Book contents
- Personality Disorder
- Personality Disorder
- Copyright page
- Dedication
- Contents
- Foreword
- Acknowledgements
- Chapter 1 History of Personality and Its Disorders
- Chapter 2 Assessment of Personality
- Chapter 3 Personality Difficulty
- Chapter 4 Borderline Personality Disorder
- Chapter 5 Cultural Perspectives
- Chapter 6 Personality and Health
- Chapter 7 Personality Disorders and Comorbidity with Other Mental Illness
- Chapter 8 Treatment and Outcome of Personality Disorder
- Chapter 9 Moderating the Stigma of Personality Disorder
- Chapter 10 What Needs to Be Done Now
- Appendices
- References
- Index
- References
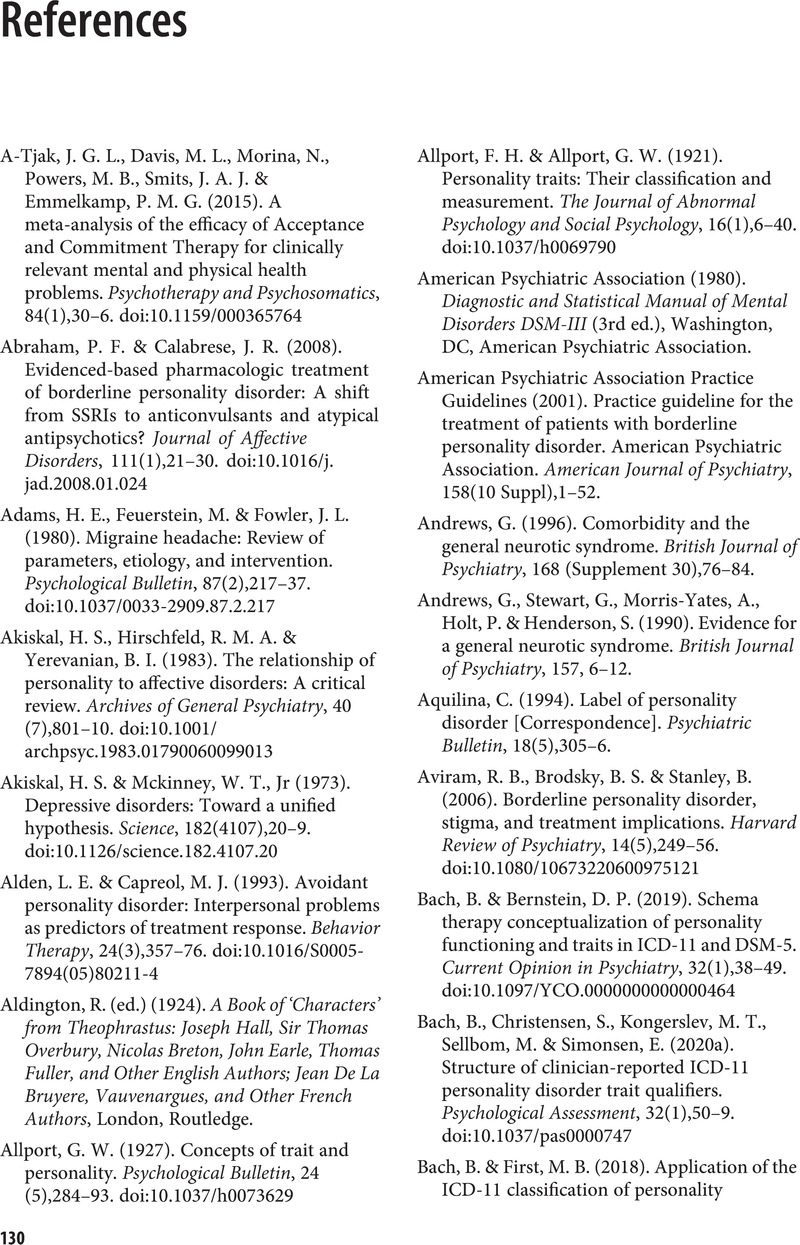
References
Published online by Cambridge University Press: 04 February 2022
- Personality Disorder
- Personality Disorder
- Copyright page
- Dedication
- Contents
- Foreword
- Acknowledgements
- Chapter 1 History of Personality and Its Disorders
- Chapter 2 Assessment of Personality
- Chapter 3 Personality Difficulty
- Chapter 4 Borderline Personality Disorder
- Chapter 5 Cultural Perspectives
- Chapter 6 Personality and Health
- Chapter 7 Personality Disorders and Comorbidity with Other Mental Illness
- Chapter 8 Treatment and Outcome of Personality Disorder
- Chapter 9 Moderating the Stigma of Personality Disorder
- Chapter 10 What Needs to Be Done Now
- Appendices
- References
- Index
- References
Summary
- Type
- Chapter
- Information
- Personality DisorderFrom Evidence to Understanding, pp. 130 - 156Publisher: Cambridge University PressPrint publication year: 2022