Introduction
Telecare has become a ubiquitous part of social care offered by English local council adult social care departments, whether directly provided or commissioned from external partners. Outcomes of telecare use for older people have been extensively researched and studies of family and other unpaid/informal carers and telecare use have suggested that carers find that it offers reassurance (Jarrold and Yeandle, Reference Jarrold and Yeandle2009) and enables them to participate more fully in society (Carretero et al., Reference Carretero, Stewart and Centeno2015). However, less is known about if and how providers of telecare involve family and other unpaid/informal carers in the process of offering or providing it to older people and how this impacts on their caring role.
This paper is structured in five sections. The first explores the context of carers and telecare. In the second, details of the data sources on which this paper draws are provided and the methods used to sample, collect and analyse the data are described. The third section presents the findings and the fourth section discusses the implications of the findings in the light of Twigg and Atkin's (Reference Twigg and Atkin1994) conceptualisation of carer–practitioner relationships and locates them within the literature. In the final section, conclusions are drawn.
Background
Carers
In this paper, the term ‘carer’ is used to describe people who provide unpaid/informal support or care to another person: usually to family members or partners, but sometimes to friends or neighbours. The United Kingdom (UK) 2011 census found 6.8 million people or 12 per cent of the UK population self-identified as carers (Buckner and Yeandle, Reference Buckner and Yeandle2015: 8). Since many unpaid carers do not describe themselves as such (Colombo et al., Reference Colombo, Llena-Nozal, Mercier and Tjadens2011), this figure may be an underestimate. In England and Wales, 1.3 million carers are estimated to be older than 65 years and their numbers are increasing more rapidly than other age segments of the carer population (Carers UK, Reference Carers2015). Internationally, it has been estimated that in the United States of America, 43.5 million people provide unpaid care (National Alliance for Caregiving and AARP Public Policy Institute, 2015), whilst in the European Union (EU) 80 per cent of care is provided by carers (Hoffmann and Rodrigues, Reference Hoffmann and Rodrigues2010). Eurofound (2017: 45) estimates that approximately 12 per cent of the EU working-age population provide unpaid care, although percentages vary considerably among member states.
The importance of carers has been acknowledged in public policy in England for several decades. The Carers (Recognition and Services) Act 1995 (HM Government, 1995), the National Strategy for Carers (Department of Health, 1999), the Carers (Equal Opportunities) Act 2004 (HM Government, 2004) and an update of the National Strategy for Carers (HM Government, 2010) recognised and endorsed their role. The Care Act 2014 (HM Government, 2014) created a statutory duty for councils to assess carer needs and to support them in their own right.
Whilst some studies have shown positive aspects of caring (Carbonneau et al., Reference Carbonneau, Caron and Desrosiers2010), numerous studies highlight the potential adverse impact of caring on physical and mental wellbeing of the carer (Luengo-Fernandez et al., Reference Luengo-Fernandez, Leal and Gray2008; Rand and Malley, Reference Rand and Malley2014; Wolff et al., Reference Wolff, Spillman, Freedman and Kasper2016) and ability to remain in paid employment (Carers UK and Employers for Carers, Reference Carers2012; King and Pickard, Reference King and Pickard2013). The need for public services to offer more support to carers is often argued (Rand and Malley, Reference Rand and Malley2014; Moriarty et al., Reference Moriarty, Manthorpe and Cornes2015).
In this paper, our theoretical understandings of carers is aligned with Twigg and Atkin's (Reference Twigg and Atkin1994) typology of carers and their relationship with services providing or funding care. Their conceptual framework encompasses four models describing how carers are typically perceived:
(1) ‘Resources’: family or other unpaid carers are perceived as ‘the “given”, taken-for-granted’ (Twigg and Atkin, Reference Twigg and Atkin1994: 12) form of care provision, prior to and separate from any formal services. The aim is to maximise the care for the cared-for person; the needs and wellbeing of the carer in their own right are largely ignored.
(2) ‘Co-workers’: in this model carers provide care alongside statutory services. Formal providers recognise the interests and wellbeing of the carer but only insofar as the lack of carer wellbeing limits the quality of care for the cared-for person.
(3) ‘Co-clients’: the wellbeing of the carer is at the centre of attention and carers are supported in their own right by the formal service. Potential conflicts of interest between carer and cared-for person are also recognised.
(4) ‘Superseded’ carers: in this model the aim is to overcome caring, either by maximising independence for the cared-for person or recognising that caring is not needed anymore. This model also acknowledges situations in which caring puts too great a burden on the carer and the person needs to cease or change their care-providing role.
Telecare
Telecare is commonly described as ‘care provided at a distance’ (Curry et al., Reference Curry, Trejo Tinoco and Wardle2002: 1) and usually refers to electronic equipment installed in domestic settings that collect, process and relay information either to the user themselves (e.g. to remind them to do something), to someone in the near vicinity (typically a carer) or somewhere outside a user's home (usually a monitoring or call centre). The rapid rate of technological innovation and development has led to some terminological confusion because definitions can become out of date. Some eschew the term ‘telecare’ in favour of ‘remote care’ (Barlow et al., Reference Barlow, Curry, Chrysanthaki, Hendy and Taher2012).
Typically, telecare consists of a system of connected sensors and devices of various kinds that are worn by and/or dispersed around the user's home. They may require user activation (e.g. personal alarm buttons) or work ‘passively’ (e.g. pressure mats or exit sensors). This paper excludes equipment that sends health data directly to clinicians or enables users to communicate directly with health-care professionals (sometimes referred to as ‘telemedicine’). We also differentiate between stand-alone and monitored devices. Monitored devices generate and send an alert signal to a third party, typically a monitoring centre. Devices that alert carers via pagers or smartphones also belong to this category. Stand-alone devices just operate in the home and do not relay information elsewhere.
Telecare's potential for carers was first mentioned in the National Strategy for Carers (Department of Health, 1999) as a means to support their caring role by enabling an alert to be sent to a co-resident carer, e.g. if they are caring for someone with dementia who gets up during the night. The refreshed Carer Strategy (HM Government, 2010) took this example further by describing one of the main aims of telecare as being to allow carers to be away from the cared-for person, e.g. to enable them to remain in employment.
Interest and use of telecare in social care over the last two decades have grown (Doughty et al., Reference Doughty, Cameron and Garner1996; Woolham et al., Reference Woolham, Gibson and Clarke2006; Miles and Doughty, Reference Miles and Doughty2011), though telecare systems have been in use in sheltered housing schemes since the 1960s (Fisk, Reference Fisk2003). There are approximately 1.7 million telecare users in the UK (Gibson et al., Reference Gibson, Newton, Pritchard, Finch, Brittain and Robinson2016). Policy makers in England have made reference to telecare since the Department of Health Information Strategy (NHS Executive, 1998) and the Royal Commission on Long Term Care (1999). Telecare, from the outset, has been seen as a cost-effective way of delaying or preventing moves to long-term care and reducing the number of unplanned hospital admissions (Botsis and Hartvigsen, Reference Botsis and Hartvigsen2008). However, others have been more cautious in promoting these outcomes (Bayer et al., Reference Bayer, Barlow and Curry2007).
Studies of telecare's impact on carers have produced conflicting findings (Mortenson et al., Reference Mortenson, Demers, Fuhrer, Jutai, Lenker and DeRuyter2012; Davies et al., Reference Davies, Rixon and Newman2013; Madara Marasinghe, Reference Madara Marasinghe2016). Several found that telecare provides carers with reassurance or ‘peace of mind’ (Woolham, Reference Woolham2005; Jarrold and Yeandle, Reference Jarrold and Yeandle2009), and reduces stress and anxiety (Alaszewski and Cappello, Reference Alaszewski and Cappello2006; Jarrold and Yeandle, Reference Jarrold and Yeandle2009; Olsson et al., Reference Olsson, Engström, Skovdahl and Lampic2012) and carer burden (Mortenson et al., Reference Mortenson, Demers, Fuhrer, Jutai, Lenker and DeRuyter2012). However, other studies have not found any reduction of carer stress (Torp et al., Reference Torp, Hanson, Hauge, Ulstein and Magnusson2007). Some have also argued that telecare could add to carer burden because it renders the carer more ‘accessible’ and because it heightens the need to respond to technology-generated alerts (Alaszewski and Cappello, Reference Alaszewski and Cappello2006; Bowman et al., Reference Bowman, Hooker, Steggell and Brandt2013).
Methods
This paper is based on findings from a wider study of telecare provision in England (Woolham et al., 2018b). Exploring the involvement of carers was part of the wider research objective to investigate the strategic aims of telecare provision by local councils and how telecare was operationalised. The overall study adopted a three-stage, mixed-method design.
Stage 1: Interviews with telecare managers
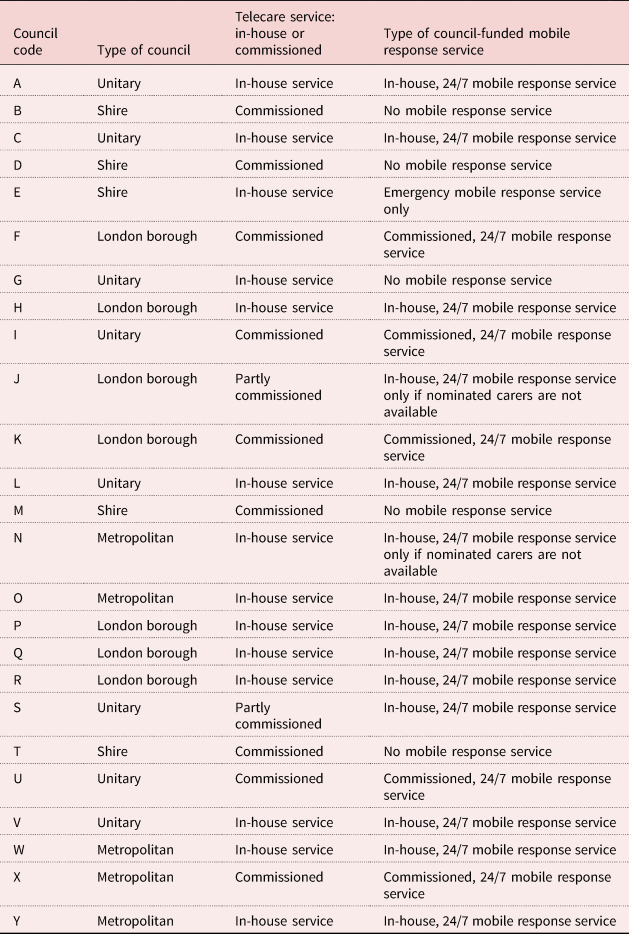
An initial purposive sample of 44 local councils (with social services responsibilities) was established from which a representative target sample of 25 were sought (we assumed that not every contacted council would wish to participate). Councils in the sample were selected according to the proportion of older people in their general population, the proportion of older people receiving long-term social care services, but also according to the distribution of the four different types of local council (shire, unitary, metropolitan and London borough) and different geographical regions in England. This larger sample was contacted by telephone and/or email and, if consent was given and a senior manager leading on telecare (telecare manager) could be identified, an interview was arranged. If no consent was given, the next council on the list was contacted until the final sample size was achieved. The final set of 25 participating councils (codes A–Y) was proportional to council type and consisted of:
• Eight unitary authorities (mix of urban and rural).
• Five metropolitan authorities (urban).
• Five shire counties (rural).
• Seven London boroughs (urban).
All geographical regions of England were represented (see Table 1).
Table 1. Overview of participating local councils in Stage 1 interviews
From the sample of 25 councils, 27 telecare managers were interviewed between May and August 2016. Interviews were all completed by telephone and audio-recorded with consent.
The semi-structured interview schedule focused on strategic aims of telecare provision and how these were operationalised and delivered, exploring assessment processes, installation, maintenance and arrangements to respond to telecare-generated alerts, what telecare equipment and services were offered to older people, and the support and information offered to self-funders. One question asked directly about carers: ‘What needs do unpaid carers have in your council that can be met through providing Telecare?’ A subset of questions asked telecare managers about strengths and weaknesses of telecare provision from different perspectives, including those of carers.
Stage 2: Case studies
To gain further, deeper knowledge about forms of telecare provision, from the sample of 25, four councils were sought to participate as case studies. Although all managers in Stage 1 initially indicated interest and ability to take part in Stage 2, one council withdrew and an alternative council was approached. The participating four councils (codes G, H, M and N) were purposefully selected because the Stage 1 interviews indicated that they had contrasting approaches to telecare provision, e.g. commissioned or in-house service provision, separate or combined assessments of social care needs and telecare, or availability/non-availability of in-house or commissioned response services.
In these sites, 21 interviews were undertaken from September to November 2016. The interviews were with ‘stakeholders’ in ‘typical’ telecare provision processes. Interviewees comprised four telecare commissioners, seven staff responsible for telecare assessments, four installers and six ‘responders’ (some staff had multiple roles). Three of the responders were employed by the council or a commissioned service, and three were family carers, all of whom were adult children of an older telecare user. One carer was from an area where the council provided an in-house response service, the others came from a council with no council-organised response service. All interviewees were nominated by participating councils (see Table 2).
Table 2. Overview of participants in interviews in the case studies in Stage 2
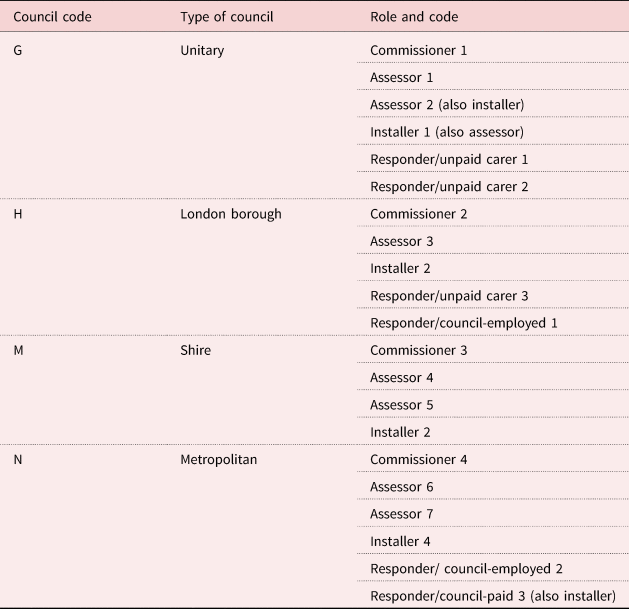
The questions followed the same themes as in Stage 1. Three questions asked directly about carers, e.g. one question asked for the needs of responding carers: ‘Are the needs of carers who respond when alarms go off also taken into account when service user assessments are done?’
Stage 3: Survey
To complement interviews in Stage 1 but to be able to involve all 152 English councils, an online survey using the platform SurveyMonkey was undertaken. The survey explored similar themes to interviews in Stage 1 and ran from November 2016 until January 2017. It comprised 58 open and closed questions, of which seven focused on or referred to carers’ involvement in telecare provision directly, e.g. ‘How could the needs of relatives and unpaid carers be met through providing telecare?’
A link was sent with an invitation to take part to all 152 English local councils, either to the telecare manager or if these could not be identified to the Director of Adult Social Services. The final response rate was 75 per cent (N = 114); 20 per cent of the responses were from commissioned telecare services which could clearly be linked to a council as responders were asked to give their name, role and the council they represented. Unidentifiable or anonymous responses and responses from telecare manufacturers, researchers or private individuals were excluded.
Analysis
Audio-recordings of all interviews were fully transcribed and entered into NVivo computer software to assist coding and analysis. Framework Analysis (Ritchie and Spencer, Reference Ritchie, Spencer, Bryman and Burgess1994) was adopted for this purpose as it provides a clear process for the analysis of large qualitative data-sets. Five distinct stages of analysis were undertaken: (a) including detailed data familiarisation, (b) development of thematic frameworks based on research objectives and new, potentially unexpected, emerging themes and sub-themes, (c) indexing/coding and (d) merging (‘charting’) of data according to these frameworks, here indexing all data on carers, both from the questions directly asking about carer involvement and also from the entire data-sets when carers were mentioned by respondents, and finally (d) interpretation of themes and sub-themes. Data on carers from open questions in the survey were examined for new emerging themes or sub-themes and then integrated in the existing frameworks.
Quantitative survey data were entered into SPSS v22 software and descriptive and comparative analyses were conducted.
Findings on carers from the separate analysis of quantitative data, interview data and open responses from the survey were combined (Sandelowski and Barroso, Reference Sandelowski and Barroso2007) and analysed to extract sub-themes for further interpretation. The comparative analysis was extended to include both quantitative and qualitative data and included, for example, exploring possible differences between in-house and commissioned provision of telecare. However, whilst the organisational approach to provision did not seem to impact on the involvement of carers, further analysis showed differences between different types of councils, and between councils that funded response services and those where unpaid carers were the main responders. These findings are presented and discussed below.
As data were predominately collected from senior managers and practitioners, it was felt that Twigg and Atkin's (Reference Twigg and Atkin1994) conceptualisation of carer–practitioner relationships would be helpful in framing the discussion.
Results
Three broad themes emerged from the analysis of data showing varied contexts in which carers were involved in the provision of telecare to older people and the responsibilities they assumed. These were:
• council strategies concerning carers and telecare;
• carers’ varied involvement in the telecare provision process;
• plans to increase involvement of carers and how to overcome current barriers to optimal use of telecare.
Carers and council telecare strategies
Both telecare manager interviews and the online survey sought details of what the council wanted to achieve through providing telecare services for older people. Its use to support carers was frequently mentioned. Twenty-four managers in interviews and 84 per cent in the survey indicated that the use of telecare reduced carer stress by providing reassurance or ‘peace of mind’, and that it gave carers more independence and improved their quality of life. For co-resident carers, telecare managers felt that telecare was able to alert carers of changes to the cared-for older person's wellbeing or whereabouts without the need for constant physical checks. Telecare managers also referred to the role of monitoring centres in supporting carers. When an alert was raised, either actively by the older person or by the telecare equipment itself, the call handler could establish a response was needed, either from a carer, a paid response service, the emergency services or a combination of these. Telecare managers also described how monitored telecare devices allowed carers to remain in employment:
We've also got a significant growing number of working-age carers who really worry about what can happen. It can be disruptive to their daily routine by having to be checking people and ringing them up, and so they're having the call centre as a buffer with telecare, it is allowing some people to juggle working life and family life and a caring life. (Telecare manager 4, council D, Stage 1)
The survey indicated that 27 per cent of councils offered a mobile response service as part of their telecare services where a member of staff visited telecare users in a ‘wellness check’ to ensure that the person for whom an alert had been raised was uninjured. Telecare managers felt that this service supported carers. The value was confirmed by one interviewed carer:
I wouldn't be without it … I wouldn't be able to go to work now with peace of mind if mum didn't have that. (Carer 1, council G, Stage 2)
Carers’ involvement in telecare provision
Assessments
Interviewed telecare managers felt that carers’ views were considered in telecare assessments because these assessments were often attended by carers; and the assessments tried to establish whether family members, friends or neighbours already provided support and could therefore assist with the service by monitoring or responding.
Whilst two telecare managers said that they also assessed carers in their own right in the context of telecare provision, none of the three interviewed carers could remember having been assessed, either as part of their relative's assessment or in a separate carer assessment.
Installation and maintenance of telecare
Councils used their own or commissioned staff to install telecare equipment. Telecare managers said that they involved carers at this stage to explain how equipment worked. Some councils also expected telecare users or their carers to take responsibility for maintenance and adjustment of devices and to alert the telecare service if a device malfunctioned. Though the survey suggested that telecare devices were programmed to alert the service provider that maintenance was required in a majority of councils (57%), a fifth (20%) said that they relied solely on telecare users or carers to inform them if equipment malfunctioned or did not address the problem for which it had been provided for some reason.
Survey findings indicated that 17 per cent of councils held telecare users or their carers responsible for basic maintenance, such as changing batteries and re-setting equipment. Interviews indicated that some councils would only service monitored devices, so users and carers were expected to carry out the maintenance and adjustment of ‘stand-alone’ equipment. For this, carers were usually given training:
Our telecare installers, they'll only install equipment with the client there, and the reason for that is, one, to make sure that it's appropriate for the individual, but it's also to help with that initial training of both the individual and their carers or responders, so that where there are needs for particular pieces of equipment to be adjusted or whatever, and when that's a responsibility of the client, there is a degree of training involved in that. (Commissioning manager 3, council M, Stage 2)
Interviews indicated that in eight of 25 councils carers were asked to refill medication dispensers. It was acknowledged this was an added responsibility but it was also claimed that medication dispensers supported carers because they reduced their workload:
Refills for pill dispensers … when we go through the information we basically show it to the family member saying, ‘This is how you programme it, you put the number of doses, the amount of times, and then you just fill it like this.’ Other times, certain pharmacists are happy to fill them … Pill dispensers can be what we call stand-alone, so we just drop it off and then it's their thing. (Installer 4, council N, Stage 2)
Some telecare managers were cautious about greater involvement of carers in the maintenance of some telecare equipment. They said that more complex equipment, such as epilepsy detectors or Global Positioning System- (GPS) based devices, needed specialist knowledge and their own staff were better able to service these. Some telecare managers also acknowledged that not every carer was comfortable or confident in setting up or maintaining equipment:
I think that's something that we are very mindful of, not overwhelming people. Quite often, when you've got an elderly person with a carer, that person maybe the person's partner. You are talking about people in their eighties. My dad is 74 years old, he is pretty techy, but not everybody is. And it's not always about age either, it depends on background and you can have somebody in their thirties, forties who really isn't technology minded or somebody in their eighties who can code on the computer. It's very person-specific. (Telecare manager 6, council F, Stage 1)
Responding to alerts generated by telecare
Carers played a key role in responding to alerts generated by telecare, both from stand-alone devices and monitored equipment where the technology initially alerted a monitoring/call centre call handler.
Though some councils offered a response service as part of their telecare services, others relied solely on carers to respond to alerts raised in a monitoring centre, when no emergency services were needed (see Table 3).
Table 3. Who provides ‘first-line’ response to alerts generated by telecare in the monitoring centre?
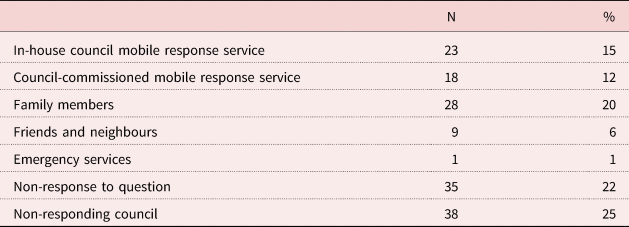
Note: N = 152.
In 20 councils where there was no in-house or commissioned response service, telecare was not provided if an older person could not identify and ‘nominate’ someone to attend when needed. There were differences between councils that provided response services and those that relied either entirely or mainly on carers to respond to telecare alerts generated in monitoring centres: whilst six rural counties that took part in the survey offered an in-house or commissioned response service, 15 relied on carers. Similar results were also found in some large unitary councils. Their large geographical size will have been an underlying reason.
The provision of a mobile response did not always alleviate carer responsibilities. One carer reported that almost all telecare alerts received by the call centre would result in the call handler contacting her to respond rather than using triage protocols or their own response staff. This not only hampered this carer's ability to work but increased her stress and anxiety for her mother's safety:
They kept ringing me and I said, ‘Go and check on her, that's the service you're paid to do.’ That's what was happening at the beginning, they would just ring me every time the alarm went off … I gave my number because I'm the closest out of everyone, but they were just using that as a back-up service. But when I spoke to the social worker he went, ‘No, that shouldn't be happening, they're doing it wrong’, and he spoke to them and said, ‘You have got to attend. Only call [the daughter] if you can't deal with whatever's there and she will come down.’ (Carer 3, council H, Stage 2)
Following the social worker's intervention which initiated a change to the triage protocol, this carer said that she was subsequently contacted only when necessary.
Managing the telecare package and decommissioning equipment
In the Stage 3 online survey 77 respondents, in Stage 1 interviews 16 managers and in Stage 2 case studies five installers and three commissioners reported situations in which telecare equipment had been decommissioned at the request of either the older recipient or, more often, their carers. Reasons cited were because they felt it did not meet needs, including instances where the older person was not able to use it, e.g. personal alarms requiring user activation provided to people with dementia who were unable to operate the device reliably. In other cases, equipment was abandoned and removed because the carer felt that it had become too invasive and caused anxiety to the older person, which in turn impacted negatively on them as carers. Some requests to remove telecare had arisen because too many devices were provided, causing confusion among older people and carers. One carer reported that her mother had been provided with a wrist-worn falls alarm but was unable to use it, and a pressure mat, but the carer did not understand what need the mat was supposed to address. Both devices were removed after a few months at the carer's request:
Talking about it now, saying about the wrist band and remembering about the mattress, I even forgot she had that one, it feels like they just give you everything, which I get in a way, I suppose, seeing what works for you and then take away what doesn't. (Carer 3, council H, Stage 2)
This carer felt that her mother had been given a ‘standard’ package of telecare that had not been personalised to address her specific needs and, because of this, telecare had caused more problems than it solved. The provision of standardised and over-prescribed telecare packages was also reported by some telecare managers who felt that this sometimes increased carer stress and worry.
Involving carers and overcoming barriers
Both the online survey and interviews revealed frequent claims that an important reason for carers being unable to use telecare successfully was that carers lacked information and knowledge about telecare and its functions. In the survey, when asked how carers’ needs could be met, 49 participants said that information and training for carers was ‘most important’. Of the 25 interviewed telecare managers, 20 felt that there were problems with carers’ levels of knowledge about telecare and several said that they wanted to improve this situation:
We've got a training package on promoting telecare, and some of the training that is being delivered has been to carers groups and carers organisations. We are trying to support carers in using telecare which will support them to look after somebody. It's part of a general campaign really about raising awareness for social workers and service users and carers. (Telecare manager 5, council E, Stage 1)
Other plans included increasing carers’ involvement in different stages of telecare provision. One aim was to increase the numbers of telecare users and/or their carers who could carry out the adjustment and maintenance of telecare devices beyond replacing batteries. One council planned for users and/or carers to install their own telecare equipment:
At the moment, everything that we install, the engineers install. We need to be more competitive and we will be moving towards the option for self-installation. (Commissioner 1, council G, Stage 2)
Among those councils that provided or funded a response service, two telecare managers wanted to pass on responsibility to the family or other unpaid carers to free up resources:
I think in some cases, it should be the family and if they don't want to take it or they simply don't answer the phone, they know that that call is then going to be forced to us. I think we need to move back to having more family involvement with it. (Telecare manager 12, council L, Stage 1)
Discussion
The previous section focused on a thematic presentation of data in the varied contexts in which carers were involved in the provision of telecare to older people and the responsibilities they take on during the process. This section discusses these findings, drawing on Twigg and Atkin's (Reference Twigg and Atkin1994) typology and existing research.
Twigg and Atkin's typology offers a framework to explore carers and telecare beyond the different stages of telecare provision by local councils as it considers four possible approaches of understanding both formal providers’ as well as carers’ involvement and perspectives in the process which might be applied to telecare as well as hands-on care.
Carers as resources in the provision of telecare
This section discusses stages of carers’ involvement in the provision of telecare, in which carers seemed to be perceived and involved as ‘resources’ and are ‘taken-for-granted’ (Twigg and Atkin, Reference Twigg and Atkin1994: 12). According to Twigg and Atkin's framework, where carers are typologised as ‘resources’, the aim is to maximise outcomes for (older) service users whilst essentially ignoring the needs of carers.
Integration of carer needs and perspectives in the assessment process
Our findings show that particularly during the assessment stage of telecare provision, councils seemed commonly to perceive carers as sources of information. They asked about the environmental and social situation of the older person and whether some needs were met with the support of carers, but largely not about those carers’ situations. It was not clear if carers were actively involved in decisions about what devices should be provided, either at assessment or installation stages.
The importance of taking account of the needs and circumstances of carers to make telecare ‘work’ for an older person has been discussed widely. Sugarhood et al. (Reference Sugarhood, Wherton, Procter, Hinder and Greenhalgh2014) highlight the need to identify and address the complexity of the context in which telecare is provided so that older people can successfully adopt and use telecare. Others have also suggested that a failure to properly involve the prospective user, or their carers, in the assessment may lead to subsequent telecare abandonment (Gramstad et al., Reference Gramstad, Storli and Hamran2014; Miller et al., Reference Miller, Whitlatch and Lyons2016). The customisation of telecare to match technology to need precisely has also been widely discussed (Wey, Reference Wey and Marshall2004, Reference Wey and Woolham2006; Woolham, Reference Woolham2006; Godwin, Reference Godwin2012; Olsson et al., Reference Olsson, Engström, Skovdahl and Lampic2012; Greenhalgh et al., Reference Greenhalgh, Wherton, Sugarhood, Hinder, Procter and Stones2013; Gibson et al., Reference Gibson, Newton, Pritchard, Finch, Brittain and Robinson2016; Kerssens et al., Reference Kerssens, Sattler and Monteiro2014). The quality of the assessment will help determine the degree of ‘fit’ between need and telecare solution. Other research (Godwin, Reference Godwin2012; Federici and Borsci, Reference Federici and Borsci2016) has shown that telecare equipment is often rejected or abandoned when telecare does not meet individual needs of service users or carers.
Integration of carers in telecare ‘maintenance’
Carers were frequently asked to carry out minor repairs and basic maintenance, and were sometimes relied upon to inform the council when greater maintenance or repair work was needed. In some councils carers were solely responsible for the maintenance of stand-alone equipment. Although repairs are often a ‘one-off’ event, our findings resonate with other research showing that carers are frequently relied upon to undertake the continual, often unacknowledged, invisible ‘day-to-day’ maintenance work to enable older people to use telecare devices. Moser and Thygesen (Reference Moser, Thygesen, Barnes, Brannelly, Ward and Ward2015) also described the demands and highlighted the responsibilities that telecare places upon carers. These include ensuring devices are constantly charged and/or that batteries are replaced, switched on when needed and, in the case of GPS-based devices, that the older person carries the device with them if they leave their home. A final example of continual ‘maintenance work’ carried out by carers from this study was the refilling of automated medication dispensers, designed to dispense the correct medication at the correct time and remind the patient to take it. As Gibson et al. suggest:
Family carers played a key role in facilitating the integration of AT [assistive technology] into the usual routines of their relatives by undertaking much of the everyday work required to ensure their habitual use. (Gibson et al., Reference Gibson, Dickinson, Brittain and Robinson2015: 5)
These tasks require time and can add to carers’ worries that something could go wrong (Hamblin, Reference Hamblin2017).
Self-assembly or self-installation
Related to maintenance, increased self-assembly and installation by service users or carers were discussed by some councils as a future aim. This highlights a further potential increase of carers as ‘resources’ to augment but also to replace services currently provided by councils in England. This is consistent with other research: Milligan et al. (Reference Milligan, Roberts and Mort2011: 352) suggested that use of telecare might lead to ‘a downward cascade of care-work and responsibilities’, e.g. ‘from nurses to family carers or patients’.
Carers as telecare responders
Another aspect of telecare provision that involved carers was the response to technology-generated alerts, whether actively generated by an older person, through stand-alone equipment, or through monitored telecare where no council services were available. Where paid-for response services were available, these brought some relief for carers and, here, they can be defined as ‘co-workers’ rather than ‘resources’.
Carers as co-workers in the provision of telecare
This section discusses aspects of telecare provision in which carers were perceived as ‘co-workers’: defined by Twigg and Atkin (Reference Twigg and Atkin1994) as being where councils recognise the carer's situation and interests, and provide care services for the older person alongside those of the carer with the same objective of ensuring carer wellbeing.
Response services
As our findings show, most councils offered paid-for response services. However, even in those councils that had a 24/7 paid response service, carers might often be contacted first: paid staff would only be dispatched in these councils if the carer was unavailable.
Managing and reviewing telecare provision
Managing telecare provision was another stage in which councils seemed to perceive carers as co-workers. In this study, telecare managers and carers alike discussed carers’ involvement in making changes to telecare provided. Changes might occur when, for example, provision did not meet the older person's needs, if these had changed, or if equipment or services did not ‘work’ for the end user (or the carer). Though carers may perceive monitoring centres and response services as efficient and reliable (Jarrold and Yeandle, Reference Jarrold and Yeandle2009), there is often a need to adjust protocols in monitoring centres before telecare could be said to ‘work’ for some carers. Failure to have effective triage arrangements in place and to understand and share technology-derived information properly have been linked to carer stress and increased carer ‘burden’ (Alaszewski and Cappello, Reference Alaszewski and Cappello2006). Procter et al. (Reference Procter, Wherton, Greenhalgh, Sugarhood, Rouncefield and Hinder2016) recommend monitoring centre personnel should be more knowledgeable about the individual's needs and circumstances to inform their decisions about whether to contact a carer, another nominated responder or paid staff, if emergency services are not required. Better assessments for telecare, as previously discussed, but also improvements to reviews of telecare packages might help to decrease unnecessary involvement of carers at this stage, which might also help to minimise carer stress and anxiety.
As shown in the section above on barriers to telecare use, telecare managers in interviews and the survey each thought carers lacked knowledge and information about telecare. Other studies have also found that the amount and quality of information available via councils varies significantly. Gibson et al. (Reference Gibson, Newton, Pritchard, Finch, Brittain and Robinson2016), for example, estimate that only half of local councils provide sufficient information to support people with dementia and their carers using telecare, and argue for increased information to be made available to carers to support their involvement in the process. This would, on the one hand, increase their knowledge, but on the other hand it could put an onus on carers to acquire this knowledge and to take on more responsibility.
Carers as co-clients in the provision of telecare
There was little evidence from our study of carers being ‘co-clients’; the third model in Twigg and Atkin's typology, and one in which the wellbeing of the carer is at the centre of attention and carers are supported in their own right by formal services. Although councils now have a statutory duty to consider and assess carers’ needs in their own right since the Care Act 2014 (HM Government, 2014), there was little evidence that carers were offered a separate assessment as part of the telecare assessment process or in their own right. This is consistent with others’ findings which show that this lack of consideration extends beyond telecare to wider social care provision (Glendinning et al., Reference Glendinning, Mitchell and Brooks2015; Yeandle, Reference Yeandle2016; Woolham et al., 2018a).
Provision of telecare and superseded carers
The last model in Twigg and Atkin's typology is the ‘superseded’ carer. Here care-giving is overcome by enabling independence of the older person or by acknowledging that the carer cannot provide care, e.g. through their own frailty or because other responsibilities make caring impossible.
As the findings on telecare strategies show, telecare is provided by councils to give or to help maintain independence for older people and to support carers. One outcome from providing telecare described by telecare managers was that carers were enabled to remain in paid employment or to undertake other responsibilities, e.g. caring for children.
One example, recurrently stated, was of aforementioned automated medication dispensers, which could replace periodic checking to ensure medication was taken. However, although such devices made constant checking unnecessary, they created new and different responsibilities, because carers needed to ensure that the device was correctly refilled and set up. Medication dispensers therefore did not entirely ‘supersede’ the carer, but did potentially free up time for them to carry out other responsibilities. Additionally, though automated dispensers might free up carer time, reduced contact – where medication taking is technology assisted – might also carry a risk of older people developing ‘new’ needs if this leads to greater isolation and loneliness (Steptoe et al., Reference Steptoe, Shankar, Demakakos and Wardle2013).
Limitations
One weakness of the study is the small number of family or unpaid carers involved in the case studies. This makes wider comparison of perspectives of local council telecare managers and experiences of carers unattainable. However, the three involved carers provided an alternative perspective to the perceptions of telecare managers.
Carer involvement in our paper is predominantly discussed from the perspectives of telecare managers and practitioners in council or council-commissioned services: future research could focus on carers directly. However, it is also worth noting that the ‘proxy’ perspective offered by managers will have real impacts on telecare recipients and their carers.
A further limitation is that all interviewees and survey respondents were nominated or selected by participating councils, and other views and experiences within the local and national context might be lost to this research. However, we do not think it would have been feasible for our study to recruit participants without council support.
Conclusion
This paper aimed to develop knowledge of the nature and extent of family or other unpaid carers’ involvement and the impact of telecare provision for older people on carers, and how their involvement is perceived within English local councils by applying Twigg and Atkin's (Reference Twigg and Atkin1994) typology of carer support. We argue that carers are largely perceived as ‘resources’ and taken for granted when councils provide telecare to older people. There are instances in which carers are ‘co-workers’ but this is mainly around responding to monitored telecare and attached services and not the case in all councils. Carers’ position and status as ‘co-workers’ could be improved in practice by consistently involving carers in assessments of the older person (providing the older person assents to this). The carer's perspective will add and inform as to how needs and abilities of the cared-for person are perceived by the local council and potentially assisted by telecare. The way telecare is used in some councils creates the conditions for some carer roles to be superseded with telecare both by maximising the older person's independence and/or replacing hands-on care services through telecare. However, some councils also have strategies in place that will potentially result in an increase in carer responsibilities in the future.
Carers’ own rights as ‘co-clients’ (recognised in the Care Act 2014) for their own needs to be assessed and to be given support often seemed overlooked. Our study also suggests that some councils may need to increase the amount and quality of information they provide about telecare so carers can have informed choice about their own role in telecare provision.
Our findings are consistent with previous research that suggests that telecare can support carers in their role, e.g. enabling them to have respite from caring or to engage in other activities, and, in some cases, remain in employment. It also confirms others’ findings that carers are often essential for telecare to work for older people; whether by ensuring equipment is functioning correctly or responding to alerts. In addition, when telecare does not meet the needs and goals of the older person, carers initiate changes to equipment or services, or request the removal of telecare.
Acknowledgements
The authors wish to offer grateful thanks to all research participants. They would also like to thank Jill Manthorpe for her constructive and supportive comments on earlier drafts of this article. Any mistakes or omissions are the responsibility of the authors only.
Author contributions
NS prepared each draft of this manuscript. Other authors contributed by suggesting amendments and changes. All authors were involved in the conception and design of the study, data collection, and analysis and interpretation of data.
Financial support
This work was supported by the English National Institute for Health Research/School for Social Care Research (grant number C088/T15-011/KCLJW-p89). The views expressed in this publication are those of the authors and not necessarily those of the funder, the Department of Health and Social Care or the UK National Health Service.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
The study received a favourable ethical opinion from the Health Research Authority Research Ethics Committee (HRA reference 16/NI/0051). It was also supported by the Association of Directors of Adult Social Care Services (ADASS).







