Key Point Box
-
∙ Depression is increased in unprovoked first seizure patients at first presentation compared with control population.
-
∙ The prevalence of depression increased with a longer duration of undiagnosed epilepsy at the time of first clinical assessment.
Seizures can be considered a result of a complex process in the brain resulting from an imbalance of metabolic and biological variables. Population studies show that 25% to 30% of first seizures are acutely provoked by disturbances in brain chemistry caused by direct insult to the brain or metabolic disturbances.Reference Annegers, Hauser, Lee and Rocca 1 , Reference Pohlmann-Eden, Beghi, Camfield and Camfield 2 Seizures that do not result directly from acute systemic, metabolic, or toxic cerebral insult are considered unprovoked.Reference Pohlmann-Eden 3 For unprovoked seizures, the individually contributing risk factors for ictogenesis are still poorly understood and difficult to disentangle, particularly when structural and functional abnormalities and hereditary background are missing. More recently, psychiatric conditions such as depression and anxiety have been discussed as either potential risk factors or indicators for subsequent seizure occurrence.Reference Hesdorffer, Hauser, Olafsson, Ludvigsson and Kjartansson 4 In people with epilepsy through all stages of the disease, there are high comorbidity rates of depression and anxiety, with a wide range reported at between 20% and 80%.Reference Tellez-Zenteno, Patten, Jetté, Williams and Wiebe 5 Interpretation is still challenging because multidimensional factors are likely playing a role in psychiatric manifestation in epilepsy such as: seizure etiology, location electroencephalogram (EEG) focus, duration of epilepsy, medication side effects, socioeconomic sequels, and stigmatization.Reference Pohlmann-Eden, Beghi, Camfield and Camfield 2 Others have suggested that these comorbid conditions in seizures are best explained by an imbalance in the neurochemical milieu and/or common or shared mechanism using similar neuroanatomical structures.Reference Kanner 6 The exact nature of the relationship between epilepsy and psychiatric mood disorders is still not well understood.Reference Adelow, Andersson, Ahlbom and Tomson 7
The objective of our study was to define the prevalence of psychiatric symptoms of anxiety and depression in patients at the time of their first clinical presentation for seizure diagnosis.
METHODS
Study Population
All patients referred to the Halifax First Seizure Clinic (HFSC) at the Queen Elizabeth II Health Sciences Centre between 2014 and 2016 were eligible for the study. A total of 57 patients and 31 controls were recruited to participate. Inclusion criteria were any participants referred to the HFSC for examination of possible first episode of seizure and older than 18 years. Exclusion criteria included all subjects with a lower than grade 7 education, known significant cognitive dysfunction or psychomotor delay, progressive neurological disease, provoked seizure, psychogenic nonepileptic seizure, evidence for already established seizure or epilepsy diagnosis in their medical history, or presence of prior psychiatric comorbidity. Control participants were recruited from nonblood relatives or partners of patients who were present at the appointment (Figure 1). The Research Ethics Board at the Nova Scotia Health Authority approved this study.

Figure 1 Flow chart of study population recruitment and categorization.
Measures of Anxiety and Depression
At the time of the referred patients’ initial visit to the HFSC, all potential participants were immediately informed of the nature of study before even having seen the specialist (MD, epileptologist) or the epilepsy nurse practitioner (NP). With this algorithm, we avoided the potential bias of the anxiety of an extensive assessment and counselling and potentially a diagnosis of epilepsy by the MD or NP on a patient’s test performance. Patients were asked to provide consent to participate, and afterwards completed the following tests under supervision of the research assistant:
-
1. Neurological Disorders Depression Inventory for Epilepsy (NDDI-E): This self-report screening tool uses six-item scale for identification of major depression in epilepsy. Scores >15 are considered positive for major depressive episode, with specificity of 90% and sensitivity of 81% with a positive predictive value of 0.62.Reference Micoulaud-Franchi, Lagarde and Barkate 8
-
2. Generalized Anxiety Disorder 7-Item (GAD-7) scale: This is a self-report seven-item anxiety scale instrument for identification of generalized anxiety disorder. Scores >14 are considered positive for severe anxiety. This tool has a specificity of 92% and sensitivity 56% with a positive likelihood ratio of 7.2.Reference Spitzer, Kroenke, Williams and Löwe 9
Subsequently, all patients were then seen by an MD and NP for full comprehensive assessment, neurology examinmation, diagnosis, counselling, and defining further diagnostic steps and treatment decisions. Despite being referred to the HFSC for a first seizure, following the comprehensive assessment, some participants were found to have a history of undiagnosed seizures before the index seizure that resulted in their referral. Those found to have a history of seizures for less than 12 months were defined to have new-onset epilepsy (NOE) and those with seizures dating back beyond 12 months were categorized as newly diagnosed epilepsy (NDE).Reference Pohlmann-Eden, Legg and Crocker 10 Magnetic resonance imaging and routine and sleep-deprived EEG were completed as part of the comprehensive diagnostic workup. Magnetic resonance imaging findings in this study are reported with regard to their topographical distribution. Patient and diagnostic variables were obtained following the appointment through medical chart review (age, gender, level of education).
Statistical Analysis
Statistical analysis was performed using SPSS statistical software, version 23 (IBM Corp.). Participants with scores of ≥15 for NDDI-E and ≥14 for GAD-7 were dichotomized as presence or absence of depression and anxiety. Chi-square odds ratios (ORs) were calculated for control versus unprovoked seizure patient for both anxiety and depression. All statistical tests were significant at the 95% confidence interval (CI).
RESULTS
Demographic Comparisons
Our study included 57 unprovoked first seizure subjects and 31 age-matched healthy controls. Level of education did not significantly differ between control participants compared with seizure patients. There were more males in the patient population, but this distribution difference did not rise to the level of statistical significance (Table 1).
Table 1 Sociodemographic information for study population
Results of Screening Instruments
In our healthy control population, 6.5% screened positive for depression (NDDI-E >15), whereas 33% of our unprovoked first seizure participants screened positive (p=0.01). Performance on the GAD-7 did not differ significantly between groups; 9.7% of controls had severe anxiety compared with 23% of unprovoked first seizure patients (p=0.14, Figure 2). The Pearson-Chi test among unprovoked first seizure patients was significant for depression (p=0.005), but not for anxiety (p=0.43, Figure 2).
Subcategorization of the unprovoked first seizure participants was then conducted as first seizure (unprovoked single seizure, n=15), NOE (seizures occur within 12 months, n=24), and NDE (seizures occur longer than 12 months, n=18; Figure 1)Reference Pohlmann-Eden, Legg and Crocker 10 Further Pearson-Chi testing showed first seizure had 13.3% screen positive for depression with an OR of 2.23 compared with control; this did not reach statistical significance (OR, 2.2; 95% CI, 0.28-17.6). Positive screening for depression in participants with NOE was 37.5% of the sample (OR, 11.6; 95% CI, 2.1-64) and an even greater number of those with NDE were seen at 44.4% (OR, 20; 95% CI, 2.2-181).
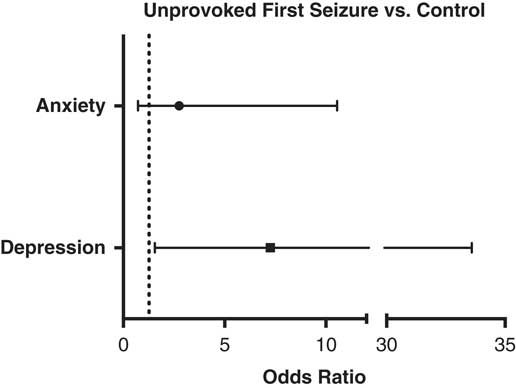
Figure 2 Forest plot comparing the presence of anxiety and depression in unprovoked first seizure patients versus control population.
The vast majority of patients presented with generalized tonic-clonic seizures when presenting to HFSC (n=52). Seizures were further classified into focal if there was evidence for clinical focal onset, dyscognitive seizures, preceding auras, or EEG findings suggestive of focal findings. All others were classified as generalized seizures. Unprovoked first seizure patients were dichotomized as either presence or absence of anxiety or depression as described by the screening questionnaire cutoffs. The results are summarized in Tables 2 and 3. Unprovoked first seizure patients with comorbid depression were found to have no differences in focal onset, frequency, EEG findings, number of medications, alcohol, tobacco, or marijuana use compared with those without psychiatric comorbidities. Similarly, unprovoked first seizure patients with comorbid anxiety were found to have no difference in focal onset, frequency, EEG findings, number of medications, alcohol, tobacco, or marijuana use compared with those without psychiatric comorbidities. Magnetic resonance imaging results were normal in two-thirds of all patients (Tables 2 and 3); pathological findings were overall subtle and ranged from remote discrete vascular lesions to nonspecific scars or showed global diffuse changes. No gross lesions such as tumors or large infarcts were identified. Temporal abnormalities were significantly more present in both the patients with comorbid anxiety (38.5%) and the patients with comorbid depression (26.5%) compared with patients with no psychiatric comorbidities (0.0%), which showed no abnormalities in this region (Tables 2 and 3).
Table 2 Comparison of demographic and diagnostic information for unprovoked seizure patients with and without depression
Bold text indicates significant difference with Fisher’s Exact Test.
* Indicates significant difference with Chi-Square Test.
Table 3 Comparison of demographic and diagnostic information for unprovoked seizure patients with anxiety and without anxiety
DISCUSSION
First seizure presentations represent a significant challenge for practitioners to individually evaluate the risk of a seizure recurrence and provide optimal counseling. This patient group provides an unique opportunity to learn more about subtle mechanisms of disease evolution by analyzing group patterns.Reference Pohlmann-Eden 3 Our study is an innovative approach that focuses on psychiatric comorbidities as potential risk factors or indicators for seizure recurrence among well-established, known prognostic factors such as etiology and abnormal EEG. Although previous studies have attempted to retrospectively analyze this population for prevalence of anxiety and depression, our study evaluated patients for these items at their first presentation to help understand a potential underlying directional relationship.Reference Hesdorffer, Hauser, Olafsson, Ludvigsson and Kjartansson 4 , Reference Tellez-Zenteno, Patten, Jetté, Williams and Wiebe 5 Here, we used screening questionnaires as a tool in clinical practice to quantify subjective variables.Reference Spitzer, Kroenke, Williams and Löwe 9 In particular, the NDDI-E and GAD-7 are two validated self-reported screening questionnaires with high sensitivity and specificity for depression and anxiety, respectively.Reference Micoulaud-Franchi, Lagarde and Barkate 8 , Reference Gilliam and Albertson 11 - Reference Cole 13 We attempted to control the effect of hospital environment on anxiety and depression by recruiting our control population from the nonblood relative or partner of patients at the time of visit. Our study protocol also required that all patients were screened for psychiatric comorbidities before they entered the doctor’s office and received any potentially concerning medical information.
In our unprovoked first seizure patients, screening with the NDDI-E indicated depression had a prevalence of 33.0% similar to other reports on patient populations with epilepsy and a comorbid diagnosis of depression, but this rate is higher than the reported prevalence based on survey studies and studies on implantable cardioverter-defibrillator population databases.Reference Tellez-Zenteno, Patten, Jetté, Williams and Wiebe 5 , Reference Wiegartz, Seidenberg, Woodard, Gidal and Hermann 14 , Reference Fiest, Dykeman and Patten 15 Retrospective studies on prevalence of previous depression before first seizure onset report lower prevalence of 12.0% and 3.9%.Reference Hesdorffer, Hauser, Olafsson, Ludvigsson and Kjartansson 4 , Reference Tellez-Zenteno, Patten, Jetté, Williams and Wiebe 5 One explanation for this discrepancy is possible coding errors and incomplete data collection through retrospective chart review compared with personal screening. Alternatively, the GAD-7 and NDDI-E have a false-positive rate of 10% and 8%, respectively, which may account for some variation in our study population. In terms of control participants, we found a prevalence of control population that indicated prevalence of depression of 6%, similar to the Canadian Community Health survey that reported a yearly prevalence rate of major depressive episode of 4.8% in the adult general population.Reference Meng and D’Arcy 16
Anxiety screening was positive for 23% of unprovoked first seizure patients and 9.7% of control participants, which was not significantly different between the groups. In comparison, Brandt et al found that in a population of long-term refractory focal epilepsy, 19.2% of the patients had an anxiety disorder, whereas the 2012 Canadian Community Health Survey quotes a yearly general population prevalence rate of 4.8%.Reference Meng and D’Arcy 16 , Reference Brandt, Schoendienst and Trentowska 17 It is also possible that the hospital environment or the associated uncertainty around the appointment outcome resulted in increased anxiety for both groups. Additionally, there may be a bias toward less anxious patients in the patient sample; it could that the most anxious patients did not attend their appointments, as is known to occur in treatment-resistant epilepsy.Reference Hamilton, Anderson and Dahodwala 18
Subcategorizing patients with the diagnosis of first seizure, NOE, or NDE based on first clinical history has been reported to help determine patient prognosis.Reference Pohlmann-Eden, Beghi, Camfield and Camfield 2 We found that the prevalence rate of depression increases with duration of undiagnosed epilepsy at the time of first clinical assessment. That is, the diagnoses of first seizure, NOE, and NDE represent a sequentially increased risk of presenting with depressive symptoms (Figure 3). Based on our results, we speculate that an increase in duration of seizure history leads to an increase in depression through upset of the neuroanatomical structures important in mood stabilization. This idea of a underlying neurobiological mechanism to seizure development through psychiatric disorders has been proposed previously by Kanner,Reference Kanner 6 , Reference Kanner 19 , Reference Kanner 20 and others have reported an increase in seizure frequency was associated with increased prevalence of depressive symptoms.Reference Thapar, Roland and Harold 21 One suggested mechanism may be that depression increases seizure frequency through the mechanism of sleep deprivation.Reference Jackson and Turkington 22 Taken together, we add further clinical evidence of a bidirectional relationship between depression and seizures based on length of seizure occurance.Reference Kanner, Schachter and Barry 23 Anxiety, however, did not show the same intercorrelation in our study populations.
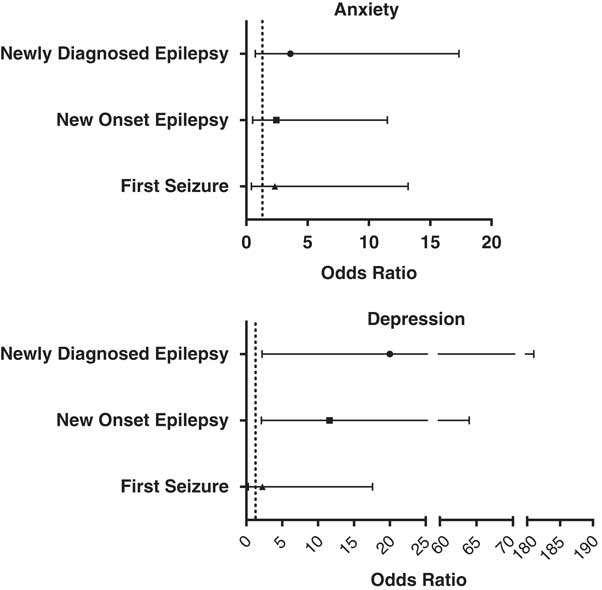
Figure 3 Odds ratio of anxiety and depression for first seizure, new0onset epilepsy, and newly diagnosed epilepsy.
Interestingly, both unprovoked first seizure patients with comorbid anxiety or depression had a significant greater number of abnormalities in imaging of the temporal lobe region. This finding has to be interpreted with all caution because the numbers of these subgroups are very small. It provides further support to the current view that in few patients a common pathway in the highly connected temporal lobe may explain the cooccurrence of seizure onset and psychiatric comorbidity.
Our study is limited by its use of screening questionnaires as a tool for the diagnosis of anxiety and depression because they are not a substitute for a full psychiatric examination. Further, we are aware that our control group is not an ideal population and results may be biased by the fact that nonblood relatives such as partners may be exposed to similar anxiety levels because they share a common household and social environment. Furthermore, our study is significantly underpowered to draw clear conclusions regarding semiology of first seizure presentations.
In conclusion, evidence from our study supports a bidirectional relationship between the onset of seizures and the presence of psychiatric symptoms of depression at time of initial presentation. Certain patient and diagnostic variables may act as red flags for further psychiatric investigation and careful reassessment for risk of seizure recurrence. We conclude that screening for psychiatric disorders at the first presentation of unprovoked seizure provides valuable information that may help determine the course of a patient’s illness. Appropriate management of these disorders must be an integral component of caring for patients with epilepsy.
Acknowledgments and Funding
This research was supported by a research grant from the Epilepsy Association of Nova Scotia.
Disclosures
BP-E received a grant from the Epilepsy Association of Nova Scotia. MB received a grant from the Epilepsy Association of Nova Scotia. CC, KL, and CL have nothing to disclose.








