The interplay between personality disorder and mental state disorder is increasingly recognised as needing clinical attention, with the former often significantly influencing the latter. There is a growing understanding that personality disorders are an important cause of morbidity worldwide, Reference Tyrer, Mulder, Crawford, Newton-Howes, Simonsen and Ndetei1 and that the disorder influences treatment outcomes for many other health conditions. Reference Tyrer, Reed and Crawford2 Typically the coexistence of a personality disorder leads to worse outcomes in the treatment of mental state disorders, and this has been described for internalising disorders such as depression and eating disorders, Reference Newton-Howes, Tyrer and Johnson3–Reference Steinhausen5 as well as schizophrenia. Reference Newton-Howes and Marsh6 It is not so clear, however, that a negative association exists between the outcomes of externalising mental state disorders and personality disorder. Nonetheless, personality has for some time been an area of research activity in externalising disorders, particularly alcohol use disorders (AUDs). Indeed, until the late 1960s alcoholism was considered to be a form of personality disorder. Reference Sellman, Foulds, Adamson, Todd and Deering7 Population data from the USA suggest that 29% of those with a current AUD have a personality disorder. Reference Grant, Stinson, Dawson, Chou, Ruan and Pickering8 This figure is significantly higher than that in the general population, where the prevalence of personality disorder has been estimated at 2–6% internationally. Reference Huang, Kotov, De Girolamo, Preti, Angermeyer and Benjet9 An even higher prevalence of personality disorder, particularly antisocial personality disorder (ASPD), has been reported in treatment-seeking samples of patients with AUD, Reference Arias, Szerman, Vega, Mesias, Basurte and Morant10,Reference Ross, Glaser and Germanson11 with the prevalence of personality disorder occasionally reported as being over 50%. Reference Bowden-Jones, Iqbal, Tyrer, Seivewright, Cooper and Judd12 This range of prevalence data suggests both that personality disorder is clearly identifiable in patients with AUD and is more common in AUD than in the general population, but is not ubiquitous with the psychosocial problems in AUDs.
Given the high prevalence of personality disorder in patients with an AUD, and the evidence that personality disorder is relevant to treatment outcome in other mental state disorders, closer investigation of the role of personality disorder in treatment outcome for patients with AUD is needed. If it is the case that personality disorder is relevant, there is also a need to determine whether this is the case for all types of alcohol outcomes or just a subset. Although it has historically been believed that the presence of a coexisting personality disorder leads to worse treatment outcomes for patients with AUD, Reference Rounsaville, Dolinsky, Babor and Meyer13 a recent review of predictors of AUD treatment outcome more generally did not find strong evidence that this is the case. Reference Adamson, Sellman and Frampton14 However, this review identified only a small number of relevant studies, most of which focused on ASPD rather than other types of personality disorder. A narrative overview of the literature does not provide any clear indication of the association between AUD and personality disorder. We therefore aimed to perform a systematic review of the association between personality disorder status and alcohol treatment outcomes for patients with an AUD.
Method
Conduct and reporting of the review were designed to conform to guidelines for the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). Reference Moher, Liberati, Tetzlaff and Altman15 The review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO; registration CRD42015023972) prior to literature searching. A single amendment was made to the protocol to remove ambiguity following the literature search, but no change was made to the populations examined or the primary outcomes as predefined The change specified the Addiction Severity Index as a measure of psychosocial functioning, Reference McLellan, Luborsky, Woody and O'Brien16 the use of retention in treatment as a secondary outcome and provided clarity around quality assessment using the Newcastle–Ottawa Scale. Reference Wells, Shea, O'Connell, Peterson, Welch and Losos17 The protocol was designed to identify studies reporting on the association between categorical personality disorders or dimensional personality traits and alcohol treatment outcomes in clinical trials. Only outcomes relating to categorical disorders are presented.
Eligibility criteria
Randomised controlled trials and longitudinal studies in which psychosocial and/or pharmacological treatments were provided for an AUD were considered for inclusion. Studies were required to have examined the association between personality disorder status and treatment outcome over at least 8 weeks. As the diagnostic criteria for AUD and personality disorder have evolved over time, any paper from 1980 onwards with clear diagnostic criteria for these two disorders was considered for inclusion. Studies were required to have been published in peer-reviewed journals subsequent to the introduction of DSM-III in 1980 because of the increased diagnostic rigour from this time, 18 improving homogeneity of the populations studied. Dissertation abstracts and conference proceedings, and studies examining treatments for the personality disorder rather than AUD, were not considered for inclusion.
Search strategy and selection criteria
A broad search strategy was employed in line with prior personality disorder and mental state disorder systematic reviews, Reference Newton-Howes, Tyrer and Johnson3,Reference Newton-Howes, Tyrer, Johnson, Mulder, Kool and Dekker4 in order to minimise the risk of overlooking important research. Searches were undertaken using the Ovid platform in Medline, Cochrane, EMBASE and PsycINFO from 1980 until 24 November 2015. For personality disorder the search terms used were personality, personality disorder, antisocial borderline, schizoid. For AUDs the search terms were alcohol related disorder, alcohol dependence, alcohol abuse, alcohol addiction and alcoholi*. Results from each keyword within alcohol and personality clusters were combined with the Boolean classifier OR, and the two searches were then combined with the Boolean classifier AND. In addition, hand searches of articles cited by previous reviews and articles referenced in the papers in our final sample were conducted. Two authors (J.A.F. and G.M.N.-H.) independently screened the titles and abstracts of citations identified by the search strategy. Citations identified as potentially relevant were then compiled into a screened sample by consensus. The full text of these articles was then independently reviewed by two authors (N.H.G. and J.A.F. or G.M.N.-H.) to determine whether studies met inclusion criteria. Where two or more articles referred to the same study population, the article providing the most robust reporting of the systematic review's a priori primary outcomes was selected. Data from other articles pertaining to the same study sample were then used only to provide information about baseline patient data.
Outcomes
The primary alcohol outcomes were time to relapse and self-reported alcohol consumption (quantity and frequency). Two other outcomes that were not nominated a priori in the review protocol were also investigated, as it became apparent during the process of the review that they were commonly reported. These were retention in treatment and scores on the Addiction Severity Index. Reference McLellan, Luborsky, Woody and O'Brien16
Data collection and extraction
A data extraction form was used to record key characteristics of each trial included in the final sample. Data were extracted independently by at least two authors (N.H.G. and G.M.N.-H. or J.A.F.). The data extracted were sample size, demographic characteristics of sample (age, gender), baseline AUD, type of interventions provided to study participants, treatment setting, study completion rate, alcohol outcomes and personality disorder diagnosis. All information was cross-checked by at least two authors conferring. Study authors were contacted with requests for further information on outcomes that were not clearly reported in published material. It was agreed a fourth review author (J.M.B. or R.T.M.) would moderate if consensus could not be reached in regard to inclusion or data extraction; however, this did not occur.
Assessment of study bias
Study quality and potential for bias was assessed using the Newcastle–Ottawa quality assessment scale. Reference Wells, Shea, O'Connell, Peterson, Welch and Losos17 This is a widely used tool for assessing the quality of non-randomised studies, and was chosen in preference to tools that emphasise randomisation and blinding procedures, because treatment effects in clinical intervention studies were not of primary interest in this review. Reported outcomes were checked against published trial protocols. Disagreements about trial quality were resolved by discussion between at least two review authors.
Synthesis of results
For outcomes where results from at least three studies were available and reporting quality was adequate, heterogeneity was assessed using the I 2 measure. Reference Higgins and Green19 Random effects meta-analysis was then conducted using RevMan version 5.3 software. 20 Where meta-analysis was not possible a narrative account of the quantitative findings of the included papers was used.
Quality of evidence and risk of bias
The GRADE approach was used to assess the quality of evidence for each clinical outcome across studies. Reference Guyatt, Oxman, Vist, Kunz, Falck-Ytter and Alonso-Coello21 This approach assesses the quality of a body of evidence for a particular outcome of interest by summarising data quality for that outcome across studies using a standardised heuristic. Reference Higgins and Green19 The GRADE method combines information about study conduct, consistency of outcome measures, generalisability and magnitude of effect size.
Results
In all, 22 studies were included in the review, comprising 4861 participants (Fig. 1). Of these studies, 21 were in English and 1 was in German. Of the 22 included studies, 9 primarily examined ASPD; Reference Booth, Yates, Petty and Brown22–Reference Cacciola, Alterman, Rutherford and Snider30 3 examined borderline personality disorder (BPD); Reference Caputo, Francini, Brambilla, Vigna-Taglianti, Stoppo and Del Re31–Reference Rolland, Valin, Langlois, Auffret, Gautier and Deheul33 1 investigated ASPD or BPD; Reference Ralevski, Ball, Nich, Limoncelli and Petrakis34 and the remaining 9 studies reported on the presence of any personality disorder. Reference Bottlender, Bottlender, Scharfenberg and Soyka35–Reference Zikos, Gill and Charney43 The characteristics of these studies are shown in Table 1.

Fig. 1 Study search.
Table 1 Summary of studies included in systematic review

| Quality rating a |
Time to outcome |
Personality measure | ||||||
|---|---|---|---|---|---|---|---|---|
| Study | Design | n | Drinking pattern b | Disorder | Tool | Major findings | ||
| Booth et al (1991) Reference Booth, Yates, Petty and Brown22 | 4 | Cohort | 255 | 15 mo | Unknown | ASPD | DSM-III | ASPD not associated with any difference in readmission risk |
| Bottlender et al
(2002) Reference Bottlender, Bottlender, Scharfenberg and Soyka35 |
3 | Cohort | 102 | 6 mo | Any Axis II | DSM-IV, SCID–II | No significant difference between groups with and without personality disorder in relation to relapse or study completion |
|
| Cacciola et al (1995) Reference Cacciola, Alterman, Rutherford and Snider30 | 3 | Cohort | 141 | 7 mo | ‘Alcohol dependent’ | ASPD | DSM-III, DIS | ASPD group showed significant improvement in all domains measured by the ASI, and had a comparable percentage of heavy drinking days in follow-up despite heavier drinking at baseline |
| Caputo et al (2011) Reference Caputo, Francini, Brambilla, Vigna-Taglianti, Stoppo and Del Re31 | 4 | Cohort | 48 | 12 wk | ‘Alcohol dependency’ | Mainly BPD | DSM-IV-TR | No significant difference between groups with and without personality disorder in relation to continuous abstinence from alcohol or treatment retention |
| Charney et al
(2015) Reference Charney, Heath, Zikos, Palacios-Boix and Gill36 |
5 | RCT | 265 | 12 wk | Drinking past 20 or 30 days on admission |
Any Axis II | DSM-IV, SCID–II | Personality disorder associated with treatment non-response, treatment drop-out and shorter time to relapse |
| Hunter-Reel et al
(2014) Reference Hunter-Reel, Epstein, McCrady and Eddie37 |
3 | RCT | 102 | 6 mo | Unknown. Must have used alcohol within the past 60 days |
Any Axis II | DSM-IV, SCID–II | Avoidant and dependent personality disorders, but not other personality disorders, were associated with higher percentage days drinking |
| Krampe et al (2006) Reference Krampe, Wagner, Stawicki, Battels, Aust and Kroener-Herwig38 | 3 | Cohort | 112 | 4 yr | Unknown | Any Axis II | DSM-IV, IDCL-P | Patients with personality disorder had less cumulative abstinence and shorter time to relapse |
| Kranzler et al (1996) Reference Kranzler, Del Boca and Rounsaville23 | 3 | Cohort | 225 | 3 yr | ‘Alcohol abuse or dependence’ | ASPD | DSM-III, DIS | Patients with ASPD had more drinks per drinking day, a higher percentage of drinking days and more alcohol-related symptoms at follow-up |
| Longabaugh et al
(1994) Reference Longabaugh, Rubin, Malloy, Beattie, Clifford and Noel24 |
4 | RCT | 229 | 18 mo | ‘Alcohol consumption was high’; ‘49% hospitalised for alcohol-related reasons’; ‘81% alcohol dependence’ |
ASPD | DSM-III, DIS | ASPD not associated with any difference in average daily consumption or drinks per drinking day. However, ASPD was associated with lower percentage of drinking days |
| Nace et al (1986) Reference Nace, Saxon and Shore32 | 4 | Cohort | 74 | 1 yr | ‘Most patients were solely alcoholics’; all in-patients |
BPD | DSM-III, DIS | No significant difference between BPD and non-BPD groups in relation to drinking days or total abstinence |
| Nielsen et al (2007) Reference Nielsen, Rojskjaer and Hesse39 | 3 | Quasi-randomised trial | 108 | 9 mo | ‘Mainly alcohol-dependent clients’ | Any Axis II | MCMI | No significant difference in treatment completion between personality disorder and non-disorder groups |
| Nordholm & Nielsen (2007) Reference Nordholm and Nielsen40 |
4 | Non-randomised controlled trial |
363 | 1 yr | ‘87% alcohol dependent and 13% alcohol abusers’ |
Any Axis II | ICD-10-R | Patients with personality disorder had more drinking days and higher ASI alcohol scores |
| Poldrugo & Forti (1988) Reference Poldrugo and Forti41 |
4 | Cohort | 404 | 1 yr | ‘Alcoholics’ | Any Axis II | DSM-III | Patients with personality disorder in general had similar or worse outcomes to those without such disorder, except dependent personality disorder who had better outcomes, and ASPD who had worse outcomes |
| Powell et al (1992) Reference Powell, Penick, Nickel, Liskow, Riesenmy and Campion25 | 3 | Cohort | 360 | 1 yr | ‘Alcoholic men’ | ASPD | PDI | No difference between ASPD v. other groups in relation to total abstinence or drinking days |
| Powell et al (1995) Reference Powell, Campbell, Landon, Liskow, Thomas and Nickel26 | 2 | RCT | 216 | 6 mo | ‘DSM-III compatible alcohol dependence’ | ASPD | PDI-R | Patients with ASPD did better with nortriptyline compared with placebo |
| Ralevski et al (2007) Reference Ralevski, Ball, Nich, Limoncelli and Petrakis34 | 2 | RCT | 254 | 12 wk | ‘Alcohol dependence’ | ASPD or BPD | DSM-IV, SCID–II | Personality disorder not associated with any difference in alcohol outcomes. Medication equally effective for patients with ASPD |
| Rolland et al (2015) Reference Rolland, Valin, Langlois, Auffret, Gautier and Deheul33 | 4 | Case-control | 203 | 1 yr | ‘DSM-IV criteria for alcohol dependence’ | BPD | DSM-IV | BPD associated with more heavy drinking days |
| Schuckit (1985) Reference Schuckit27 | 4 | Cohort | 577 | 1 yr | ‘Alcohol abuse or dependence according to DSM-III’; drinking >24 days in the past month |
ASPD | DSM-III | ASPD was not associated with any significant difference in percentage drinking days, drinks per day or maximum drinks per day |
| Tomasson & Vaglum (1996) Reference Tomasson and Vaglum29 |
4 | Cohort | 217 | 1 yr | ‘Treatment seeking alcoholics’ | ASPD | DSM-III, DIS | ASPD was associated with heavier consumption at baseline but not at follow-up |
| Verheul et al (1999) Reference Verheul, Van Den Brink, Koeter and Hartgers28 | 4 | Cohort | 309 | 14 mo | ‘According to CIDI, 85.4% of the patients met criteria for a DSM-III-R alcohol dependence diagnosis. In addition, 9.8% met criteria for DSM-III-R alcohol abuse’ |
ASPD | DSM-III-R, CIDI | ASPD was associated with earlier drop-out but no difference in change in heavy drinking or problem drinking days between ASPD and non-ASPD groups |
| Wolwer et al (2001) Reference Wolwer, Burtscheidt, Redner, Schwarz and Gaebel42 | 4 | RCT | 120 | 6 mo | ‘Alcohol dependence’ | Any Axis II | DSM-III-R, SCID–I | No difference in abstinence for personality disorder compared with no disorder |
| Zikos et al (2010) Reference Zikos, Gill and Charney43 | 5 | Cohort | 177 | 12 wk | ‘Alcohol use disorders’; drinking >19 days in the past month |
Any Axis II | DSM-IV, SCID–II | Cluster B personality disorder patients had earlier drop-out and relapse |
ASI, Addiction Severity Index; ASPD, antisocial personality disorder; BPD, borderline personality disorder; CIDI, Composite International Diagnostic Interview; DIS, Diagnostic Interview Schedule; IDCL-P, International Diagnosis Checklists for Personality Disorders; MCMI, Millon Clinical Multiaxial Inventory; mo, months; PDI(−R), Psychiatric Diagnostic Interview (− Revised); RCT, randomised controlled trial; SCID–II. Structured Clinical Interview for DSM Axis II Disorders; wk, weeks; yr, years.
a. Score on 9-item Newcastle–Ottawa Scale.
b. All fulfil inclusion criteria for alcohol use disorder.
Personality disorder prevalence
Excluding one study that reported only on ASPD that developed before the onset of alcoholism, Reference Schuckit27 the prevalence of ASPD ranged from 15% to 41% (median 28%) in the remaining eight ASPD studies; in the BPD studies, BPD prevalence ranged from 11% to 27% (median 18%); and in studies reporting on any personality disorder, total prevalence ranged from 34% to 71% (median 55%).
Baseline differences between patient groups
Baseline differences between patients with and without personality disorder were assessed to examine whether any association found in outcomes was potentially explained by these differences. Baseline data were not presented in four papers. The reporting of baseline data in the remaining 18 papers was highly variable, and data were therefore summarised narratively rather than by meta-analysis or meta-regression. In the majority of studies alcohol consumption patterns at baseline did not differ between patients with and without a personality disorder, Reference Powell, Penick, Nickel, Liskow, Riesenmy and Campion25,Reference Verheul, Van Den Brink, Koeter and Hartgers28,Reference Ralevski, Ball, Nich, Limoncelli and Petrakis34,Reference Nordholm and Nielsen40,Reference Zikos, Gill and Charney43 although three papers reported heavier alcohol consumption at baseline among patients with ASPD. Reference Longabaugh, Rubin, Malloy, Beattie, Clifford and Noel24,Reference Schuckit27,Reference Tomasson and Vaglum29 There was consistent evidence that patients with ASPD had earlier onset of alcohol use and alcohol problems. Reference Kranzler, Del Boca and Rounsaville23,Reference Powell, Penick, Nickel, Liskow, Riesenmy and Campion25,Reference Schuckit27,Reference Zikos, Gill and Charney43 As expected, patients with ASPD also reported more legal problems, Reference Powell, Penick, Nickel, Liskow, Riesenmy and Campion25,Reference Schuckit27,Reference Verheul, Van Den Brink, Koeter and Hartgers28,Reference Cacciola, Alterman, Rutherford and Snider30 and more concurrent use of other substances. Reference Schuckit27,Reference Cacciola, Alterman, Rutherford and Snider30,Reference Nordholm and Nielsen40,Reference Zikos, Gill and Charney43 Several studies also reported an excess of physical, psychological and social problems among patients with ASPD, Reference Kranzler, Del Boca and Rounsaville23,Reference Verheul, Van Den Brink, Koeter and Hartgers28 and among those with personality disorder more generally. Reference Nordholm and Nielsen40
Primary alcohol outcomes
A wide range of alcohol outcomes were reported, including the a priori outcomes (time to relapse and self-reported quantity and frequency of alcohol consumption). The reporting was, however, heterogeneous and variable in quality, meaning that meta-analyses were only able to include a minority of studies for each outcome. A lack of comparable outcome measures and incomplete statistical reporting were the primary problems.
Time to relapse
Three studies reported that the presence of personality disorder was associated with a significantly shorter time to first relapse. Reference Charney, Heath, Zikos, Palacios-Boix and Gill36,Reference Krampe, Wagner, Stawicki, Battels, Aust and Kroener-Herwig38,Reference Zikos, Gill and Charney43 In a further study that examined time to readmission in a sample of male veterans, the presence of ASPD was not a significant predictor of readmission for alcohol-related problems. Reference Booth, Yates, Petty and Brown22
Alcohol consumption
No study reported alcohol consumption per drinking day or total consumption for those with personality disorder in general, or among patients other than those with cluster BPD. Only one of the four studies that reported on the number of standard drinks consumed per drinking day (DDD) identified personality disorder as a predictor of this alcohol outcome. In this study Kranzler et al reported that ASPD was associated with higher DDD during follow-up (7.3, s.d. = 5.7) compared with those without ASPD (4.9, s.d. = 5.1). Reference Kranzler, Del Boca and Rounsaville23 In a study of 229 patients Longabaugh et al found no overall difference in DDD between patients with and without ASPD during 18 months of follow-up, after adjusting for baseline DDD. Reference Longabaugh, Rubin, Malloy, Beattie, Clifford and Noel24 Schuckit compared participants with primary ASPD (defined as people who had ASPD before the onset of alcohol or other substance problems) with other groups of participants; in this study the primary ASPD group had similar levels of DDD at follow-up (15.7, s.d. = 10.7) compared with those with primary alcoholism (14.3, s.d. = 10.8). Reference Schuckit27 Ralevski et al investigated the effect of ASPD or BPD in a sample of 254 predominantly male veterans. Reference Ralevski, Ball, Nich, Limoncelli and Petrakis34 Patients with ASPD consumed slightly more alcohol in total at baseline compared with those without ASPD (10.9 drinks per day v. 9.6), whereas for BPD v. no BPD the figures were 10.3 v. 9.9 drinks respectively. At follow-up the average level of alcohol consumption was low (<0.5 drink per week) and heavy drinking was infrequent (<5% of days) across the whole sample. No difference in drinks per drinking day was reported according to the presence of ASPD or BPD.
Three studies (n = 875) were able to be included in a meta-analysis of DDD outcomes (Fig. 2). Reference Kranzler, Del Boca and Rounsaville23,Reference Schuckit27,Reference Ralevski, Ball, Nich, Limoncelli and Petrakis34 Outcomes across these studies showed low heterogeneity (I 2 = 20%). People with personality disorder had higher DDD at follow-up (pooled estimate of mean difference in DDD 2.15, 95% CI 0.72–3.58). Two further studies reported findings for total alcohol consumption, with conflicting results. In a case–control study based on a cohort of patients receiving baclofen for alcohol dependence, Rolland et al compared participants with BPD and an age- and gender-matched control group. Reference Rolland, Valin, Langlois, Auffret, Gautier and Deheul33 Patients with BPD drank substantially more per week than those without the disorder (61.3 drinks, s.d. = 49.7 v. 14.7 drinks, s.d. = 24.1 respectively) during follow-up; however, as patients were not matched on the basis of alcohol consumption at baseline, the follow-up findings are difficult to interpret. Conversely, in a prospective study of 351 patients admitted to in-patient detoxification in Iceland, ASPD was associated with heavier consumption at baseline but did not predict consumption at 1 year of follow-up. Reference Tomasson and Vaglum29 The majority of patients were abstinent at that point, suggesting that, like the rest of the sample, patients with ASPD generally had a good outcome.
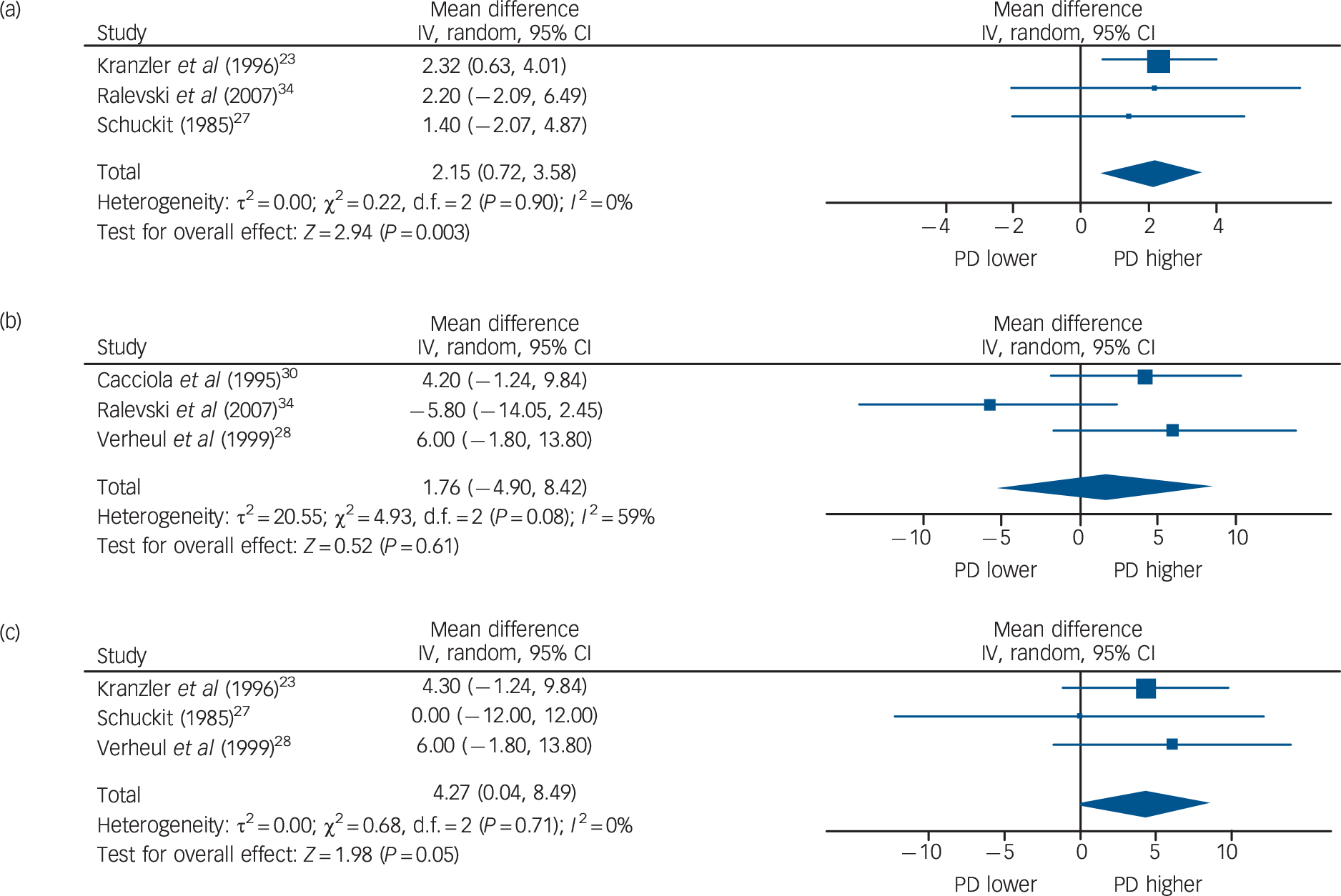
Fig. 2 Association between personality disorder status (PD) and primary alcohol outcomes: (a) drinks per drinking day; (b) percentage days heavy drinking; (c) percentage days drinking. For Ralevski et al comparison is between ASPD and no ASPD; Cacciola et al includes results from participants with primary cocaine dependence. ASPD, antisocial personality disorder.
Percentage of days drinking
As was the case for quantity of alcohol consumed, the percentage of drinking days (PDD) was not reported consistently, although the majority of papers found no association between personality disorder and PDD. In all, seven studies reported on the number or percentage of drinking days in the follow-up period. Schuckit found that patients with primary ASPD consumed alcohol on 191 days (s.d. = 141) in the previous year compared with 170 days (s.d. = 138) for patients with primary alcoholism, a non-significant difference. Reference Schuckit27 Kranzler et al reported that both men and women with ASPD had more drinking days in 3 years of follow-up (202 days v. 157 days for men with and without ASPD respectively and 168 days v. 109 days for women). Reference Kranzler, Del Boca and Rounsaville23 However, this became non-significant after adjusting the model for confounders. Similarly, BPD, ASPD and personality disorder were not associated with higher PDD over a 12-month period irrespective of treatment population. Reference Powell, Penick, Nickel, Liskow, Riesenmy and Campion25,Reference Nace, Saxon and Shore32,Reference Nordholm and Nielsen40 In contrast to these studies Hunter-Reel et al reported a higher PDD in patients with cluster C personality disorder (but not other personality disorders) over a 6-month follow-up. Reference Hunter-Reel, Epstein, McCrady and Eddie37 However, analyses presented in this study were severely limited by low numbers of participants with each type of personality disorder. One further study also reported a higher PDD among people with ASPD (21.7%, s.d. = 34.0) compared with those without ASPD (15.7%, s.d. = 28.0) although this difference was not statistically significant. Reference Verheul, Van Den Brink, Koeter and Hartgers28 As shown in Fig. 2, three of the above studies (n = 960) could be meta-analysed, Reference Kranzler, Del Boca and Rounsaville23,Reference Schuckit27,Reference Verheul, Van Den Brink, Koeter and Hartgers28 all of which compared participants with and without ASPD. There was no heterogeneity in outcomes across studies (I 2 = 0%). The PDD was estimated to be slightly higher in people with ASPD compared with those without that disorder (mean difference 4.27%, 95% CI 0.04–8.49).
Percentage of days with heavy drinking
Five studies reported on the percentage of heavy drinking days (PHDD) during follow-up, four of which showed similar improvement for patients with personality disorder compared with those without personality disorder. Verheul et al reported that participants with ASPD had higher PHDD (defined as at least five drinks) at baseline (64.7%, s.d. = 42.7) than the non-ASPD group (55.7%, s.d. = 36.3). Reference Verheul, Van Den Brink, Koeter and Hartgers28 At follow-up the ASPD group continued to have a higher PHDD (21.7%, s.d. = 34.0) than the non-ASPD group (15.7%, s.d. = 28.0) but the overall improvement was similar across both groups. Cacciola et al reported on PHDD (defined as drinking to intoxication) during follow-up over 7 months of treatment in a mixed sample of men with alcohol and/or cocaine dependency. Reference Cacciola, Alterman, Rutherford and Snider30 In this study participants with childhood- or adult-onset ASPD drank to intoxication more often at baseline (35.1% for those with childhood-onset and 37.8% for those with adult-onset disorder) than those without ASPD (20.7%). However, at follow-up the frequency of drinking to intoxication was 10.7% for the ASPD group and 6.5% for the non-ASPD group, suggesting that similar improvement was shown by both groups. A similar pattern of findings was reported by Nordholm & Nielsen in a study of people attending out-patient alcohol treatment in Denmark. Reference Nordholm and Nielsen40 In this study PHDD (defined as more than three drinks per day) was 44.0% for those without personality disorder and 50.7% for those with personality disorder at baseline and 19.3% v. 23.0% respectively at follow-up, again implying a similar improvement regardless of personality disorder.
Ralevski et al reported that the PHDD at baseline (defined as days with five or more standard drinks) for participants with ASPD (44.7%, s.d. = 40.3) was similar to that of the remainder of the sample (45.0%, s.d. = 39.0). Reference Ralevski, Ball, Nich, Limoncelli and Petrakis34 At baseline PHDD also did not differ according to whether BPD was present. At follow-up the PHDD was 14.3% (s.d. = 35.7) for those without ASPD and 8.5% (s.d. = 23.7) for those with the disorder. However, as the group of patients without ASPD also included some people with BPD, these findings are difficult to interpret. Conversely, in the study by Rolland et al, people with BPD had a significantly higher PHDD (defined as an intake of at least 50 g of alcohol) at follow-up (74.3%, s.d. = 25.3) in comparison with those without that disorder (41.7%, s.d. = 33.3), although differences in drinking patterns between the two groups at baseline were not clearly reported. Reference Rolland, Valin, Langlois, Auffret, Gautier and Deheul33 Three of the above studies, Reference Verheul, Van Den Brink, Koeter and Hartgers28,Reference Cacciola, Alterman, Rutherford and Snider30,Reference Ralevski, Ball, Nich, Limoncelli and Petrakis34 comprising 758 participants, reported data on the difference between ASPD and non-ASPD groups in a form that could be meta-analysed (Fig. 2). There was some variation within those studies in how heavy drinking was defined, and moderately high heterogeneity was present (I 2 = 67%). There was no significant difference in PHDD between those with and without ASPD during follow-up (mean difference 1.76%, 95% CI −4.90 to 8.42).
Secondary outcomes
Retention in treatment
Eight studies reported on the odds of treatment retention for people with personality disorder compared with those without such disorder. Outcomes showed moderately high heterogeneity (I 2 = 57%) so random effects meta-analysis was conducted. The pooled estimate of the odds of treatment retention was 0.35 (95% CI 0.18–0.69), indicating that participants with personality disorder were more likely to withdraw before treatment completion (Fig. 3). Two further studies assessed the mean number of days in treatment, with one study reporting that people with ASPD had fewer days in treatment, Reference Verheul, Van Den Brink, Koeter and Hartgers28 and one reporting no difference between patients with ASPD, BPD or neither personality disorder. Reference Ralevski, Ball, Nich, Limoncelli and Petrakis34

Fig. 3 Association between personality disorder status (PD) and treatment retention.
Quality of evidence and risk of bias
Table 2 outlines the quality and risks of bias across studies for each primary and secondary outcome, using a GRADE approach. Reference Oxman and Group45 It is notable that although the studies included in the systematic review comprised 4861 participants in total, meta-analyses of the primary outcomes stipulated in the review protocol comprised no more than three studies per outcome. This was due to the variable (but mainly poor) quality of statistical reporting and the diversity of alcohol outcomes employed in the studies selected. A number of studies did not report statistics in sufficient detail to allow calculation of an estimate of effect sizes and their variance, for example by reporting the mean of an outcome variable in the study sample but not its standard deviation. All included studies were of low or very low quality according to their scores on the Newcastle-Ottawa Scale. The overall quality of the evidence was very low, suggesting one high-quality study could significantly alter the findings of this review (see online Table DS1). The handling of missing data is a further issue with potential to bias the findings of individual studies. As noted, patients with personality disorders were more likely to withdraw from treatment, but in most cases studies reported findings for study completers. Few studies adopted robust statistical approaches to minimise bias arising from missing data. Therefore the findings reported in this review largely apply to individuals who were retained in follow-up, and they may not be generalisable to patients leaving the studies.
Table 2 Summary of quality of evidence for individual outcomes: personality disorder v. no personality disorder

| Outcome | Total participants, n |
Unadjusted alcohol outcomes at follow-up | Quality of evidence a |
Comments b |
|---|---|---|---|---|
| Primary outcomes | ||||
| Time to relapse | 809 | Personality disorder was associated with shorter time to relapse in 3/4 studies |
Very low | Incomplete reporting in some studies. Difficult to quantify magnitude of any effect |
| Percentage of days drinking |
1930 | PDD slightly higher in participants with ASPD v. those without (mean difference 4.27%, 95% CI 0.04 to 8.49) |
Very low | Incomplete reporting in some studies but good consistency across studies; most studies reported findings only for completers group; only 3 studies meta-analysed |
| Percentage of days with heavy drinking |
1394 | No significant difference in PHDD between participants with and without ASPD during follow up (mean difference 1.76%, 95% CI −4.90 to 8.42). |
Very low | Incomplete reporting in some studies; most studies reported findings only for completers group; only 3 studies meta-analysed |
| Alcohol consumption: drinks per drinking day |
1285 | Participants with personality disorder had higher DDD at follow-up (mean difference in DDD 2.15, 95% CI 0.72 to 3.58) |
Very low | Incomplete reporting; lack of agreement between studies. Most studies reported findings only for completers group; only 3 studies meta-analysed |
| Other outcomes | ||||
| Treatment retention | 474 | Personality disorder was associated with lower odds of treatment retention (OR = 0.35,95% CI 0.15 to 0.69) |
Low | Modest consistency between studies |
| Alcohol-related psychosocial impairment |
1417 | Personality disorder was associated with more impairment at baseline but no difference in the amount of improvement during treatment |
Very low | Moderate consistency across studies in spite of variable outcome measures used |
ASPD, antisocial personality disorder; DDD, drinks per drinking day; PDD, percentage of days drinking; PHDD, percentage of heavy drinking days.
a. See guidelines issued by the GRADE Working Group, Reference Guyatt, Oxman, Vist, Kunz, Falck-Ytter and Alonso-Coello21 also accessible at www.clinicalevidence.bmj.com.
b. For all outcomes the evidence presented was largely based on observational data. Baseline data were highly variable and poor quality. In most studies comparisons of personality disorder v. non-disorder subgroups were conducted on those completing the study, with no robust procedures to account for participants who dropped out. Findings also were largely not adjusted for potential confounding variables.
Discussion
Personality disorders are a common coexisting problem among patients presenting for treatment of an AUD. In our review up to two of every three patients had a comorbid personality disorder. Understanding the association between personality disorder and the outcome of treatment for an AUD therefore seems important. Although some evidence suggested that people with personality disorder were more impaired at the point of entry into treatment, with treatment they generally showed a similar amount of improvement to that of patients without personality disorder, assuming they remained in treatment (and their data were therefore analysed). This was the case both for specific alcohol-related outcomes and generic measures of psychosocial functioning (see online supplement DS1). In fact, in some areas improvements from baseline were at least as great as in those without personality disorders. This may be related to poorer baseline measures and subsequently greater capacity for gain with successful alcohol treatment. A standard difficulty with research examining personality disorder in mental state disorder is the stability of the personality disorder diagnosis over time with the treatment of the mental state disorder. This difficulty is well described for internalising disorders. Reference Ferro, Klein, Schwartz, Kasch and Leader46 This systematic review identifies similar problems existing for externalising disorders such as AUD. Although the short time frame may be considered problematic, research examining change in alcohol use in patients with personality disorder suggest much of the change is early, Reference Foulds, Mulder, Newton-Howes, Adamson, Boden and Sellman47 albeit sustained positive change is most clinically relevant. There was, however, some evidence that people with a personality disorder are less likely to complete treatment, an important proxy marker for longer-term success. Reference Newton-Howes and Stanley48 This suggests that modifications to treatment interventions aimed at retaining patients with personality disorder in treatment might be worthwhile. Evidence-based interventions that improve retention in addictions treatment in general, Reference Dutra, Stathopoulou, Basden, Leyro, Powers and Otto49 and specifically in individuals with personality disorder, Reference Tyrer50 are likely to add value to overall outcome.
Frustratingly, efforts to synthesise data identified in this review were hampered by several key methodological limitations of the included papers. First, the overall quality of data reporting was poor; further, the quality of evidence across studies for each of the primary outcomes was similarly poor, partly because evidence was largely based on observational data. Marked variation in the alcohol outcomes reported by different studies meant that each meta-analysis included only a few studies. Finally, no attempt was made to meta-analyse the change in alcohol consumption patterns from baseline to study completion. This was because some studies that reported these measures adequately for the whole sample did not give a breakdown according to personality disorder, whereas some studies included in the meta-analyses presented in Fig. 2 did not adequately report baseline data. For these reasons we are cautious about suggesting that our findings truly represent the relationship between AUD outcomes and personality disorder in general, or for specific personality disorder clusters or subtypes. Reference Balshem, Helfand, Schunemann, Oxman, Kunz and Brozek51 Personality disorders are a heterogeneous group in terms of patterns of behaviour, cognition and subjective distress. We have followed the general personality disorder approach in line with the likely changes to the ICD, Reference Tyrer, Crawford, Mulder, Blashfield, Farnam and Fossati52 as this increases the power of our findings and is forward-facing, although these concerns remain. This is despite this being the most comprehensive review of this literature to date.
Although personality disorders are highly prevalent in people with alcoholism, and are an important prognostic indicator for mental disorders in general, Reference Tyrer, Mulder, Crawford, Newton-Howes, Simonsen and Ndetei1,Reference Newton-Howes, Tyrer, Johnson, Mulder, Kool and Dekker4,Reference Newton-Howes, Tyrer, North and Yang53 few previous reviews have attempted to investigate the association between personality disorder and treatment outcome in AUD. However, in a review of prognostic indicators in alcoholism more generally, Adamson et al found limited evidence that personality disorder is a predictor of altered treatment outcomes. Reference Adamson, Sellman and Frampton54 It is also noteworthy that some major clinical trials in the alcohol field, such as Project MATCH and COMBINE, Reference Allen, Mattson, Miller, Tonigan, Connors and Rychtarik55,Reference Anton, O'Malley, Ciraulo, Cisler, Couper and Donovan56 are absent from the set of studies included in our review. In the case of the COMBINE study this may be because Structured Clinical Interview for DSM Axis II Disorders modules were not part of the baseline assessment. 57 For Project MATCH, the study presented detailed data on ASPD × treatment interaction effects but without apparent consideration of any main effects of ASPD on alcohol outcomes. Reference Allen, Anton, Babor and Carbonari58 This suggests the opportunity to investigate the prognostic significance of personality disorder may not have been fully exploited in either of these large and important studies. It is possible such analyses could still significantly add to our understanding of the association between personality disorder and AUD.
Study limitations
The conclusions of this review must be viewed as tentative because of a number of limitations. The included studies were mainly small to medium in size and the quality of evidence was low for reasons already discussed. Statistical reporting was generally poor. Furthermore, our inferences about the association between personality disorder and treatment outcome are largely based on unadjusted observational data for participants who were retained in treatment. No study used modern statistical approaches for handling missing data, and the higher withdrawal rates among participants with personality disorder meant that analysing only the completer group is likely to have introduced bias. It is also likely that the effect of personality disorder on alcohol treatment outcomes is confounded by other covariates such as age, gender, severity of alcohol problems and other psychopathological disorder at baseline. However, few studies presented adjusted outcomes. Therefore future studies investigating this area should carefully consider the role of these and other covariates. It is also possible that blinding to status could have influenced outcome, as clinicians can have a bias towards patients with personality disorder; Reference Newton-Howes, Weaver and Tyrer59 however, post hoc sensitivity analysis for this was not possible as no study provided information on blinded follow-up assessment and baseline personality status.
Future research
The findings from this review also speak to an urgent need to achieve better harmonisation of outcomes across studies in the alcohol field. In other areas of psychiatry such as mood disorders there tends to be much less variability in outcome reporting. For example, in a recent review of mood outcomes among people with AUD, Reference Foulds, Adamson, Boden, Williman and Mulder60 we reported that the majority of studies used the Hamilton Rating Scale for Depression (HRSD). Thus, in spite of concerns about the validity of scales such as the HRSD, Reference Bagby, Ryder, Schuller and Marshall61 consistent use at least makes quantitative synthesis of data across studies straightforward. Given that results from individual studies are often unreliable, consensus guidelines on the reporting of alcohol clinical trials are needed in order to help pool evidence from multiple studies.
A further development likely to influence this area is the rapid evolution in personality disorder classification, with a shift towards a more dimensional approach. Reference Tyrer, Crawford, Mulder, Blashfield, Farnam and Fossati52 This shift will entail a new era of studies investigating the association between dimensional personality domains and treatment outcomes in alcoholism and other substance use disorders. The new era presents a much-needed opportunity to improve the quality of evidence in this area.







eLetters
No eLetters have been published for this article.