Introduction
Social anxiety disorder (SAD) is common and usually first occurs during adolescence (Kessler et al., Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2005; Merikangas et al., Reference Merikangas, Nakamura and Kessler2009), with almost all cases occurring by early adulthood (Beesdo et al., Reference Beesdo, Pine, Lieb and Wittchen2010). It is associated with high levels of impairment in education and work, social relationships, and day-to-day life (La Greca and Harrison, Reference La Greca and Harrison2005; Ranta et al., Reference Ranta, Kaltiala-Heino, Rantanen and Marttunen2009; Stein and Kean, Reference Stein and Kean2000; Wittchen et al., Reference Wittchen, Fuetsch, Sonntag, Müller and Liebowitz1999) and has a particularly low natural recovery rate in the absence of treatment (Bruce et al., Reference Bruce, Yonkers, Otto, Eisen, Weisberg, Pagano and Keller2005; Ranta et al., Reference Ranta, Kaltiala-Heino, Rantanen and Marttunen2009). Developing effective and scalable treatments for adolescent SAD will be important to offset the individual, NHS and societal costs associated with the disorder.
Cognitive therapy for SAD (CT-SAD) is a distinctive form of cognitive behavioural therapy (CBT) that is highly effective for adults (Mayo-Wilson et al., Reference Mayo-Wilson, Dias, Mavranezouli, Kew, Clark, Ades and Pilling2014). It aims to reverse the processes specified in the cognitive model of social anxiety developed by Clark and Wells (Reference Clark, Wells, Heimberg, Liebowitz, Hope and Scheier1995). Comparisons with other active treatments for adults have demonstrated that CT-SAD is superior to: two forms of group CBT, exposure therapy, interpersonal psychotherapy, psychodynamic psychotherapy, SSRIs, medication-focused treatment as usual, and placebo medication (Clark et al., Reference Clark, Ehlers, McManus, Hackmann, Fennell, Campbell and Louis2003; Clark et al., Reference Clark, Ehlers, Hackmann, McManus, Fennell, Grey and Wild2006; Leichsenring et al., Reference Leichsenring, Salzer, Beutel, Herpertz, Hiller, Hoyer and Leibing2013; Mörtberg et al., Reference Mörtberg, Clark, Sundin and Åberg Wistedt2007; Stangier et al., Reference Stangier, Heidenreich, Peitz, Lauterbach and Clark2003; Stangier et al., Reference Stangier, Schramm, Heidenreich, Berger and Clark2011). Individual CBT (including Clark and Wells’ CT-SAD) is recommended as the first-choice treatment for adult SAD in the current NICE Guideline (NICE, 2013), and was judged to be most cost-effective in the long-term. The Guideline noted the limited data for psychological interventions in youth SAD, and concluded that CBT was the most promising intervention, and further that CT-SAD should be considered for the treatment of adolescents with social anxiety. There is currently a lack of studies examining moderators of CBT for youth SAD, although for CBT in general, from the studies that have been carried out, it seems that factors such as modality and parental involvement may not affect response (Creswell et al., Reference Creswell, Waite and Hudson2020).
In line with this, a randomised controlled trial with adolescents (Ingul et al., Reference Ingul, Aune and Nordahl2014) demonstrated that CT-SAD was superior to both a psychological placebo and a generic form of CBT on self and clinician ratings at post-treatment. At 12-month follow-up when the two treatment arms were compared, it was found that gains and group differences persisted. The study is significant as it demonstrates treatment specificity of cognitive therapy for SAD in adolescents. Whilst the findings are notable, CT-SAD was not implemented fully in the study. Interventions for socially traumatic memories were not included, and psychoeducation and anxiety hierarchies, which are not part of CT-SAD, were used. Subsequently, Leigh and Clark (Reference Leigh and Clark2016) undertook a pilot study to examine whether the full CT-SAD could be delivered to adolescents with appropriate age-relevant adaptation (Cognitive Therapy for Social Anxiety Disorder in Adolescents; CT-SAD-A). At the end of treatment, all participants were free of all diagnoses and this improvement was maintained at follow-up, with an average reduction of 87% on a social anxiety symptom scale. Taken together, these findings are promising and point to the potential value of delivering CT-SAD early in the course of social anxiety. However, the therapist in the pilot study had received extensive training in CT and we know from research with socially anxious adults that specific CT competencies are needed for good outcomes (Ginzburg et al., Reference Ginzburg, Bohn, Höfling, Weck, Clark and Stangier2012). Therefore, the question arises as to whether modestly trained therapists in routine Child and Adolescent Mental Health Services (CAMHS) can also achieve good patient outcomes. This will be important to demonstrate if CT-SAD-A is to be disseminated more widely. Related to this, it is also necessary to estimate the NHS costs associated with training therapists and delivery of CT-SAD-A, as this can provide a first insight into the economic viability of the treatment in routine clinical practice.
The study had two main aims: first, to train NHS CAMHS therapists to deliver the adapted treatment and to assess young people’s outcomes; and second, to estimate the cost of delivering CT-SAD-A within an NHS CAMHS setting.
Method
Ethics and consent
The study was approved by the NHS South Central – Oxford B Research Ethics Committee (REC reference: 16/SC/0315) and University of Reading Research Ethics Committee (UREC 16/43). Informed consent/assent was sought from parents and from young people.
Treatment
CT-SAD-A, which is the adolescent version of CT-SAD for adults based on the Clark and Wells (Reference Clark, Wells, Heimberg, Liebowitz, Hope and Scheier1995) model, is a distinctive form of CBT delivered in 14 weekly 1.5-hour sessions provided on a one-to-one basis. CT-SAD-A involves: development of an individualised version of the Clark and Wells (Reference Clark, Wells, Heimberg, Liebowitz, Hope and Scheier1995) model; an experiential exercise to help patients discover the unhelpful effects of self-focused attention and safety behaviours; video feedback; systematic training in externally focused, non-evaluative attention; and behavioural experiments. When indicated, there may also be work on: socially traumatic memories; anticipatory worry and post-event processing; low self-esteem; parental beliefs and behaviours; and bullying and its consequences. Further details of the treatment with case examples are described by Leigh and Clark (Reference Leigh and Clark2016) and can also be found at: www.oxcadatresources.com
Training
The training employed a two-stage approach (Beidas and Kendall, Reference Beidas and Kendall2010; Rakovshik and McManus, Reference Rakovshik and McManus2010) involving an initial workshop followed by a period of supervised practice. The 2-day workshop involved a combination of teaching, video material, and experiential exercises and role-plays. Clinicians were provided with a detailed treatment manual and a memory stick containing extended training videos ahead of the workshop (these resources are available to access at: www.oxcadatresources.com). After the workshop, clinicians attended weekly supervision via video-link or telephone in small groups. Supervision sessions involved detailed discussion of the previous treatment session, review of questionnaire measures, discussion of any problems that had arisen, and then step-by-step planning for the next session. Videotaped treatment sessions were discussed on a regular basis in supervision.
Setting and therapists
Two NHS Foundation Trusts in England participated: Oxford Health and Berkshire Healthcare NHS Foundation Trusts. Seven therapists (four from Oxford Health) completed the training: three clinical psychologists and three CBT therapist. All had at least 2 years of experience using CBT and of working with young people. One therapist attended the initial training workshop and three supervision sessions but then withdrew from the study due to a change in circumstances, therefore n = 6 therapists for the report of clinical outcomes and n = 7 therapists for cost outcomes.
Inclusion and exclusion criteria for adolescent patients
Young people (11–17.5 years) with a primary DSM-5 diagnosis of social anxiety disorder routinely referred to CAMHS were eligible. If young people were prescribed psychotropic medication the dosage must have been stable for 2 months. Young people with established autistic spectrum disorders, learning disabilities, suicidal intent or recurrent self-harm, or identified by social services as currently ‘at risk’ due to child protection concerns were not eligible.
Outcome measures
The Anxiety Disorders Interview Schedule (ADIS) – child and parent report (Silverman and Albano, Reference Silverman and Albano1996) was administered at baseline and follow-up to young people and parents by psychology postgraduates trained to a high level of inter-rater reliability [kappa/intraclass correlation was >.85 for diagnoses and Clinical Severity Ratings (CSR) across all anxiety disorders and for SAD specifically]. For each disorder, a CSR was assigned (from 0 to 8), with scores of 4 or more indicating presence of a disorder.
The self-report version of the Liebowitz Social Anxiety Scale for Children and Adolescents (LSAS-CA-SR; Masia-Warner et al., Reference Masia-Warner, Klein and Liebowitz1999) assesses social anxiety. Fear and avoidance of 24 social situations are rated on a 4-point scale (total range 0–144). It has well-established psychometric properties (Masia-Warner et al., Reference Masia-Warner, Storch, Pincus, Klein, Heimberg and Liebowitz2003).
The Social Participation and Satisfaction Questionnaire (Alden and Taylor, Reference Alden and Taylor2011) assesses participation in and satisfaction with relationships.
Concentration in class was assessed by asking young people to rate their ability to concentrate in class in the preceding week (0–100) (Leigh and Clark, Reference Leigh and Clark2016).
Symptoms of anxiety and depression were assessed using the child version of the Revised Child Anxiety and Depression Scale (RCADS; Chorpita et al., Reference Chorpita, Yim, Moffitt, Umemoto and Francis2000). It has robust psychometric properties (Chorpita et al., Reference Chorpita, Moffitt and Gray2005).
Process measures
Several measures covering central processes in cognitive models of social anxiety (Clark et al., Reference Clark, Ehlers, McManus, Hackmann, Fennell, Campbell and Louis2003) adapted for use with adolescents (Leigh and Clark, Reference Leigh and Clark2016) were used to guide therapy.
The Child & Adolescent Social Summary Weekly Rating Scale (CASSWRS; Clark et al., Reference Clark, Ehlers, McManus, Hackmann, Fennell, Campbell and Louis2003) was used as an additional measure of social anxiety, obtaining an average score (range 0–8).
The Child & Adolescent Social Cognitions Questionnaire (CASCQ) covers 22 common social anxiety-related negative thoughts. A mean belief rating is obtained (range 0–100).
The Child & Adolescent Social Attitudes Questionnaire (CASAQ) is a 41-item scale measuring social anxiety-related beliefs. A mean belief rating is obtained (range 1–7).
The Child & Adolescent Social Behaviour Questionnaire (CASBQ) is a 29-item scale of common social safety-seeking behaviours. A mean score is obtained (range 0–3).
All of these measures can be obtained from: www.oxcadatresources.com
Treatment acceptability rating
At the end of treatment, participants rated how acceptable they found the treatment (two items rated on a 5-point scale: ‘I was satisfied with the treatment’ and ‘I would recommend the treatment to others’).
Health economic records
Clinician logs (clinician includes both supervisors and therapists) were designed to capture the amount of healthcare resources (i.e. qualified staff time) necessary to implement CT-SAD-A. They were completed by both supervisors and therapists, who recorded the amount of time spent in activities related to the CT-SAD-A treatment, including training, supervision, preparation and delivery of CT-SAD-A. Data recorded in the clinician logs were used to calculate the total mean amount of qualified staff time used by the NHS per adolescent treated. Results were stratified by type of staff time use.
Analysis
Comparisons between pre-treatment and follow-up were made with non-parametric Wilcoxon signed ranks tests. The Z-statistic is presented, with associated p-values and effect size estimates (r). An effect size of ≥0.1 is interpreted as small; ≥0.3 medium; and ≥0.5 is large (Cohen, Reference Cohen1988). Reliable change on our primary outcome measure, the LSAS-CA-SR, was defined as a pre–follow-up change exceeding the measurement error of the scale (Evans et al., Reference Evans, Margison and Barkham1998), based on data from Masia-Warner et al. (Reference Masia-Warner, Storch, Pincus, Klein, Heimberg and Liebowitz2003), equating to a change of 16.13 or more. Reliable and clinically significant improvement (RCSI) was defined as pre–follow-up change of at least 2 standard deviations (SD) from the original mean (Evans et al., Reference Evans, Margison and Barkham1998), equating to a drop of at least 48.75 points.
In the cost analyses, for each study participant, all components of treatment costs, stratified by category of resource use, were computed by multiplying units of resource use by their unit costs (Curtis, Reference Curtis2017) (see Supplementary material, Table S1), expressed in 2016/17 UK pounds sterling (£). Mean imputation was used to handle missing data, as they referred to the time spent on face-to-face therapist contact with the young person, and were highly deterministic (i.e. readily identifiable and standardised given observed practice). A conditional imputation method was conducted whereby missing data were estimated as an average of known durations for the specific patient. Results were reported in terms of total amount of qualified staff time and associated NHS costs for training and supervision as well as in terms of mean values of qualified staff time and associated NHS cost per patient treated, with variability around the mean measured by standard deviations.
Results
Characteristics of patients
The ten females and two males had an average age of 15.17 years (SD = 1.80, range 12–17). The sample was predominantly White British (10/12), which was representative of the local areas. None reported being prescribed psychotropic medication. All met DSM-5 criteria for SAD. Only two patients had no co-morbid diagnoses; GAD was present in eight patients, and depression (either major depressive disorder or dysthymia) in three. There were five diagnoses of specific phobia pre-treatment across four patients, with one patient diagnosed with two specific phobias. One patient had a diagnosis of post-traumatic stress disorder and one had a diagnosis of panic disorder.
Seven patients received the planned 14 weekly therapy sessions, two patients received 10 weekly sessions, and one patient each received 11 sessions, 12 sessions and 17 sessions. Seven patients received at least one booster session. The follow-up assessment was carried out on average 2.88 months (SD = 1.15, range 1.16–4.63) after the final weekly therapy session.
Outcomes
Social anxiety symptoms
Table 1 presents baseline characteristics and social anxiety symptom outcomes at post-treatment and follow-up for patients. Treatment was associated with a significant reduction in social anxiety symptoms on the LSAS-CA-SR at follow-up (Z = –3.06, p = .002, r = 0.62). Scores dropped on average 66.80% over time (range 3–100%; Fig. 1) and ten participants, 83% of the sample, made a reliable improvement. Nine of these participants also demonstrated a reliable and clinically significant improvement. RCADS social anxiety T-scores showed a significant and large decrease over treatment (Z = –2.93, p = .003, r = 0.60): eight patients were in the borderline or clinical range at pretreatment, based on age and gender (T-score > 65), whereas only one patient remained in the clinical range at follow-up.
Table 1. Social anxiety symptom outcome measures
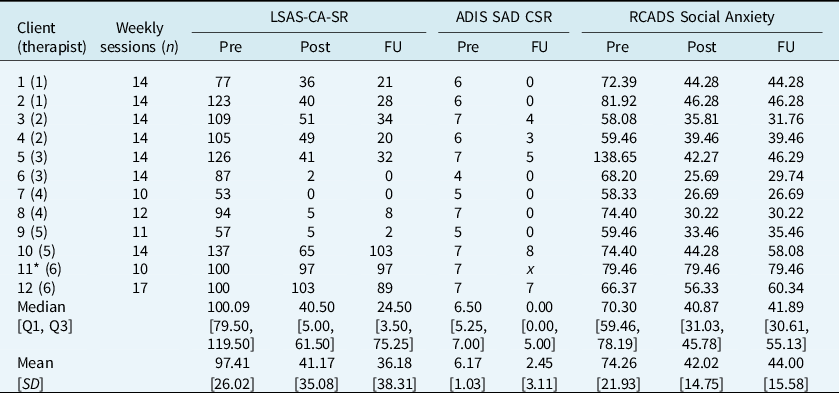
Pre, pre-treatment assessment; Post, post-treatment assessment; FU, follow-up assessment; LSAS-CA-SR, Liebowitz Social Anxiety Scale – Child & Adolescent – Self-Report Version; ADIS SAD CSR, Anxiety Disorders Interview Schedule Social Anxiety Disorder Clinical Severity Rating; RCADS, Revised Children’s Anxiety & Depression Scale; SD, standard deviation; Q, quartile.
* Participant 11 did not attend the follow-up assessment. Scores from their final weekly appointment are presented and included in follow-up summary statistics. x indicates missing data.

Figure 1. Individual patient LSAS-CA-SR scores at the following measurement points: pre-assessment, mid-treatment, at the end of weekly sessions, and at the follow-up assessment.
Diagnostic outcomesFootnote 1
Seven patients (64%) lost their primary diagnosis of SAD (see Table 1). Six lost their diagnosis of GAD, and three diagnoses of specific phobia were lost (one patient had two phobias at pre-treatment and lost one of these at follow-up). Depressive disorders increased from three to four by follow-up. Of the four patients who retained their diagnosis of SAD at follow-up, one had lost their diagnosis of depression, two had retained their diagnosis of depression, and one had acquired a new diagnosis of depression. One patient lost their diagnosis of SAD but had become depressed at follow-up. Six patients (55%) were free of all diagnoses at follow-up.
Other clinical outcomes
As can be seen in Table 2, there was a significant drop in RCADS depression subscale scores1 over time (Z = –2.94, p = .003, r = 0.63). For 10/11 patients, depression scores were below threshold (T < 65) at follow-up (whilst 5/11 had been below threshold pre-treatment). ID4 continued to show elevated symptoms of depression at follow-up, and also developed a new diagnosis of depression over the course of treatment, whilst losing their SAD diagnosis (see diagnostic outcomes section). RCADS depression score for the other patient (ID12) who had been assigned a new diagnosis of depression during the course of treatment was above threshold at the start of treatment and showed a small decrease at follow-up.
Table 2. Related clinical outcome measures
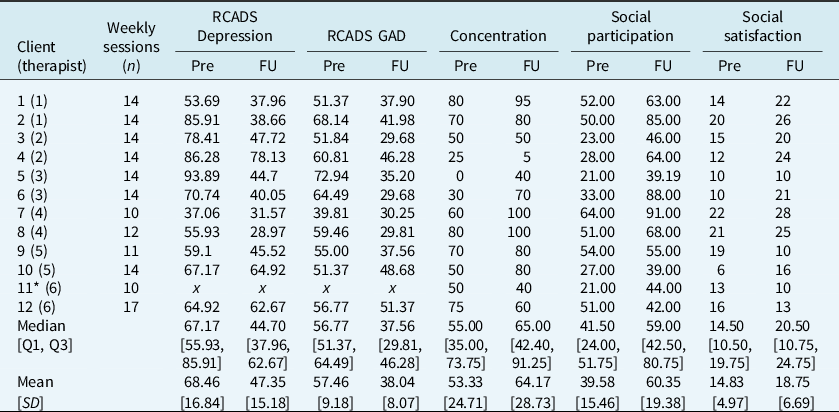
Pre, pre-treatment Assessment; FU, follow-up assessment; RCADS, Revised Children’s Anxiety & Depression Scale; SD, standard deviation; Q, quartile.
* Participant 11 did not attend post-treatment assessment. Scores from their final weekly appointment are presented where available and included in follow-up summary statistics. x indicates missing data.
There was a large and significant drop in RCADS GAD scores1 over the course of treatment, with all patients scoring below threshold at follow-up (Z = –3.02, p = .003, r = 0.64). The group as a whole showed large improvements in social participation (Z = –2.90, p = .004, r = 0.59) and moderate improvements at trend level in social satisfaction (Z = –1.96, p = .050, r = 0.40).
The group showed a small to medium improvement in concentration (r = 0.30), although this was non-significant (Z = –1.49, p = .137). As can be seen in Table 2, one young person showed no change (ID10) and three a deterioration in their concentration (ID4, ID11 and ID12). Patients ID10, ID11 and ID12 are those young people who did not show a clinically significant improvement on the LSAS-CA-SR and whilst ID4 lost their diagnosis of SAD, they developed a new diagnosis of depression during treatment.
Table 3 provides descriptive statistics for the process measures. All patients reported some reduction in ratings of belief in social cognitions and the group as a whole showed a large reduction in belief ratings on the ASCQ (Z = –3.06, p = .002, r = 0.62). For nine patients these reductions were substantial (belief rating reduced by 88–100%), and these same patients also showed a clinically significant improvement on the LSAS-CA-SR. There was a large reduction in safety behaviour use by the end of treatment (Z = –2.85, p = .004, r = 0.58), and a large reduction in negative social attitudes (ASAQ) (Z = –2.67, p = .008, r = 0.55). Only one patient (ID10) showed a strengthening of their negative social attitudes, and they also retained their SAD diagnosis at follow-up.
Table 3. Social anxiety process measures
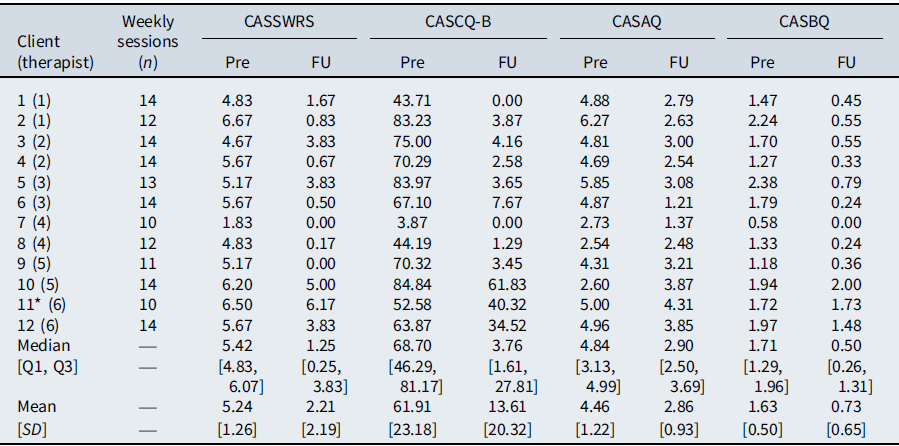
Pre, pre-treatment assessment; FU, follow-up assessment; CASSWRS, Adolescent Social Summary Weekly Rating Scale; CASCQ-B, Adolescent Social Cognitions Questionnaire Belief Ratings; CASAQ, Adolescent Social Attitudes Questionnaire; CASBQ, Adolescent Social Behaviour Questionnaire.
* Participant 11 did not attend their follow-up assessment. Scores from their final weekly appointment are presented and included in the follow-up summary statistics.
Treatment acceptability
Eleven young people completed the treatment acceptability scale at the follow-up assessment. All of them agreed (either ‘somewhat’ or ‘completely’) with the statements ‘I was satisfied with the treatment’ and ‘I would recommend the treatment to others’.
Cost of treatment delivery in NHS CAMHS
Mean supervisor time per therapist attending each workshop was 278 minutes (SD = 157) and associated mean NHS cost was £287 (SD = 162). Mean supervisor time per therapist per case supervision week was 50 min (SD = 14) and associated mean NHS cost was £51.50 (SD = 14.6) (Supplementary material, Table S2). Mean therapist time for each workshop attended was 420 min (7 h) (SD = 0) and associated mean NHS cost was £294 (SD = 0). On average, each therapist participated in 24 (SD = 12) case supervision sessions. Mean therapist time per case supervision session attended was 73 min (SD = 40) and associated mean NHS cost was £51 (SD = 28) (Supplementary material, Table S3). Each adolescent treated received on average 5279 min (around 88 h) (SD = 1301) of qualified clinician time (including therapist’s training and case supervision) and this would cost the NHS £4047 (SD = 1003) per adolescent treated. The main cost driver was face-to-face delivery of the CT-SAD treatment (£1861; SD = 358 per adolescent treated) (Supplementary material, Table S4).
Discussion
The findings of the training case series provide preliminary evidence that good outcomes can be achieved from the delivery of CT-SAD-A in standard NHS CAMHS during supervised practice. Patients were routine referrals to CAMHS services. All patients presented with a primary diagnosis of SAD and received CT-SAD-A provided by CAMHS therapists as part of their training in this novel treatment. The group as a whole demonstrated large and significant improvements in social anxiety symptoms, as well as associated clinical outcomes. Substantial improvements in the proposed psychological mechanisms that are proposed to drive change in this treatment (social beliefs and behaviours) were also reported and treatment acceptability was high. To the best of our knowledge, this is the first detailed cost analysis of treatment for SAD in young people. The economic analysis indicated that the total cost to the NHS of the CT-SAD-A treatment was £4047 (SD = £1003) per adolescent treated, of which £1861 (SD = £358) referred to the specific estimated cost of face-to-face delivery. The remaining cost was for training and supervising therapists who were not previously familiar with the treatment.
As in the first case series of CT-SAD-A, undertaken by our group (Leigh and Clark, Reference Leigh and Clark2016), the drop in LSAS was substantial (67%) at follow-up. The mean change of 61 points on the LSAS reported here compares favourably with the figures reported for adult CT-SAD; e.g. mean changes of 43 and 46 on the LSAS reported by Clark and colleagues (Clark et al., Reference Clark, Ehlers, McManus, Hackmann, Fennell, Campbell and Louis2003 and Clark et al., Reference Clark, Ehlers, Hackmann, McManus, Fennell, Grey and Wild2006, respectively). From visual inspection of the LSAS-CA-SR (see Fig. 1), it is clear that nine of the 12 patients reported considerable improvement in symptoms. They reported an average reduction of 85% on the measure (vs 13% for the other three patients) and attained clinically significant improvement. Seven of the nine patients lost their primary SAD diagnosis and the other two showed reductions on their ADIS CSR SAD rating (ID3: 7 to 4; ID5: 7 to 5). All nine patients improved to below clinical thresholds on the social anxiety and GAD subscales of RCADS. These findings, and our loss of diagnosis rate of 64% for the sample overall, compare favourably with outcomes of children and young people with SAD from trials of more general forms of CBT. For example, Ginsburg et al. (Reference Ginsburg, Kendall, Sakolsky, Compton, Piacentini, Albano and March2011) reported recovery rates of 40% among children and young people with SAD who received 14 sessions of a generic form of CBT for anxiety.
Importantly, scores on measures of the psychological mechanisms that are targeted in CT-SAD-A all reduced substantially over the course of therapy for the nine improvers, in contrast to the non-improvers. On the CASCQ, the average reduction was 96% (89–100%) for the nine improvers vs 32% (23–46%) for the three non-improvers; on the CASBQ it was 77% (68–100%) vs 7% (–3–25%); and on the CASAQ it was 43% (2–75%) vs –4% (–48–22%).
Whilst we would not expect any treatment to be effective for all patients, it is interesting to consider why the three remaining patients responded considerably less well to therapy compared with the other nine. As can be seen from Fig. 1, it does not appear to be a function of SAD severity. Possible explanations include factors relating to how the treatment was delivered. It may be that the particular therapists for these patients did not gain as much from the training as the others, or had less time available, so had less time to prepare, were less able to conduct full length sessions (90 min), and as such were less able to facilitate in vivo behavioural experiments. Alternatively, it might be that differences in therapist allegiance affected uptake and delivery of CT-SAD-A techniques. In future, examination of therapist allegiance ratings and blind rating of therapist competency could shed light on these hypotheses. Larger trials would provide the opportunity to examine potential predictors of response to treatment, including therapist and patient-specific factors, more thoroughly and systematically.
Notably, the patient outcomes described are for those treated during the CAMHS therapists’ training, and so it is possible that the outcomes reported may be an under-estimate of patients’ potential gains and an over-estimate of economic costs, because we would expect therapists to achieve better outcomes as they accrue more experience. Future research would benefit from establishing the extent, and optimum modalities, for delivering therapist training in CT-SAD-A in order to achieve best outcomes. Notwithstanding these issues, the findings highlight the potential benefit of delivering CT-SAD to adolescents.
There are, of course, important limitations of the training case series, including the small sample, which only included two males, and uncontrolled design lacking a baseline assessment phase, which means we cannot rule out the possibility of symptom change due to the passage of time, or non-specific therapy effects. We would suggest that this is unlikely, as the patients had all experienced symptoms for at least 6 months in order to qualify for a diagnosis, and in many cases social anxiety had been present for much longer. We cannot rule out potential non-specific therapeutic benefits of therapist contact and support, and therefore a controlled comparison is needed to test this alternative explanation. Furthermore, longer term outcomes and examination of possible moderators of treatment outcomes should certainly be included in any further systematic evaluation.
Strengths of the study included the thorough assessment and training procedures that were implemented within the CAMHS context. A further strength of our study is the inclusion of a cost analysis, highlighted as lacking by NICE (NICE, 2013). The estimated cost of delivering treatment (excluding training and supervision of therapists) was £1861 per young person treated within our study, which was admittedly based on a small sample size. Nevertheless, in a tentative comparison with treatments for adults our cost compares favourably to NICE’s estimated cost of delivering CT-SAD per patient with adults (£2341) (Mavranezouli et al., Reference Mavranezouli, Mayo-Wilson, Dias, Kew, Clark, Ades and Pilling2015), which has been found to be most cost-effective when psychological and pharmacological interventions for SAD adults have been compared (NICE, 2013).
Our economic results need to be interpreted in light of some limitations. While the response rate of supervisor-completed economic logs was 100% throughout the study duration, therapist-completed economics logs had rates of missing values that ranged from 50 to 67% for various treatment session across all patients, and imputation methods had to be used to handle missing data. Using mean imputation reduced sample variability with the consequence that uncertainty around our cost estimates was under-estimated. It should also be noted that the way in which the training phase was conducted was less than optimal due to the fact that new therapists were recruited at different times throughout the training programme. Consequently, two cohorts of therapists were trained separately, causing a duplication of supervisors’ time in the training phase which led to inflated costs. In ‘real world’ practice, workshops could be delivered to much larger numbers of therapists. This should be examined in future studies. Finally, the lack of a control condition precludes any conclusions about cost-effectiveness (i.e. whether CT-SAD-A may be good value for money) in comparison with current usual practice.
Our preliminary findings suggest that therapists working in busy CAMHS settings can achieve good outcomes for routinely referred SAD patients even whilst undergoing their training in the therapy and our results point to the potential value of delivering the training more widely. Based on our small sample and working within the current CAMHS context, the cost of delivering CT-SAD-A with adolescents appeared to be no more than the cost of delivering CT-SAD with adults, and would be expected to bring greater economic advantages due to the earlier onset of benefits, including potentially related to increased engagement in education.
Supplementary material
To view supplementary material for this article, please visit: https://doi.org/10.1017/S1352465821000035
Data availability
The data that support the findings of this study are available from the corresponding author (E.L.), upon reasonable request.
Acknowledgements
We would like to express wholehearted thanks to the participating families, therapists, their service managers and clinical leads, and the R&D teams at the Oxford Health and Berkshire Healthcare NHS Foundation Trusts. We are also grateful for the comments of the other members of the Trial Management Group.
Financial support
This work was supported by the National Institute of Health Research (NIHR HTA 14/170/01; NIHR Research Professorship; C. Creswell; Senior Investigator (D.M. Clark)); Wellcome Trust (Clinic Research Fellowship (E. Leigh); Programme Grant (D.M. Clark). M.V. receives funding from the National Institute for Health Research (NIHR) Applied Research Collaboration Oxford and Thames Valley at Oxford Health NHS Foundation Trust, and the NIHR Oxford Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Ethics statement
All authors have abided by the Ethical Principles of Psychologists and code of Conduct as set out by the BABCP and BPS. Ethical approval for this study was gained from the local NHS Research Ethics Committee (REC reference: 16/SC/0315).
Conflicts of interest
David M. Clark is one of the authors of the cognitive model of social anxiety that CT-SAD-A is based on and has also played a central role in developing CT-SAD. No other conflicts of interest are declared.









Comments
No Comments have been published for this article.