Introduction
Arterial hypertension (AH) is the most important risk factor for stroke and occurs approximately in 70% of ischemic stroke (IS) patients Reference Go, Mozaffarian and Roger1 and most IS patients have elevated blood pressure (BP) at stroke onset. Reference Mustanoja, Putaala and Gordin2 Current evidence shows a strong positive association between a reduction of BP and risk of recurrent IS (RIS). 3–Reference Liu, Wang and Gong5
The incidence of IS among young adults increases as reported recent studies Reference Rosengren, Giang and Lappas6–Reference George, Tong and Bowman8 and represents approximately 20% of all IS. Reference Putaala9–Reference Putaala, Metso and Metso13 A cause of IS in young patients remains often unclear or differ from elderly patients, Reference Putaala, Metso and Metso13–Reference Wolf, Grittner and Böttcher15 but one-third of them may be affected by a recurrent vascular event. Reference Pezzini, Grassi and Lodigiani16–Reference Rutten-Jacobs, Arntz and Maaijwee18 Furthermore, traditional vascular risk factors (VRFs) including AH becoming more prevalent in young IS patients during the last years, especially in those with unhealthy life style. Reference Putaala, Yesilot and Waje-Andreassen14,Reference Andersson and Vasan19 This corresponds to the more than twice increased prevalence of AH in the common young adult population during the last 20 years. Reference Yano, Stamler and Garside20
Data about AH in young IS patients and about antihypertensive treatment in secondary prevention are limited, since few of them were enrolled in clinical trials or studies. A recent retrospective registry-based study showed that young IS patients, users of antihypertensives, had a lower risk of RIS and mortality compared to the non-users. Reference van Dongen, Aarnio and Martinez-Majander21 Another study showed that higher admission systolic and diastolic BP were independently associated with the risk of RIS, while 24-hour BP levels were not. Reference Mustanoja, Putaala and Gordin2
We aimed to assess prospectively the incidence of AH in young IS patients and evaluate the impact of BP compensation after patients’ discharge on the risk of RIS using outpatient BP Holter. Furthermore, we aimed to analyze possible associations among the presence of AH and poor BP compensation after discharge and presence of other risk factors and conditions.
Subjects and Methods
We analyzed consecutive young IS patients <50 years of age, who were enrolled in the prospective single-center observational Heart and Ischemic STrOke Relationship studY (HISTORY) registered on ClinicalTrials.gov (identifier NCT01541163) between years 2011 and 2019. Reference Kral, Skoloudik and Sanak22 The study protocol was published in detail previously, Reference Kral, Skoloudik and Sanak22 and thus, we present here a part, which was essential for this study.
All enrolled patients underwent an identical diagnostic protocol, which involved computed tomography (CT) or magnetic resonance imaging (MRI) including CT or MRI angiography, ultrasound of cervical and cerebral arteries, transoesophageal echocardiography (TEE) with the use of contrast agent for a bubble test, ultrasound of veins of both upper and lower limbs in patients with the TEE finding of right–left shunt to exclude present or previous deep vein thrombosis. Reference Powers, Rabinstein and Ackerson23 In all patients without presence of AF at the admission or during a hospital stay at stroke unit, a 24-hour electrocardiogram (ECG) Holter and 3- or 4-week ECG Holter monitoring were performed.
A 3-month clinical outcome was assessed by an experienced certified neurologist and using the modified Rankin Scale with a score of 0–2 for a good outcome. All patients used antiplatelets or anticoagulants in the secondary prevention according to the stroke etiology. Most enrolled patients were followed through a clinical or phone controls at least once a year in the follow-up (FUP).
Causes of strokes were classified and graded according to the ASCOD classification. Reference Amarenco, Bogousslavsky and Caplan24 All patients with the ASCOD score other than “grade 1” (potentially causal) were classified as cryptogenic. Reference Amarenco, Bogousslavsky and Caplan24
AH was defined according to the World Health Organization criteria. Reference Whitworth25 All patients had admission BP measurement (emergency room) followed with regular measurements performed each hour during the stay at stroke intensive care unit (at least the first 24 hours). BP measurements continued in a regimen of regular three measurements per day during the remaining hospital stay. All BP measurements were performed by a fully automatic arm BP monitors in the laying patient.
Outpatient BP Holter (Spacelabs™ model 90217A) was performed 1 month after the discharge in consecutive young IS patients between the years 2017 and 2019. The evaluation and interpretation of recorded levels of BP were done by a blinded experienced and certified cardiologist in the Center for Hypertension affiliated to Department of Cardiology in our hospital.
The study protocol was in a compliance with the Declaration of Helsinki (1975) and was approved by the Ethical Committee of our hospital. All patients gave an informed consent to participate in the study.
Statistical analysis SPSS software (version 22.0; SPSS, Chicago, Illinois) was used for the statistical analysis. Normality of distribution was checked using the Shapiro–Wilk test. All parameters with non-normal distributions are presented as means ± SD, medians, and interquartile ranges. The Mann–Whitney test was used for non-parametric values, and the chi-square test and Fisher’s exact test were used for parametric values. Univariable and multivariable logistic regression analyses (LRA) were used to evaluate analyzed demographic, baseline and clinical parameters, and VRFs as possible predictors of RIS in patients with AH. Multivariate regression stepwise model was adjusted for potential confounders. All tests used an α-level of 0.05 for significance.
Results
We enrolled 319 young IS patients <50 years of age (179 males, mean age 41.1 ± 7.8 years) in the prospective HISTORY between years 2011 and 2019 and 229 (71.8%) of them were classified as cryptogenic according to ASCOD. Patients’ demographic, baseline, and clinical characteristics are shown in Table 1. AH was present in 120 (37.6%) of IS patients and 75 (62.5%) of them used antihypertensives.
Table 1: Comparison of demographic, baseline clinical characteristics and outcomes between patients with and without AH
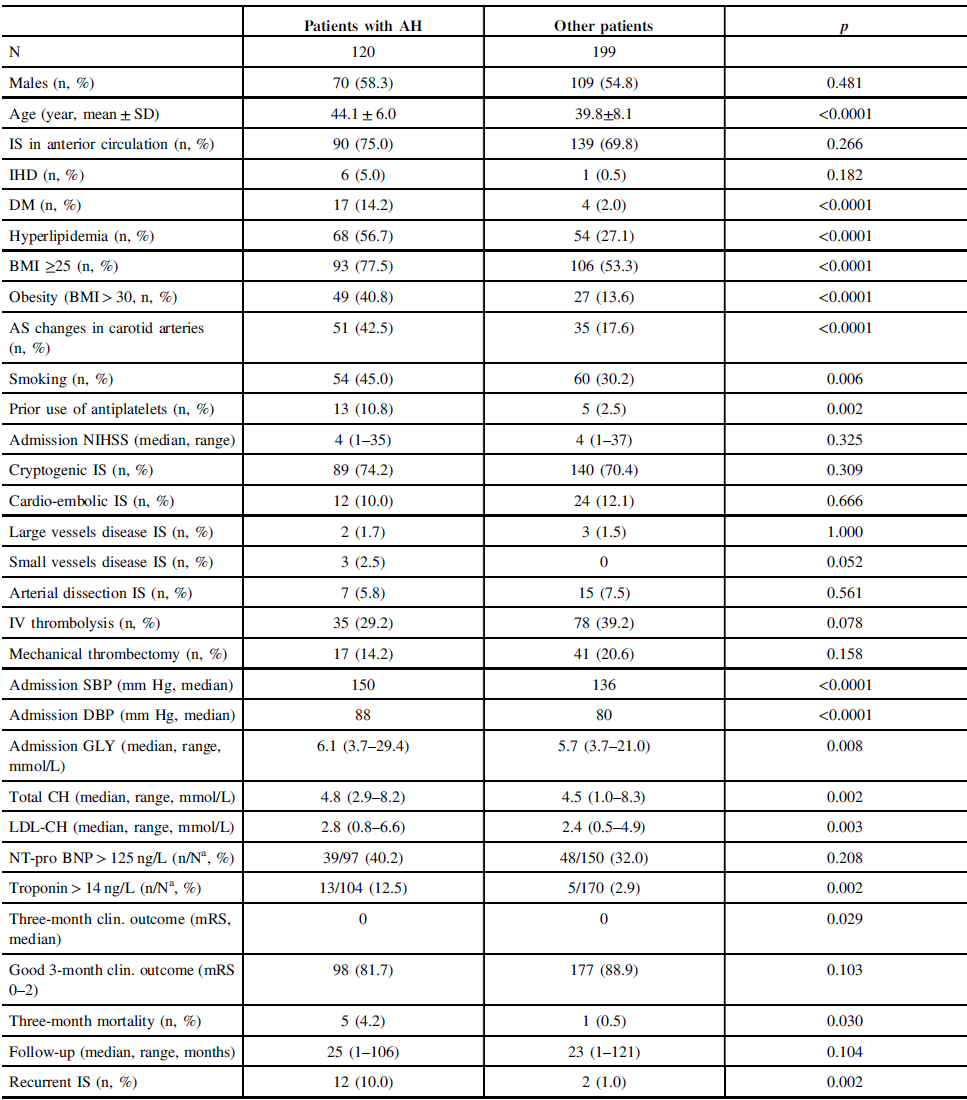
AH = arterial hypertension; AS = atherosclerotic; BMI = body mass index; CH = cholesterol; DBP = diastolic blood pressure; DM = diabetes mellitus; GLY = glycemia; IHD = ischemic heart disease; IS = ischemic stroke; IV = intravenous; mRS = modified Rankin Scale; NIHSS = National Institute of Health Stroke Scale; SBP = systolic blood pressure.
Patients with AH had more frequently RIS during the FUP with a median of 25 months (10 vs. 1%, p = 0.002) (Table 1), were older (44.1 ± 6.0 vs. 39.8 ± 8.1 years, p < 0.0001), had more frequently diabetes mellitus (14.2 vs. 2.0%, p < 0.0001), hyperlipidemia (56.7 vs. 27.1%, p < 0.0001), atherosclerotic (AS) changes in carotid arteries (42.5 vs. 17.6%, p < 0.0001), more frequently smoked (45.0 vs. 30.2%, p = 0.006), and used more frequently antiplatelets prior IS (10.8 vs. 2.5%, p = 0.002) (Table 1). Patients with AH had also higher admission systolic and diastolic BP, higher admission glycemia, total and LDL cholesterol, and had more frequently elevated serum troponin T at admission (Table 1). More patients with AH died within the first 3 months after IS (4.2 vs. 0.5%, p = 0.030) (Table 1). Number of patients with cryptogenic stroke did not differ between patients with and without AH, as well as the other etiological stroke subtypes (Table 1).
Patients with AH and RIS were older (47.3 ± 3.4 vs. 43.6 ± 5.9 years, p = 0.005), more frequently used antiplatelets prior IS (33.3 vs. 8.3%, p = 0.026), had higher admission glycemia (6.8 vs. 6.0 mmol/L, p = 0.022), and had more frequently the etiological stroke subtype “large vessels disease” according to ASCOD classification (16.7 vs. 0%, p = 0.009) (Table 2).
Table 2: Comparison of demographic, baseline clinical characteristics and outcomes between patients with AH and RIS and without RIS
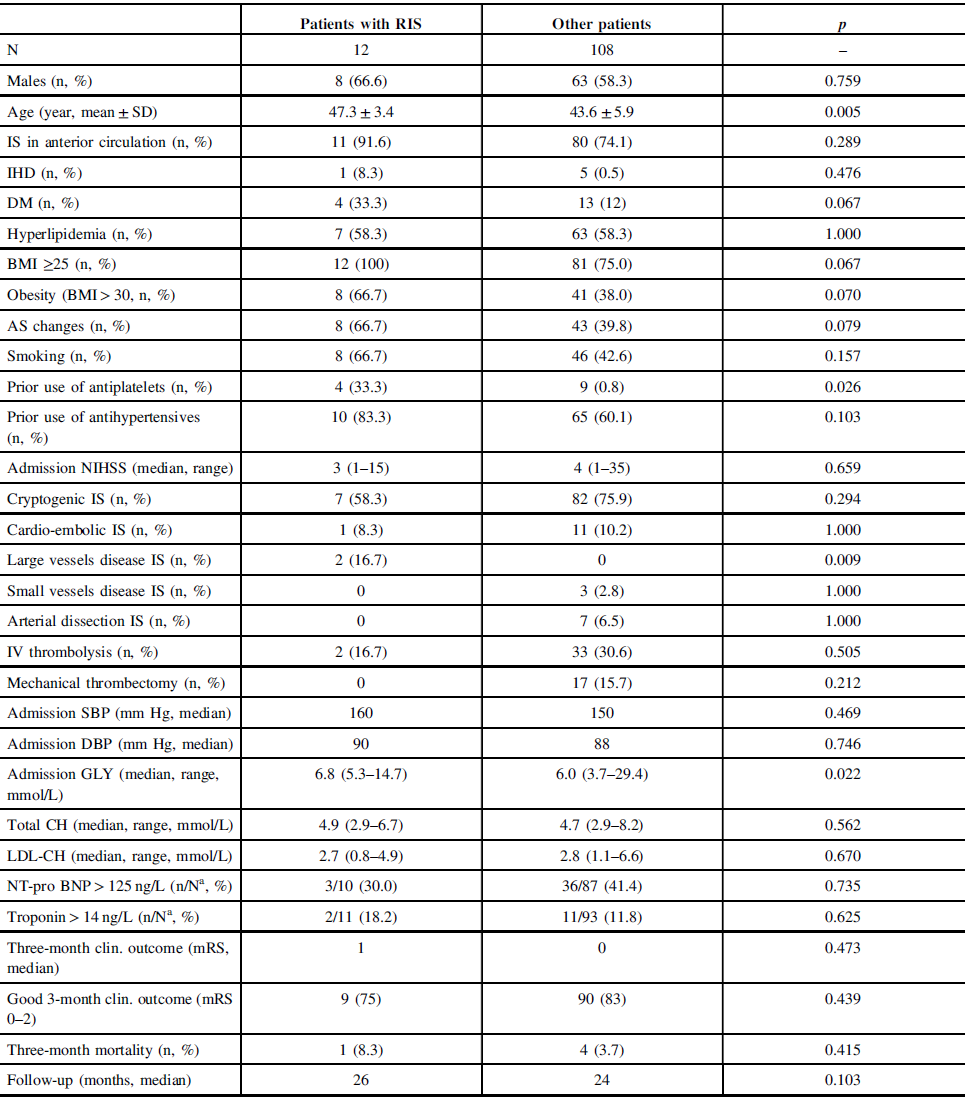
AH = arterial hypertension; AS = atherosclerotic; BMI = body mass index; DBP = diastolic blood pressure; DM = diabetes mellitus; GLY = glycemia; IHD = ischemic heart disease; CH = cholesterol; IS = ischemic stroke; IV = intravenous; mRS = modified Rankin Scale; NIHSS = National Institute of Health Stroke Scale; RIS = recurrent ischemic stroke; SBP = systolic blood pressure.
Univariate LRA showed age and prior use of antiplatelets as predictors of RIS in patients with AH (Table 3) and multivariate stepwise model showed the prior use of antiplatelets as only predictor of RIS (p = 0.011, OR: 6.125; 95% CI: 1.510–24.837).
Table 3: Univariate logistic regression analysis for identification of independent predictors of recurrent ischemic stroke; subgroup analysis of patients with AH

AH = arterial hypertension; AS = atherosclerotic; BMI = body mass index; DBP = diastolic blood pressure; DM = diabetes mellitus; IHD ischemic heart disease; IS = ischemic stroke; IV = intravenous; mRS = modified Rankin Scale; SBP systolic blood pressure.
Outpatient BP Holter 1 month after discharge was performed in 84 consecutive patients (39 males, mean age 42.8 ± 6.0 years) and elevated BP levels were detected in 26 (31.0%) of them (Table 4). Patients with abnormal BP levels after discharge on BP Holter were more frequently males, had more frequently AH (53.8 vs. 31.0%, p = 0.047) and higher admission diastolic BP, and had more frequently AS plaques in carotid arteries (50.0 vs. 24.1%, p = 0.019). The number of RIS did not differ between both subgroups (3.8 vs. 1.7%, p = 1.000) during FUP (Table 4).
Table 4: Comparison of demographic, baseline clinical characteristics and outcomes between patients with elevated blood pressure on BP Holter and with normal levels
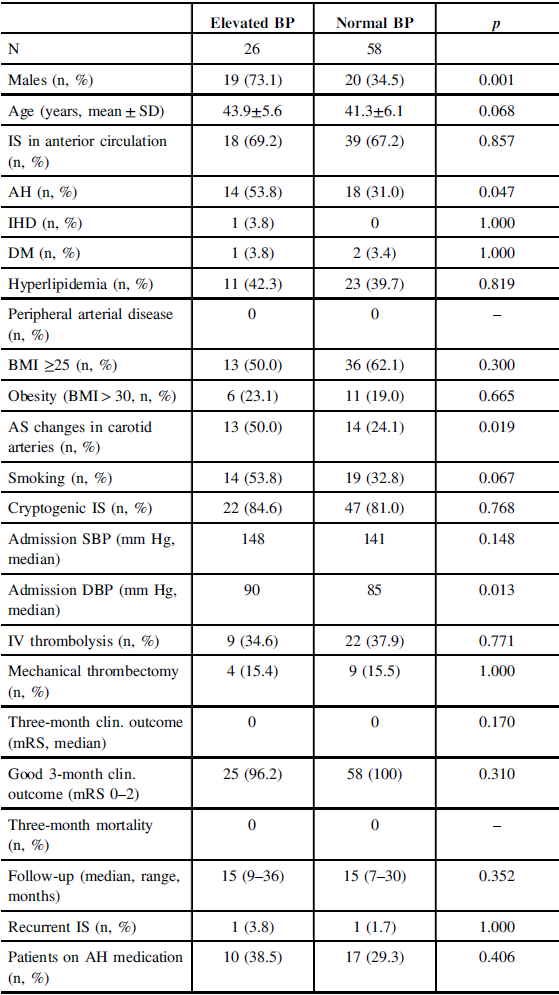
AH = arterial hypertension; AS = atherosclerotic; BMI = body mass index; BP, blood pressure; DBP = diastolic blood pressure; DM = diabetes mellitus; IHD = ischemic heart disease; IS = ischemic stroke; IV = intravenous; mRS = modified Rankin scale; SBP = systolic blood pressure.
Discussion
AH was present in 37.6% of young IS patients < 50 years of age in our study and this finding corresponds to previous report of presence of AH in 39.2% of young IS patients from the Helsinki Registry. Reference Mustanoja, Putaala and Gordin2 In our study, patients with AH had significantly more RIS during the FUP than those without AH (Table 1). The multicenter INTERSTROKE case-control study showed stronger association between AH and stroke in younger patients (< 45 years) than older (≥45 years). Reference O’Donnell, Xavier and Liu26
In our study, patients with AH were older and have more VRFs including the presence of AS changes in carotid arteries and higher level of cholesterol than those without AH (Table 1). These findings may explain the higher frequency of RIS in young IS patients with AH and support the concept of “risk profile” in young IS patients, in whom the prevention is strongly needed. Accumulation of VRF with increasing age among young IS patients was associated with increased risk of atherothrombotic event in future Reference Putaala, Haapaniemi and Kaste27 and more of VRF risk were associated with IS in those who were aged 40 to 49 years compared to those who were under 40 years. Reference Kivioja, Pietilä and Martinez-Majander28 Recent German nationwide case-control study in young IS patients showed that AH had the second highest adjusted population-attributable risk for IS among VRF. Reference Aigner, Grittner and Rolfs29 Furthermore, pooled data from 15 hospital-based registries of young IS patients (15–49 years) showed increasing frequency of large vessels AS and small vessels disease with age and higher prevalence of these causes in men. Reference Yesilot Barlas, Putaala and Waje-Andreassen30
In our study, patients with AH and RIS were older, more frequently used antiplatelets prior IS, and had higher admission glycemia in comparison with patients without RIS (Table 2). Age and prior use of antiplatelets were found only predictors of RIS in young IS patients with AH in our study in univariate LRA model (Table 3) and multivariate stepwise LRA model showed only the prior use of antiplatelets as predictor of RIS. These findings also support the concept of “risk profile” in young IS patients, who were treated with antiplatelets prior IS for the presence of VRF.
Most (74.2%) of our patients with AH had cryptogenic etiology of IS according to the ASCOD classification and the second most frequent (10%) cause was cardio-embolism (Table 1). Patients with AH and RIS had the large vessels disease (16.7%) as the second most frequent cause (after cryptogenic etiology) (Table 2), which was more frequent in comparison with the patients without RIS (0%) (Table 2). Higher frequency of large vessels disease as a cause of stroke in the young patients with AH, who suffered from RIS, may indicate the significant role of atherosclerosis and VRFs in stroke recurrence in these patients.
Elevated levels of BP on outpatient BP Holter 1 month after discharge were present in 31% of our patients (Table 4). Patients with abnormal outpatient BP Holter were older, had more frequently AH and AS changes in carotid arteries, but they had similar rate of RIS during the FUP as those with normal levels (Table 4). A recent report showed suboptimal use of antihypertensive medication in one-third of all young users after IS. Furthermore, young users of antihypertensive medication had lower risk of RIS and mortality compared to non-users after IS. Reference van Dongen, Aarnio and Martinez-Majander21
In our study, 62.5% of patients with AH used antihypertensives prior IS. This rate corresponds to 59.6% of AH users – young IS patients enrolled in the Helsinki Young Stroke Registry. Reference van Dongen, Aarnio and Martinez-Majander21 The data from this registry showed a higher proportion of antihypertensive use and better usage in patients with higher age. Furthermore, the higher frequency of use of antihypertensives was associated with presence of VRF. Reference van Dongen, Aarnio and Martinez-Majander21
Our study has limitations. Single-center design was used in our study and was based on the protocol of the prospective HISTORY. Reference Kral, Skoloudik and Sanak22 A very low number of patients, who underwent the outpatient BP Holter 1 month after discharge, was analyzed and thus, the results of the comparison between the patients with normal and elevated levels of BP were very limited. We did not analyze clinically asymptomatic RIS detected on MRI because not all patients underwent control MRI during the FUP.
In conclusion, AH was frequent in young IS patients and its presence increased the risk of RIS in them, especially in those with presence of other VRF. Abnormal levels of BP on outpatient BP Holter after discharge did not increase the risk of RIS. Despite frequent unknown cause of IS in young patients, targeted prevention in those with AH and other VRF may reduce the IS recurrence.
Acknowledgments
This work was supported by the AZV – Health Research Council, Ministry of Health of Czech Republic under grant n. 17-30101A, and by the Internal Grant Agency Palacký University Medical school under grant n. IGA LF UP_006_2020.
Conflict of Interest
All authors have no conflict of interest.
Statement of Authorship
PD and DS: study concept and design, acquisition of data, analysis and interpretation of data; drafting and critical revision of the manuscript for important intellectual content; and final approval of the version to be published. JV and MH: acquisition of data, responsibility for cardiologic part of study, and analysis and interpretation of BP values. JZ: statistical analysis and interpretation of analysis. MK, AB, DF, TD, and TV: acquisition of data and critical revision of the manuscript for important intellectual content. MT and PK: critical revision of the manuscript for important intellectual content.






