio-recorded agreement from a personal/nominated consultee.
Ethics statement
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human patients were approved by the London Bromley Research Ethics Committee (approval number 18/LO/0890). The study was registered with ClinicalTrials.gov (identifier NCT03586375), the Integrated Research Application System (identifier 239820) and the National Institute for Health Research (NIHR) Central Portfolio Management System (identifier 38554).
Outcomes
The primary outcome was change in challenging behaviour as measured by the carer-reported Aberrant Behaviour Checklist-Community version 2 (ABC-C).Reference Aman, Singh, Stewart and Field16 Secondary outcomes were mental health comorbidity (Psychiatric Assessment Schedule for Adults with Developmental Disabilities Checklist; PAS-ADD Checklist),Reference Prosser, Moss, Costello, Simpson, Patel and Rowe17 clinical risk (Threshold Assessment Grid; TAG)Reference Slade, Powell, Rosen and Strathdee18 and quality of life (Quality of Life Questionnaire; QoL-Q).Reference Shalock and Keith19 The ABC-C, PAS-ADD and QoL-Q have been validated for use with people with intellectual disabilities. The TAG is widely used in clinical practice to capture clinical risk in patients with mental illness, and has been used previously in a population with intellectual disabilities.Reference Hall, Parkes, Samuels and Hassiotis20 Quality-adjusted life-years (QALYs) were derived from the EQ-5D-5LReference Herdman, Gudex, Lloyd, Janssen, Kind and Parkin21 scores. If the participant with intellectual disability had sufficient reading ability, a researcher aided completion of a self-report version of the EQ-5D-5L. It is recommended that the proxy EQ-5D-5L should also be completed for adults with intellectual disabilities. Use of hospital and community services was obtained with the study-adapted Client Service Receipt Inventory,Reference Beecham and Knapp22 covering the previous 6 months. At 9 months follow-up, service use for the previous 6 months was extrapolated to 9 months.
Additional information
We also collected sociodemographic details, Adaptive Behaviour Scale – Short-Form (SABS)Reference Hatton, Emerson, Robertson, Gregory, Kessissoglou and Perry23 score as proxy of intellectual disability (higher scores indicate mild intellectual disability), medication use, number of hospital admissions and changes in accommodation.
Sample size
The sample size was calculated to detect a difference of 0.45 s.d. in primary outcome score. Assuming two IST models, this required 96 participants per group (192 in total) with 5% significance (two-sided), 80% power and an intraclass correlation coefficient of 0.02.Reference Hassiotis, Poppe, Strydom, Vickerstaff, Hall and Crabtree24 After inflation for 15% loss to follow-up, the estimated sample size was 113 participants per model (226 participants in total).
Statistical analyses
A detailed statistical plan was developed a priori and reviewed by the oversight Study Steering Committee. All analyses were carried out with Stata/IC version 16.0 for Windows.25 All hypothesis testing was conducted with a two-sided significance level of 5%, with corresponding 95% confidence intervals.
Clinical effectiveness
The primary outcome was estimated with a mixed-effects linear regression model, with change in ABC-C score as the outcome, a fixed effect for IST type as the main exposure and a random effect for IST to account for clustering within services. We carried out unadjusted modelling, then age, gender, accommodation type, level of intellectual disability (SABS score), level of risk (baseline TAG score), presence of autism and/or attention-deficit hyperactivity disorder, number of physical comorbidities and presence of organic, affective and psychotic disorders (as determined by the PAS-ADD) were identified as potential confounders and were included in an adjusted model. Continuous secondary outcomes were analysed with statistical models analogous to those for the primary outcome. Binary outcomes were analysed with mixed-effects logistic regression models and were unadjusted. Analyses of secondary outcomes were considered exploratory. Predictors of missingness of the primary outcome were examined with mixed-effects logistic regression. Where there were up to 20% missing items for the ABC-C, TAG and QOL-Q, they were replaced by the mean score of items present. Where items were missing for the PAS-ADD, they were replaced by a code indicating the participant was negative for the given condition.
Health economic analysis
A detailed health economic analysis plan was also developed a priori and reviewed by the oversight Study Steering Committee, and followed similar principles to the statistical analysis plan regarding assumptions. All analyses were carried out with Stata/IC version 16.0.25
Economic evaluation
Perspective
The cost-effectiveness analysis adopted the perspectives of health and social care, which covers hospital and community health, social care service and voluntary support provided by not-for-profit organisations. Wider societal perspective also includes the cost of unpaid support to the participant by family and friends.
Valuation of resource use
Costs of the IST service models were derived by combining data on annual salary, working time, overheads, number of sessions with participants, information on case-loads and referrals over 12 months. Travel costs to home visits were included where this was noted. The annual cost was then weighted to derive a cost per study participant for each IST model over 9 months. Unpaid support costs were calculated with the market price approach, the hourly rate of a home care worker was used for those not in employment and if employed, the carer hourly wage rate. All unit costs were for the financial year 2020/2021.
Cost-effectiveness
We analysed differences in mean health and social care costs and wider societal costs at 9 months in turn between the IST models, by regressing total cost from each perspective on IST model, baseline costs, total ABC-C score, health-related quality of life tariffs and a range of clinical and sociodemographic indicators. Non-parametric bootstrapping was used to estimate 95% confidence intervals for mean costs. Significance was set at P < 0.05.
Cost-effectiveness was explored with the net benefit approach,Reference Brouwer, Rutten, Koopmanschap, Drummond and McGuire26,Reference Stinnett and Mullahy27 with effectiveness measured in terms of the primary outcome measure (ABC-C score), and QALY gains were derived by developing value sets from the EQ-5D-5L by means of a cross-walk to the EQ-5D-3L value setsReference van Hout, Janssen, Feng, Kohlmann, Busschbach and Golicki28 at each time point. Uncertainty around the cost and effectiveness estimates was represented by cost-effectiveness acceptability curves.Reference Fenwick and Byford29
In sensitivity analyses, we examined whether adjustment for baseline characteristics affected the main findings. Those variables identified as significantly associated with missingness were then added to the baseline covariates used in main analyses and new incremental cost-effectiveness ratios were re-estimated.
COVID-19 impact and adaptations
Three National Health Service (NHS) sites withdrew their participation when the NIHR suspended all non-COVID-19-related research in March 2020. To carry on with recruitment, we applied for and received ethical approval to complete the consent process and research assessments remotely, using digital platforms (e.g. Zoom, telephone calls, scanned copies via email). Challenges to the study included digital poverty (e.g. lack of computer/smartphone), insufficient knowledge of using digital platforms and where a participant could receive support from if doing so, difficulty in assessing whether a patient with intellectual disabilities had sufficient verbal ability to provide consent remotely and delays in obtaining contact details for consultees.
Results
Clinical outcomes
The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) diagram (Fig. 1) presents the participant flow into the study. Enrolment took place between September 2018 and May 2020, with the last participant assessment in January 2021. There was an 8% attrition rate because of the following reasons: uncontactable (n = 12), death (n = 2, of which one was because of COVID-19), missing follow-up assessment window (n = 2), imprisonment (n = 1) and excessive stress during the pandemic (n = 1).
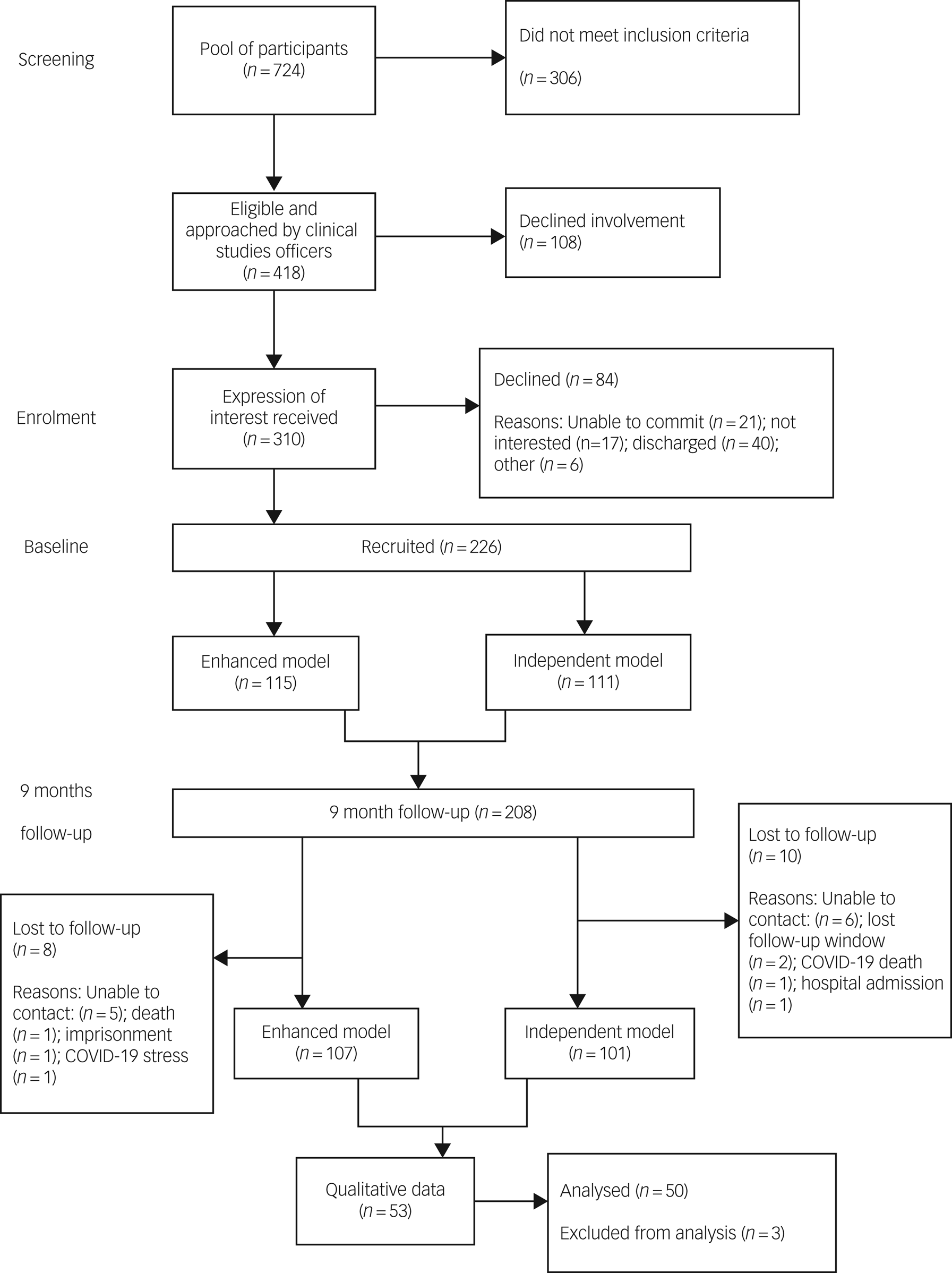
Fig. 1 STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) diagram.
Demographic characteristics of adults with intellectual disabilities per IST model at baseline and 9-month follow-up are presented in Table 1. The median age of participants was 29 years old (interquartile range (IQR) 23–39) and the majority were single male of White ethnicity. More than 60% of participants had comorbid developmental disorders. The whole cohort level of adaptive ability was 52 (s.d. = 24). Participants in the two models differed in the number of reported hearing or visual problems (enhanced 52% v. independent 68%; P = 0.018) and education status (enhanced 45% v. independent 32%; P = 0.035). At follow-up, participants were more likely to be receiving care from the enhanced IST compared with those still in contact with the independent IST (enhanced n = 78, 74% v. independent n = 45, 45%; P = 0.001). The median time adults with intellectual disabilities were seen from the enhanced ISTs was 20 months (IQR = 12–33) compared with 13 months in independent ISTs IQR = 10–22).
Table 1 Baseline sociodemographic and clinical characteristics by intensive support team model

IQR, interquartile range; ADHD, attention-deficit hyperactivity disorder.
* P<0.05.
Primary outcome
Baseline mean total ABC-C scores were similar between IST models (enhanced 64, s.d. = 34; independent 62, s.d. = 32) (Supplementary Table 1 available at https://doi.org/10.1192/bjo.2023.74/). The mean ABC-C scores were lower at 9 months for both IST models (enhanced 56, s.d. = 34; independent 49, s.d. = 32) (Supplementary Table 1). Both unadjusted and adjusted analyses found no statistically significant difference in total ABC-C score change between IST models at 9 months (adjusted β = 4.27; 95% CI –6.34 to 14.87) (Table 2). The only predictors of missingness were physical health conditions.
Table 2 Change in clinical outcomes of intensive support teams at 9 months in terms of independent intensive support teams
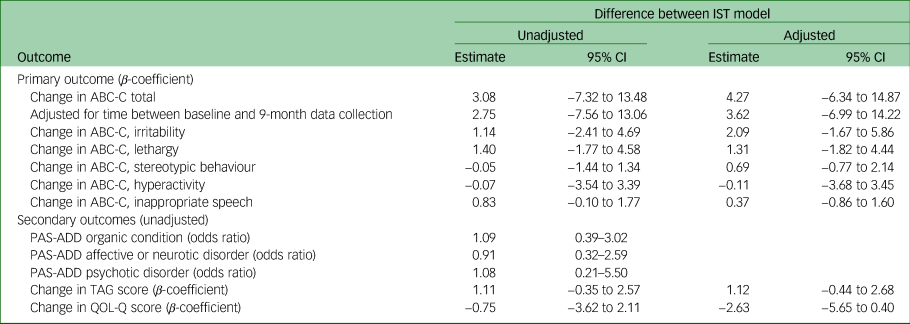
ABC-C, Aberrant Behaviour Checklist-Community version 2; PAS-ADD, Psychiatric Assessment Schedule for Adults with Developmental Disabilities Checklist; TAG, Threshold Assessment Grid; QOL-Q, Quality of Life Questionnaire.
Secondary outcomes
No statistically significant differences were found in any of the secondary outcomes between IST models at 9 months (Table 2, Supplementary Table 1).
Medication use
The mean number of medications prescribed at baseline was the same for both models (n = 5). At follow-up, the mean number was slightly reduced in the independent model (four for the independent versus five for the enhanced). At baseline, psychotropic medication was prescribed at similar proportions in both models: antipsychotic (enhanced 17% v. independent 18%) and other psychotropic (enhanced 35% v. independent 30%). The relative proportions of prescribed antipsychotics and other psychotropics did not change at follow-up: antipsychotics (enhanced 18% v. independent 20%) and other psychotropics (enhanced 31% v. independent 32%). Of those who were on psychotropics, over two-thirds were prescribed more than one medication in both models.
Psychiatric hospital admissions and change in accommodation
Over the study duration, eight participants in the enhanced model and 11 participants in the independent were admitted to a psychiatric unit as a result of a mental health crisis. Nine (4%) participants moved accommodation during the study period. All but one participant lived in supported living or residential provision.
Cost evaluation
The average annual cost of teams in the enhanced model was £612 612 (£4980 per case), whereas the average annual cost of a team in the independent model was £647 812 (£10 122 per case) (Supplementary Table 2).
Service use
From an NHS/Personal Social Services perspective, the mean total cost over 9 months was £22 915.6 for the independent model and £19 037.6 for the enhanced model; the adjusted mean difference in costs was not statistically significant (£446.55; 95% CI −5637.60 to £7519.30).
From a societal perspective the mean total cost over 9 months was £31 850.8 for the independent model and £29 852.8 for the enhanced. The adjusted mean difference in costs was not statistically significant (−£855.80; 95% CI −£8342.54 to £6059.69).
The mean use of in-patient, out-patient and day patient health services over the 9-month follow-up period are reported in Supplementary Table 3. Duration of in-patient stay, out-patient attendances, day hospital contacts and emergency (accident and emergency department) attendance, were broadly similar for both models. Notably, participants in the independent model spent longer, on average, as in-patients than those in the enhanced model (mean 8.63 days (s.d. 39.98) v. 5.26 days (s.d. 28.10). Participants in the independent model had, on average, more contacts with their general practitioner than participants in the enhanced model (mean 4.88 days (s.d. 14.20) v. 3.47 days (s.d. 3.96) attendances), although these were not statistically significant.
Cost-effectiveness
There are no statistically significant differences in QALYS in any of the comparisons of the service models at 9 months (Supplementary Table 4). Results from the regression analysis using the two outcomes of total ABC-C score and QALYs are summarised with incremental cost-effectiveness ratios in Supplementary Table 5.
Probability estimates were plotted for a range of implicit monetary values attached to improvements in total ABC-C score and QALY gain over 9 months under an NHS and societal perspective, in turn (Supplementary Figs 1−4).
The independent model had a low likelihood (approximately 50%) of being more cost-effective than the enhanced model if decision makers were not willing to pay anything for a unit improvement in the total ABC-C score. The likelihood of cost-effectiveness rose to 70% if willingness to pay for an improvement in total ABC-C score rose to £1000. Under a broader perspective, which includes cost of unpaid support, the probability of the independent model being cost-effective when compared with the enhanced model at the standard NICE-preferred willingness-to-pay levels of £20 000–30 000 per QALY, was 52%. It is therefore unlikely that there are any economic gains from choosing one model of care over another. Controlling for factors contributing to missing data in health and social care costs in sensitivity analyses did not alter the findings of the main analyses.
Discussion
The study showed that both IST models currently in operation in England were associated with reduction in behaviours that challenge at 9 months follow-up, with comparable costs.
The participants in both IST models appeared to score at levels on risk similar to those who were admitted to hospital in a previous study of an in-patient psychiatric ward.Reference Hall, Parkes, Samuels and Hassiotis20 Another study of predictors on in-patient admission that used routine clinical data did not include a measure of risk.Reference Sheehan, Mutch, Marston, Osborn and Hassiotis30
Over 28 months, during which time we enrolled and assessed participants at two time points, there were 19 admissions, averaging fewer than one admission per month across all services that took part. However, this is at odds with the monthly data release by the NHS Digital Learning Disability Services Monthly Statistics at the end of 202031 (closest date to the end of the final participant 9-month follow-up), which shows that 90 were admitted to an in-patient unit that month. When we started the participant enrolment in the autumn of 2018, there were 125 first or readmissions. There are several considerations about the interpretation of this information. First, NHS Digital reports on both people with intellectual disabilities and people with autism, so it is possible that the figures are inflated because of the diversity of the patient cohort. Second, our reporting is based on 21 services whereas NHS Digital collects data from a greater number of services.
Most recently, Dodd et alReference Dodd, Laute and Daniel32 reported on a new model of integrating intensive support service with an in-patient unit for adults with complex needs, including behaviours that challenge, at risk of admission. The new remodelled service appears to have had increasing efficacy in preventing admissions in 90% of referrals in 2020; this was up from about 60% of those referred prior to remodelling. Placement of patients was maintained in up to 80% of cases. However, although duration of in-patient care was reduced from 18 months to less than 12 months as a result of the intensive support, delayed discharges remained mostly as a consequence of lack of suitable accommodation. Bohen and WoodrowReference Bohen and Woodrow33 and Mottershead and WoodrowReference Mottershead and Woodrow34 published initial findings for the Dynamic Support Database clinical support tool. Such work, although in its early stages, is promising and points toward prevention and intervention strategies that could contribute to the refinement of the specification of ISTs. The recent publication of the action planReference Sheehan and Hassiotis35 relating to ‘Building the Right Support’3 does not make reference to ISTs or how they fit into current practice, especially regarding the stated intent to ‘close inpatient facilities for people with learning disabilities and/or autism who display behaviour that challenges’. Therefore, there is still no specific guidance as to how ISTs are to be implemented across England. Other projects relating to the Transforming Care programme have yet to report findings and do not include examination of community support, intensive or routine (e.g. https://www.birmingham.ac.uk/schools/social-policy/departments/social-work-social-care/research/why-are-we-stuck-in-hospital.aspx).
Finally, the interplay between multiple medications including psychotropics and the display of behaviour that challenges is a complex one. Apart from the interactions between different pharmacological agents, changes in psychotropic medication regimens can also affect behaviour, as is well recognised.Reference Sheehan and Hassiotis35 Future research should consider a more granular approach to medication administration and prescribing, given the significant numbers of participants on psychotropics and other drugs.
The setting of ISTs (rural or urban areas) has not been analysed in this study because literature in other populations indicates that individual demographic and clinical characteristics, rather than location, are more likely to affect adverse outcomes such as hospital admissions.Reference Osborn, Lamb, Canaway, Davidson, Favarato and Pinfold36
The only studies including a health economic evaluation are by Iemmi et al,Reference Iemmi, Knapp, Saville, McWade, McLennan and Toogood37 who reported on costs of one IST delivering positive behaviour support to five patients associated with improved outcomes at a total cost of health and social care services of £2,296 per week. Hassiotis et alReference Hassiotis, Robotham, Canagasabey, Romeo, Langridge and Blizard38 highlighted that a specialist behaviour team maybe cost neutral when compared with treatment as usual.
The health economic evaluation of this multicentre study showed that the service costs of enhanced ISTs are not significantly different from the independent ISTs, and neither are the health-related quality-of-life gains. However, as the economic burden of behaviours that challenge remains substantial,10,14,Reference Hassiotis, Parkes, Jones, Fitzgerald and Romeo39 it is likely that costs could be offset by clinical improvements associated with IST care. Cost per case would range between £4980 and £10 122 based on number of referrals per model, enhanced and independent, respectively. However, the magnitude of that change would have to exceed the unit improvement in the total ABC-C score to be considered as clinically significant, and when all costs of health and social care are taken into account the cost differences between models are not significant. Previous research indicates that experts by experience expect larger differences as a result of interventions to be clinically meaningful than those reported in existing publications.Reference Hassiotis, Melville, Jahoda, Strydom, Cooper and Taggart40
Strengths and limitations
This study is the first, to our knowledge, to have systematically evaluated IST models in England. It was fully powered with very good retention of participants (<10% attrition), the COVID-19 pandemic notwithstanding. ISTs were representative of such services in England and the study participants representative of the population on IST case-loads, which minimise the risk of bias. The findings from this study are highly relevant to the support of very vulnerable individuals with intellectual disabilities in the community, and potentially applicable to other UK countries where they seek to establish similar approaches to the acute or preventive management of behaviours that challenge.
The study also has limitations. First, responses might be subject to respondent social desirability bias. Second, this was not a randomised controlled trial, so there may have been differences between groups that we were unable to measure and adjust for in the analyses. Third, the turnover of paid carers may have affected the reporting of behaviours that challenge if the carer had not known the person with intellectual disabilities for long enough. Fourth, the lack of statistical significance in clinical outcomes between models may be an indication that adults who are referred during a crisis will recover in the short to medium term as behaviour that challenges is a remitting/relapsing condition (regression to the mean).Reference Cooper, Smiley, Jackson, Finlayson and Allan4 Fifth, as we did not recruit participants at the point of referral to the IST, we must be cautious about the change that was achieved, as it has not taken into account any improvements made before study entry. Sixth, there may have been some effects from the COVID-19 pandemic, as 131 follow-up interviews were conducted from March 2020 to January 2021, but we were unable to fully adjust for it. For example, the pandemic may have exacerbated behaviours that challenge or affected the patterns and intensity of service use in both models. This is especially important, given the current disproportionate impact of COVID-19 on people with intellectual disabilities, including higher death rates.41 Finally, we did not collect process outcomes such as Care and Treatment Reviews (CTRs) completed by the teams, although it appears that almost half of those admitted had a CTR within 6 months of admission. Therefore, it is likely that CTRs may not be the sole reason for failing to prevent an admission.
In conclusion, our findings indicate that commissioners can choose which IST model is relevant to their localities, but also that there is a need to further investigate the critical ingredients of effective IST care and understand how best ISTs may work with and fit into the wider mental health service system. This information should be incorporated within the action plans about the right community support for adults with intellectual disabilities who display behaviours that challenge.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2023.74
Data availability
Anonymised data of the study are available from A.H. on request and subject to internal review of proposals.
Acknowledgements
The authors are grateful to the study participants who participated in the study. The research team is also grateful to the NIHR Clinical Research Network (CRN), all 21 research and development offices and the project advisory group of experts by experience, for their support and commitment to the study. In particular, we acknowledge the support and contribution of Narender Kaur, Lorna Bryan, Janet Seamer, Sandy Smith and Brendan Leahy from the Camden Disability Action (Synergy). We would also like to thank the Study Steering Committee, chaired by Professor Nora Grace, for their oversight of the study. Finally, we are grateful to previous members of the research team, Amy Walsh, Isobel Harrison, Dr Victoria Ratti, Jessica Budgett and Peiyao Tang, for their contribution to delivering the IST-ID study. We want to dedicate the work to the memory of Ms Rebecca Jones, statistician co-applicant, who passed away before completion of the second stage of the study.
Author contributions
A.H. is the chief investigator of this study. A.K. and L.H. prepared the manuscript with A.H. A.K. and L.H. carried out data collection. L.M. performed the analysis of clinical data, and R.R. and N.Y. performed analyses of the health economic data. A.H., N.K., L.H., L.M., I.H., N.M., K.C., P.E.L., L.T., R.R., N.Y., V.C. and B.L.E. have contributed to the interpretation and previous iterations of the manuscript and its intellectual content. They have all agreed to the published version.
Funding
This project is funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research (HS&DR) programme (reference number 16/01/24). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. A full version of the IST-ID study that this is part of has been published in https://www.journalslibrary.nihr.ac.uk/hsdr/CHDC1642/#/full-report.
Declaration of interest
None.









eLetters
No eLetters have been published for this article.