In past decades, monumental progress has been made on under-5 year child mortality reduction in China. The under-5-children-mortality rate was mitigated by 78 %, from 79·2/1000 live births in 1991 to 10·7/1000 live births in 2015; this improvement led the country to achieve the Millennium Development Goal 4 ahead of schedule( Reference Wang, Li and Zhou 1 , 2 ). In addition to substantial improvement regarding childhood survival status, there has been a significant increase of attention by both the government of China and the global community in regard to achieving early childhood development goals over the past years( 3 , 4 ). Globally there are over 250 million children, of that number the 17·43 million that live in China were estimated to be unable to fulfil their full potential due to multiple adversities which can be marked by the lack of adequate nutrition, poor health or stimulation, inadequate nurturing, and perilous environments according to the newly released Lancet series( Reference Ruyter 5 , Reference Black, Walker and Fernald 6 ).
Maternal and child nutrition status plays an important role in infant morbidity, early development and even long-term health; childhood stunting is the foundational cause of poor cognition, low adult wages and lost productivity later in life( Reference Black, Victora and Walker 7 ). The 65th World Health Assembly set a target that by the year of 2025, the stunting prevalence of children under 5 years should be mitigated by 50 % as compared with the baseline in 2010 established by the World Health Organization( 8 ). Globally, approximately 171 million children under the age of 5 years had some sort of stunting that affected their development( 9 ). Previous studies have shown that the stunting prevalence inequality among different populations is attributed to social, economic and political determinants( Reference Black, Victora and Walker 7 , Reference Martorell and Young 10 ). Among all risk factors, feeding practices has the most direct impact upon childhood stunting. More so, appropriate interventions on the modification of feeding practices has been proved to be effective( Reference Bhutta, Das and Rizvi 11 , Reference Correia, Silva and Campos 12 ).
The significant inequities on under 5-year child survival situations among different regional populations and ethnic minority groups in China have been recognised at the national level( Reference Wang, Li and Zhou 1 ). Some regional studies report that the stunting rate among minorities was higher than the Han’s, which is the major ethnic group in China( Reference Dang, Yan and Wang 13 – Reference Wu, Yang and Yin 16 ). In addition to the socio-economic disparities, ethnic minorities have various culture and religious beliefs; therefore, these fundamental roles may dictate their feeding patterns and which may differ from the Han’s dietary practices. For example, a previous study within Tibet suggested that unbalanced diets may be linked to a greater stunting prevalence in Tibetan children living at a higher altitude( Reference Bianba, Yangzong and Gonggalanzi 17 ). Moreover, Uygur mothers were unlikely to feed their children breast milk exclusively within the first 6 months; this is due to the traditional belief that breast milk was inadequate for the growth of children( Reference Xu, Binns and Nazi 18 ). Tibetan mothers were also inclined to introduce water early as following their ethnic tradition( Reference Harris, Crawford and Yangzom 19 ). Although some studies have reported breast-feeding practices of the Chinese ethnic minorities, limited studies focused on complementary food diversity of children and the influence of different dietary patterns on the growth of children. To further support interventions on mitigating stunting in poor and remote minority areas, it is first necessary to understand the current prevalence of stunting and its numerous risk factors. Therefore, we conducted a population-based study in forty-two rural counties in the western provinces of China; these areas accounted for most of China’s ethnic minorities as well as the most resource limited region in China. Our study methods were designed to identify the association between complementary dietary diversity and infant stunting, especially the impact for children of various ethnic groups and their respective varying dietary patterns.
Methods
Study design and setting
This study was a cross-sectional baseline survey on feeding practices and child growth in 2011, covering forty-two rural counties in seven western provinces of China (Gansu, Qinghai, Xinjiang, Sichuan, Guizhou, Yunnan and Tibet), as part of maternal and child health (MCH) programme funded by UNICEF and the National Health And Family Planning Commission Of China (NHFPC). Counties were selected by NHFPC and UNICEF as programme counties due to their poor socio-economic development in addition to low MCH performance. Under-5 mortality rates were higher in surveyed counties (up to 21·1/1000 live births) as compared with the national average of 16·4/1000 live births in 2010; the per capita income of 3239 RMB within these forty-two counties were below the national average 5919 RMB in 2010( 20 ). The Ethical Committee of Peking University Health Science Centre approved this study.
A multistage sampling method was employed to select townships and villages in each county. First, fifteen administrative villages per county and two nature villages per administrative village were selected at random with population proportional to size. Within each selected nature village, ten households with children under 3 years of age were selected according to a full registration list for each village by simple random sampling; the list of children was provided by local village doctors. Random numbers for selection criteria were generated by a random number table, and staff members of this programme completed all the sampling processes. In sparsely populated Tibet, only two or three households with children under 3 years were randomly sampled and selected in each nature village. The youngest children and their caregivers in each selected household were interviewed face-to-face.
Because this study was designed to collect relevant baseline data for a childhood intervention project, we expected to see a decrement in stunting prevalence in the final evaluation. The following formula was used to calculate the sample size:
We used 0·05 as the statistical significance (α) and set the power of the test (1−β) as 0·8. We assumed the baseline stunting prevalence (p 0) would be 50 % and expected a relative 20 % decrement of stunting prevalence (p 1–p 0)/p 0. Finally, in consideration of a design effect of 2 and with an 80 % response rate, the needed total sample size of children would be 1944 (972:972).
Data collection
A structured questionnaire for caregivers was provided in our survey. Items in the questionnaire were selected from ‘Multiple Indicator Cluster Survey’ manual published by UNICEF( 21 ). The dietary intake diversity assessment involved seven foods groups: (1) grains, roots and tubers, (2) legumes and nuts, (3) dairy products (milk, yogurt and cheese), (4) flesh foods (meat, fish, poultry and liver/organ meats), (5) eggs, (6) vitamin A-rich fruits and vegetables and (7) other fruits and vegetables. Data on dietary intake for the children 24 h before the survey were obtained through caregivers’ recall. The questionnaire also included questions on the socio-economic characteristics of the household (ethnicity, education of the caregivers and income) and on the age, sex, birth order and place of delivery of the children.
Length (for children aged 0–23 months) and height (for children aged 24–35 months) were measured by two anthropometrists in each sampled village. Each measurement was performed twice and the average of both dimensions were used in the analysis. All anthropometrists underwent a systemic standardised anthropometric training before the study and followed the unified anthropometry manuals for consistent results. All village study sites used the same high-precision measuring equipment. Length was measured to the nearest 0·1 cm with the WB-B Length Meter (Wujin Weighing Apparatus Factory). Height was measured to the nearest 0·1 cm with the SH-2B Stadiometer (Wujin Weighing Apparatus Factory). Data collection was monitored for quality control by the Peking University/UNICEF team in fourteen counties and by staff from the local health bureau or the MCH hospitals in twenty-eight counties. All data collected were entered as dual replicates into a database.
Statistical analysis
WHO 2006 Child Growth Standard, length/height-for-age z scores (HAZ) was used as an evaluation standard of stunting status as recommended by WHO( 22 ). All children with z score of HAZ below 2 were defined as stunted within our study. The minimum dietary diversity (MDD) was selected from ‘Indicators for assessing infant and young child feeding practices’ published by WHO in 2008 as a core indicator in our study for accessing complementary feeding practice( 23 ). WHO guidelines implied that MDD was defined as ‘receiving foods from 4 or more food groups 24 h previous to the survey was given’( 23 ). We also use the term ‘inadequate MDD’ to refer to children who did not achieve the recommended MDD in the following context.
Within our study, thirty-two different ethnic groups were reported and ethnicity was categorised as either Han or other minority groups (Yi, Tibetan, Miao and other ethnics). Additional covariates include sex of children (male and female), age of the child, birth order of children (1, 2, 3 or more), caregiver’s education (illiterate, primary school, secondary school, college and above), place of delivery (county hospital, township hospital or at home), income (poorest, poor, middle, richer and richest) and breast-feeding during the previous day (yes/ no).
As the MDD index is generally targeted for infants under the age of 2 years, we restricted our study population to children aged 6–23 months for the final analyses( 8 ). Socio-economic characteristic distributions were calculated and compared between children within the Han and minority groups using chi-square tests. Socio-economic determinants of inadequate MDD and stunting were examined with Poisson regression; all were weighed for the variation in the sampling distribution of a population of children 6–23 months across counties. Both crude, adjusted relative risks and 95 % CI reports were adjusted for the child’s sex, age, birth order, ethnicity of the caregiver, caregiver’s education, the place of birth, income, breast-feeding during the previous day and MDD (only for stunting). We also calculated and compared the frequencies of each types of complementary foods consumptions among different ethnic groups and by different age groups. All analyses were conducted using STATA version 13.0.
Results
Samples description
In our survey, a total of 8964 children aged under 5 years were interviewed. The present study included 5196 children aged 6–23 months; among them, 53·1 % were males and 53·8 % were the first baby for their parents. A total of 31·5 % of children’s caregivers were illiterate, and 23·8 % children were delivered at their home, as shown in Table 1. Among all children belonging to various proportions of ethnic groups there were 38·0 % Han, 13·8 % Yi, 13·0 % Tibetan, 8·6 % Uighur and 26·5 % belonged to other minority groups. The distributions of various age groups were similar in different ethnic groups (P=0·234). Slight differences in child sex distribution showed variation between different ethnic groups (P<0·05). For caregiver’s education, 68·7 % of the Yi and 58·5 % of the Tibetan groups were illiterate; in contrast, the prevalence of illiteracy was only 22·2 and 3·4 % among the Han and Uighur groups, respectively. Different ethnic groups also showed disparity based on the place of delivery. For example, 19·6 % of the Yi children were delivered at a county level hospital, this proportion was higher in the Tibetan (49·9 %), Uighur (67·2 %) and Han children (73·1 %). Moreover, the income level in Han group had a relatively balanced distribution, whereas the other ethnic groups had more households belonged to the poorest or poor quintiles of income (Han: 37·0 %, Yi: 72·5 %, Tibetan: 50·0 %, Uighur: 48·8 %, P<0·001). The Han group also had less of the proportion of breast-feeding during the previous day as compared with other minorities (Han: 37·3 %, Yi: 65·5 %, Tibetan: 40·1 %, Uighur: 55·6 %, P<0·001), as shown in Table 1.
Table 1 Socio-demographic characteristics among children aged 6–23 months with Han and ethnic groups in forty-two counties in Western China (2011) (Numbers and percentages)
Minimum dietary diversity
Table 2 showed the bivariate and multivariate regression output of risk factors associated with an inadequate MDD. Among children within the age groups of 6–23 months in our study, 44·5 % of them did not achieve the MDD. Among all ethnic groups, the Yi minority had the poorest performance with 73·1 % of children not reaching MDD. The Uighur and Tibetan groups also had a relatively high probability of not receiving the MDD in their daily meals, as compared with the Han children. The variations of inadequate MDD differed by age, birth order of children, caregiver’s education level, place of delivery, income and breast-feeding during the previous day were also significant. Children aged 6–11 months had a higher proportion of inadequate MDD as compared with older children (58·6 v. 36·1 %, adjusted risk ratio (RR)=1·39). Children with a birth order of being third or greater had a higher proportion of the inadequate MDD in comparison to first born children (65·9 v. 38·2 %, adjusted RR=1·07). Children with illiterate caregivers had the highest probability of inadequate MDD (58·8 %) in comparison with other caregivers with higher education levels. In addition, children from the poorest quintile families who were delivered at home had a significant positive association with poor performance on dietary diversity, with adjusted RR of 1·32 and 1·30, respectively. No significant difference of dietary diversity was found between male and female children.
Table 2 Relative risks of inadequate minimum dietary diversity among children aged 6–23 months in forty-two counties of Western China (2011) (Percentages, relative risks and 95 % confidence intervals)
* Adjusted for all the variables in Table 2.
Further analysis on types of complementary foods found that 91·2 % of children received grains, roots and tubers during the previous day of survey, as shown in Fig. 1. More than half of children received dairy products (57·4 %), flesh foods (54·2 %), vitamin A-rich fruits and vegetables (57·1 %) and other fruits and vegetables (57·9 %), respectively. Only 34·3 % of children had eggs intake and only 15·9 % of children received legumes and nuts. When comparing variation of these types of complementary foods by ethnic groups as compared with other, it was found that the Yi group had a lower consumption of every kind of complementary foods, especially dairy products (Yi v. Han=19·5 v. 62·9 %, P<0·001), eggs (Yi v. Han=25·1 v. 43·6 %, P<0·001), vegetables and fruits (Yi v. Han=41·6 v. 71·8 %, P<0·001). The Uighur ethnic also showed similar results with most types of complementary foods intake; the only exceptions were for flesh foods (68·5 %), and non-vitamin A-rich fruits and vegetables (61·6 %). Tibetan children tend to have a greater intake of dairy products in comparison to other ethnic groups (Tibetan v. Han=75·1 v. 62·9 %, P<0·001), but generally have a lower intake of legumes and nuts (Tibetan v. Han=12·3 v. 26·4 %, P<0·001), eggs (Tibetan v. Han=25·9 v. 43·6 %, P<0·001), fruits and vegetables (Tibetan v. Han=52·5 v. 69·8 %, P<0·001). After stratification by age groups, the consumption of all types of foods by different ethnic groups were higher among children aged 12–23 months as compared with children aged 6–11 months, except for the consumption of dairy products within the Yi and Uighur groups. Moreover, the Han children showed higher consumption rates of nearly every types of food and had more children achieved MDD than other ethnicities, in both the 6–11 and 12–23 months groups.
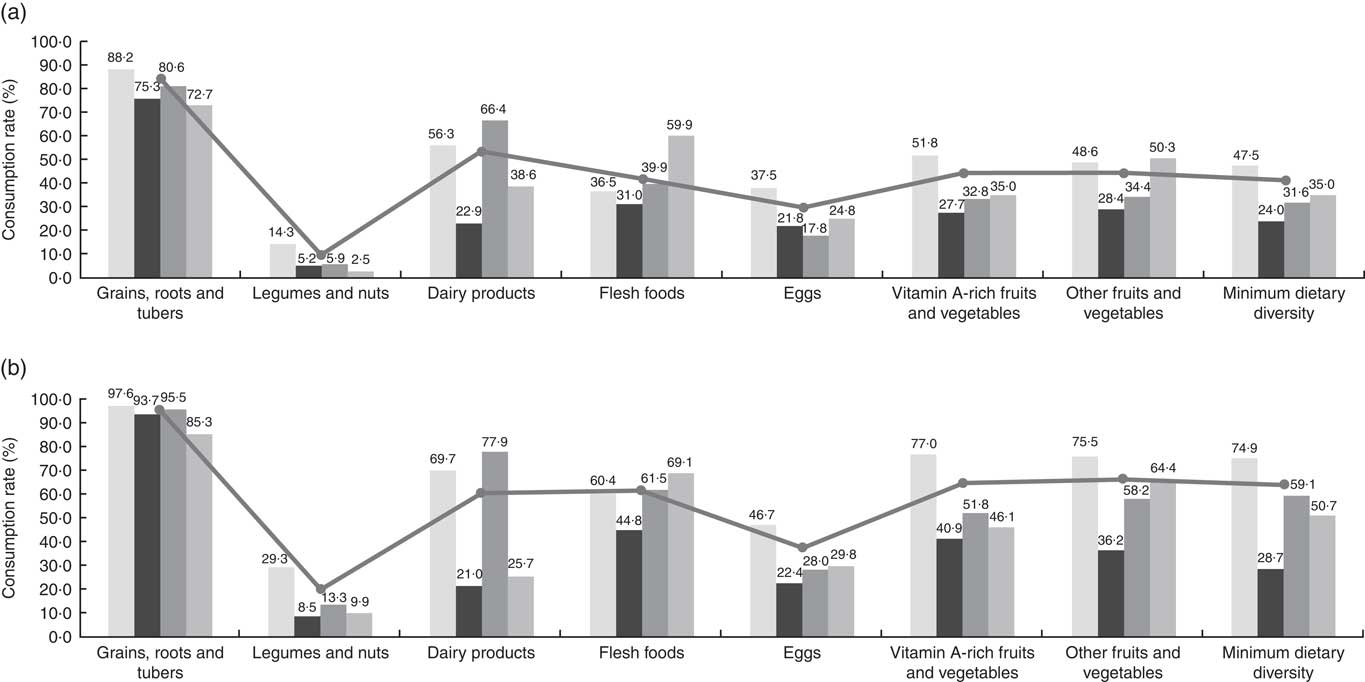
Fig. 1 Comparison of complementary food diversity among children aged (a) 6–11 months and (b) 12–23 months by ethnic groups. ![]() , Han;
, Han; ![]() , Yi;
, Yi; ![]() , Tibetan;
, Tibetan; ![]() , Uighur;
, Uighur; ![]() , total.
, total.
Stunting
As shown in Table 3, the overall prevalence of stunting in surveyed areas was 17·8 %. The prevalence of stunting among children aged 12–23 months is nearly twice as much in comparison with children aged 6–11 months (21·8 v. 11·1 %, adjusted RR=2·10). Young males appear to have a higher prevalence of stunting in comparison with their female counterparts (20·8 v. 14·3 %, adjusted RR=1·44). Based on the multivariate analysis, elder aged males delivered at home and from a poor family with a low income were found to be significantly associated with the child’s stunting. In addition, there were significant statistical associations between individual ethnic groups and stunting. The Yi, Tibetan and Uighur’s children had 1·25, 1·29 and 1·72 times greater risk of stunting in contrast to children from the Han minority, respectively. Table 3 also examined the association between MDD and stunting. After adjusting for all other factors, children who did not achieve the MDD had a 1·15 times greater risk of stunting in comparison with those who received the recommended dietary intake. The gap of stunting prevalence among different ethnic groups was large. For the Han group, only 14·9 % children were stunted, whereas the prevalence for the Yi, Tibetan and Uighur children were 26·5, 20·3 and 24·6 %, respectively.
Table 3 Relative risks of stunting among children aged 6–23 months in forty-two counties of Western China (2011) (Percentages, relative risks and 95 % confidence intervals)
* Adjusted for all the variables in Table 3.
Discussion
Timely and adequate management of complementary diets are necessary for infants aged 6 months and older; breast-feeding exclusively is insufficient to fulfil a child’s nutrition requirements. However to date, socio-economics situations have been known to limit dietary diversity among children in China, especially for those who reside in poorer western regions. Our research showed that 44·5 % of children aged 6–23 months in the forty-two western counties failed to reach the MDD as defined by WHO. The adverse situation on dietary diversity from our study is similar to other surveys conducted within China’s western areas( Reference Hipgrave, Fu and Zhou 24 , Reference Ban, Guo and Scherpbier 25 ) and some undeveloped countries( Reference Joshi, Agho and Dibley 26 – Reference Beyene, Worku and Wassie 28 ). But the status was far worse as compared with those from the eastern regions (e.g. 60 % for children aged 6 months and nearly 100 % for children aged 12 months reported in Shanghai received MDD( Reference Woo, Herbers and McMahon 29 )) and central areas (e.g. reported from the poor rural counties in Hunan Province, 73·9 % of the children aged 6–23 months received MDD( Reference Zhou, Fang and Luo 30 )) in China; this stark difference is indicative of a serious problem involving dietary diversity for children in Western China.
From the multivariable analysis results, socio-economic factors such as caregivers with low education level, low family income and children delivered at home were found to have greater risks of an inadequate MDD; these findings may suggest the importance of education, socio-economic status and access to health care services in relation to proper feeding practice. The sex of children’ had insignificant impact on the adequacy of dietary diversity, this observation was consistent with most other studies( Reference Hipgrave, Fu and Zhou 24 , Reference Joshi, Agho and Dibley 26 , Reference Liu, Li and Gong 31 ). In addition, children with a higher birth order were less likely to have a diversified feeding pattern which may indicate a negligence on a child’s individual care when parents have more than one child.
One highlight of our study were the stark differences and similarities observed based on feeding patterns by different ethnicities. First, minority groups showed a greater dietary disparity in comparison with the Han group. Nearly two-thirds of the Han’s children met the MDD criteria; this contrasts with the only one-fourth of the Yi’s, about half of the Uighur, and Tibetan children who met the similar criteria. Furthermore, we observed that children from various ethnic groups showed different patterns of complementary food in addition to a standardised diet. For all the studied ethnic groups, grains, roots and tubers comprised predominant proportion of their diets, but legumes and nuts are rarely chosen. Due to the high altitude and barren soil, most Tibetans lived on a grazing based lifestyle; therefore, groups within this population rely more on meat and dairy products as a common food source within their diets, rather than vegetable and fruits. Although meat and dairy food can provide protein, abundant energy content, and micro-elements such as Fe and Zn, there is a greater need for caregivers to be more careful with these sorts of foods and personal hygiene, which may be contaminated at the point of source. The food structure of Uighur children is most comparable with Uighur adults; this would include a greater intake of flesh foods, but less eggs, dairy products, vitamin A-rich fruits and vegetables intake. As previously mentioned meat may provide essential amino acids, additionally the increase of dietary cholesterol as found in eggs and dairy products is noticeable; the high protein and high energetic intake maintained in adult diets may lead to unbalanced growth or development in children. On the other hand, dietary patterns among ethnic groups were also shown to be subject to modification by age groups; older children are more likely to be exposed to a greater diversity of food types in comparison to their younger counterparts. For children under 1 year of age, those in Han group showed a richer diversity of complementary foods types; these children are more likely to achieve MDD earlier than other groups, this observation may account for lower stunting prevalence within this ethnic group.
Among all the groups studied, the Yi minority showed greatest disparity in nearly every type of food group. One possible explanation for this phenomenon may be due to both limited access to resources and local traditional customs. Most of the Yi people in our study lived in rural mountainous areas with inconvenient traffic infrastructure. The local average household income was low and most residence lived on coarse grains (as other food resources were limited)( Reference Gao, Ran and Xie 32 , Reference Zhou, Huang and Xu 33 ). Lack of sufficient food supplies and proper feeding knowledge, parents may tend to feed their children only with breast milk and grain foods. Further interventions should focus on improving Yi’s simple food structure to further develop feeding practice education specifically for this minorities.
Stunting reflects chronic undernutrition during the ‘critical window’ of growth and development for both infants and young children. The overall stunting prevalence among surveyed subjects living in Western China in our study was 17·8 %; this was higher than the national average prevalence of rural children of 11·2 % and mostly similar to 18·7 % in poor rural areas in 2013( Reference Yu, Zhao and Yang 34 ). Past evidence has illustrated that a lack of food dietary diversity will accumulate to child’s malnutrition status, especially stunting( Reference Arimond and Ruel 35 – Reference Marriott, White and Hadden 37 ), these findings have also been confirmed in our multivariate analysis. A study in India has showed a non-significant difference of stunting prevalence between children with medium and low food diversity, however, the difference became significant when comparing children with high and low food diversity( Reference Fenske, Burns and Hothorn 38 ). Male’s sex was more prevalent in stunting, but this was not observed in complementary food diversity. The high stunting prevalence for male children was consistent with previous studies( Reference Black, Victora and Walker 7 , Reference Jiang, Su and Wang 15 , Reference Fenske, Burns and Hothorn 38 ) and with the high under 5-year mortality rate of boys in China( Reference Wang, Li and Zhou 1 ). Education level and income were found significantly associated with MDD, whereas only income was associated with stunting. The significant association between education and stunting in the binary model disappeared after adjusting for MDD and other variables; this indicates that education levels of caregivers may be only the direct causal factor of MDD, but not stunting (education level→MDD→stunting). Other literatures also observed the association between a caregiver’s education and stunting when the authors did not adjust for dietary diversity( Reference Jiang, Su and Wang 15 , Reference Mallard, Houghton and Filteau 36 ). However, the relationship between income and stunting remains significant in both the binary and multivariable models, these observations suggest that income may confound the relationship of MDD and stunting (income→MDD→stunting, income→stunting). In another way, income is an independent risk factor which can be mediated to reduce stunting in children.
In addition, the gaps of stunting prevalence among different ethnic groups was large. Of the three-major minority ethnic groups investigated (Yi, Tibetan, Uygur), these groups showed higher stunting prevalence in comparison to the Han group. In particular, the prevalence of stunting within the Yi group was as high as 26·5 %, which was comparable with the level of Southern Africa( Reference de Onis, Blossner and Borghi 39 ). As shown in Table 1, different ethnic groups have variable distributions of children’s sex, birth order, caregiver’s education, delivery place, postpartum visit, income and breast-feeding status. Among all these factors above, children’s sex, birth order, caregiver’s education level, place of delivery, income and breast-feeding status are found to be statistically associated with MDD; whereas place of delivery, income and MDD are associated with stunting. Therefore, the disparity among different ethnic groups may be partly accounted for by the inequalities of socio-economic factors and complementary dietary performance among different ethnic groups.
Several limitations of our study should be considered. First, the tool we used to assess dietary diversity of children is 24-h dietary recall; whereas this method is rather convenient for collecting data, this conservative approach may affect our information on the food diversity based on caregiver recall bias. In addition, the types of food consumed by children may vary from day by day, therefore the results of the survey in 24 hs may differ from the actual dietary situation. Second, our study only focused on types of complementary foods, rather than the meal frequency, food quantity, food sanitation or caregiver hygiene; other feeding practice factors which are also key indicators of child growth and may play roles in developing sufficient interventions to reduce stunting prevalence. One important strength of our study is that there is a scarcity of literature that focus on dietary diversity issues in Western China; our novel results may contribute to current evidence of associations between dietary diversity and the stunting of children within western rural areas.
To conclude, our study found that nearly 44·5 % complementary feeding diversity has not met the WHO recommended MDD; an overall 17·8 % stunting rate is existent in the poor counties of Western China. Inadequate MDD was found to be positively associated with childhood stunting. Moreover, different ethnicities showed greater variation in achieving MDD and should be further explored in future research to benefit individual groups as well as the general health of Western China. To halve the stunting prevalence by 2025, further efforts are needed: for regions with limited food sources, supplementary nutrition programmes should be conducted; for these ethnic minority groups, health education for caregivers as well as nutrition interventions focusing on feeding practices in tandem with local culture and food availability improvement should be addressed.
Acknowledgements
The authors would like to thank research teams from Lanzhou University, Guangxi Medical University and Chongqing Medical University for their hard work in orchestrating the field work and identifying study population. The authors also want to thank all of family members who participated in this study from the forty-two counties in Western China.
This work was funded by a grant from UNICEF China (YH702).
H. Z. and A. W. formulated the research question and the first draft of the article and analysed the data. Y. W., H. Z., R. W. S., X. H., S. G. and Y. Y. designed study and carried it out. J. J.-S. and C. M. proofread and polished the language of this article. Y. W. and H. Z. provided overall guidance to the study. All authors contributed to the writing and revision of the article.
The authors declare that there are no conflicts of interest.






