Stroke is the second leading cause of death in Taiwan. In 2005, there were approximately 520 000 patients with cerebrovascular disease and the medical cost of this disease exceeded 12 billion New Taiwan dollars(1). Many patients surviving cerebrovascular disease were left with long-term mental and physical disability.
The incidence, recurrence and mortality of stroke and the stroke-related social burden can be decreased dramatically by controlling traditional risk factors such as hypertension, obesity, smoking and physical inactivity(Reference Straus, Majumdar and McAlister2). A previous study indicated that hypertension was strongly related to stroke and suggested that population-wide lowering of blood pressure has the potential to bring large reductions in stroke occurrence(3). In order to prevent cerebrovascular diseases, an intervention on lifestyle modification was suggested(Reference Goldstein, Adams and Alberts4). This meant that we should therefore treat aggressively risk factors for stroke in healthy subjects in the community.
However, most studies performed to investigate how to prevent stroke incidence or recurrence have been prospective or randomized clinical trials in which antihypertensive drugs were used(Reference Wang, Staessen, Franklin, Fagard and Gueyffier5, Reference Li, Engstrom, Hedblad, Berglund and Janzon6). Only a few studies have employed nutrition health education programmes to explore the primary prevention of stroke(Reference Fortmann and Varady7, 8). Regular reinforcement and repeated health nutrition education may help to encourage a healthy lifestyle but data on the effectiveness of this method are limited. Therefore, the purpose of the current study was to evaluate the intervention effect on blood pressure reduction of a family-based nutrition health education programme among community-dwelling hypertensive patients and pre-hypertensive subjects without taking antihypertensive drugs.
Methods
Study participants
This was a community-based prospective study. The study population consisted of all adults over 30 years of age living in Wen Shan and Shi Lin district as the coverage area of Wan Fang Hospital (WFH) and Shin Kong Wu Ho-Su Memorial Hospital (SKH), respectively. Sampling frame of the study was a stratified, multistage, clustering probability design based on the household registration provided by the Ministry of Interior in Taiwan (2002–2003). The primary sampling unit was villages of Wen Shan and Shi Lin districts in Taipei. The eligible villages were selected by geographic proximity, such as the degree of traffic convenience and the availability of hospital resources of WFH and SKH. Non-intervention and intervention villages were next to each other. The secondary sampling unit was the neighbourhood, and the basic sampling unit was the household. The study population was sampled according to the stratified structure of administrative records and the probability proportional to size method was used for sampling. Residents from villages with the intervention were classed as the intervention group, and those from the villages without the intervention were classed as the non-intervention group. In order to avoid contamination of health education, all participants did not know which group they belonged to. A survey was conducted from November 2003 to June 2004 (Fig. 1). After a telephone interview, 1511 subjects participated in the physical examination at baseline but only 1015 participants completed physical examinations at baseline and 6-month follow-up. After excluding subjects with normal blood pressure and subjects taking antihypertensive drugs, there were 390 participants included in the study: 208 pre-hypertensive and eighty-five hypertensive subjects in the intervention group; and sixty pre-hypertensive and thirty-seven hypertensive subjects in the non-intervention group. The study was approved by the institutional review board for human subjects of Taipei Medical University, Taipei, Taiwan and each subject provided written informed consent.

Fig. 1 Flow chart of participants through the study: family-based nutrition health education programme among community residents in Taiwan, November 2003 to June 2004 (BP, blood pressure)
Data collection
A standardized structured questionnaire including a personal medical history, family history of diseases, dietary habits, smoking and drinking status, and questions related to stroke knowledge, was completed by well-trained interviewers to collect study information. Repeated blood pressure was measured by a validated oscillometric automated digital blood pressure device (OMRON HEM-757; Omron Matsusaka Co. Ltd, Japan) after examinees had rested for at least 5 min. If the blood pressure reading between two measurements differed by more than 10 mmHg, an additional blood pressure measurement was carried out. The average of blood pressure was calculated from the two nearest blood pressure readings. Height, weight, waist and hip circumferences, total cholesterol, TAG, HDL cholesterol, LDL cholesterol and glucose were measured at each physical examination. BMI was defined as the individual’s body weight (kg) divided by the square of their height (m2). Waist:hip ratio (WHR) was computed as waist circumference divided by hip circumference. Subjects were categorized as physically active or physically inactive according to the frequency of exercise, which was defined as at least 20 min each time. Those who exercised at least once or twice weekly were grouped as physically active, others were considered as physically inactive. Study subjects who consumed at least one serving of fruit or vegetables every day were recognized as having habitual fruit or vegetable consumption; others were without the habit of fruit or vegetable consumption.
All subjects were requested to fast overnight for more than 8 h before blood collection. Blood was drawn and centrifuged within 2 h at room temperature. Serum, plasma and white blood cells (buffey coat) were collected and stored at −70°C until use. Serum was taken for analysing fasting total cholesterol, TAG, HDL cholesterol, glucose and uric acid by colorimetry in an automatic analyser (UniCel DXC 800; Beckman Coulter, Fullerton, CA, USA). LDL cholesterol was calculated by the Friedewald formula.
Study subjects with average systolic blood pressure (SBP) ≥140 mmHg or average diastolic blood pressure (DBP) ≥90 mmHg or those who had taken antihypertensive drugs were considered as hypertensive subjects. Individuals with average SBP between 120 and 139 mmHg or average DBP between 80 and 89 mmHg were defined as pre-hypertensive subjects(Reference Chobanian, Bakris and Black9).
Family-based nutrition health education programme
The intervention subjects received a family-based nutrition health education programme from a well-trained education nurse. All family members were educated to modify lifestyle-related risk factors of stroke, such as low-fat food or cooking methods, when they participated in a health examination in WFH or SKH. In the present study, lifestyle-related risk factors of stroke included heavy body weight, physical inactivity, smoking, dietary fat and alcohol intake. Above all, diet and nutrition were emphasized in the education programme. The advisors focused on improving nutritional knowledge on topics such as trying to switch from whole milk to low- or zero-fat milk, to use vegetable oil for cooking, or to change cooking methods from frying to steaming. When an unhealthy diet of family members was identified, information was given and the well-trained education nurse intended to increase motivation of these family members to modify or change their unfavourable dietary habits. Standardization of the research methods and procedures across the communities was made to make sure all data could be pooled for future analyses. In addition, a website (www.strokecenter.org.tw) designed by our team and including all materials of our health education programme was also provided to all intervention subjects to maintain the effects of the nutrition health education. Furthermore, consultation by telephone was always available on weekdays. In contrast to intervention subjects, non-intervention subjects were able to obtain a general education sheet which was always available in clinics during the routine physical examination in the study. In order to evaluate the intervention effects of family-based nutrition health education on decreasing blood pressure, another physical examination at 6 months of follow-up was also carried out.
Statistical methods
Continuous data are described by means and standard deviations and were analysed by Student’s t test. Categorical data are characterized as frequency and percentage and were compared by the continuous correction χ 2 test or Fisher’s exact test, as appropriate. The paired t test was used to compare differences in blood pressure between baseline and the 6-month follow-up visit among intervention and non-intervention subjects. Statistical analysis was carried out using the Statistical Analysis Systems statistical software package version 8·0 (SAS Institute, Cary, NC, USA). Statistical significance was set at P < 0·05.
Results
Descriptive data
In order to avoid confounding effects of stroke-related risk factors, we examined the differences between these factors in the intervention and non-intervention group at baseline, as shown in Table 1. There were no significant differences between the two groups in terms of age, sex, education, baseline blood pressure (SBP and DBP), BMI, WHR, blood lipid profiles (cholesterol, TAG), marital status, hypertension status, physical activity, and fruit and vegetable consumption.
Table 1 Baseline characteristics of pre-hypertensive and hypertensive subjects without taking antihypertensive drugs among intervention and non-intervention groups: family-based nutrition health education programme among community residents in Taiwan, November 2003 to June 2004

SBP, systolic blood pressure; DBP, diastolic blood pressure; WHR, waist:hip ratio.
Changes in blood pressure during the intervention
As shown in Table 2, at the 6-month follow-up, a significant reduction in SBP of 2·0 and 5·9 mmHg was observed among subjects with pre-hypertension and hypertension, respectively, in the intervention group. However, there were no significant decreases of SBP in non-intervention subjects. In addition, the decrease in SBP among hypertensive subjects in the intervention group was fourfold greater than that in the non-intervention group. Furthermore, there was also a significant decrease in DBP among hypertensive subjects in both groups.
Table 2 Trend of blood pressure among pre-hypertensive and hypertensive subjects without taking antihypertensive drugs: family-based nutrition health education programme among community residents in Taiwan, November 2003 to June 2004
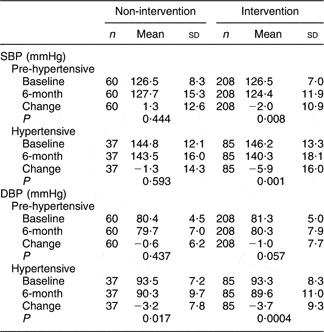
SBP, systolic blood pressure; DBP, diastolic blood pressure.
Differences in blood pressure during the intervention by stroke-related risk factors
Our data revealed that males, females and those aged ≤55 years had significant decreases in SBP among the intervention group. In addition, pre-hypertensive and hypertensive subjects with reductions in total cholesterol, LDL cholesterol and WHR, and with the habit of fruit and vegetable consumption also showed a significant decrease in SBP (Table 3). The greatest reduction of SBP (a decrease of more than 7·0 mmHg) was observed among hypertensive subjects whose total cholesterol, LDL cholesterol and waist decreased. Table 4 shows that DBP was reduced to normal value in hypertensive patients after modifying stroke-related risk factors. Moreover, study subjects whose total cholesterol, LDL cholesterol and waist decreased also had a prominent reduction of DBP (decrease of more than 4·3 mmHg).
Table 3 Difference in systolic blood pressure between baseline and 6-month follow-up visit among pre-hypertensive and hypertensive subjects without taking antihypertensive drugs in the intervention group, by stroke-related risk factors: family-based nutrition health education programme among community residents in Taiwan, November 2003 to June 2004

Table 4 Difference in diastolic blood pressure between baseline and 6-month follow-up visit among pre-hypertensive and hypertensive subjects without taking antihypertensive drugs in the intervention group, by stroke-related risk factors: family-based nutrition health education programme among community residents in Taiwan, November 2003 to June 2004

Discussion
The purpose of the current family-based nutrition health education programme was to modify risk factors of stroke, especially blood lipid profiles and waist, by changing the dietary habits of all family members to decrease blood pressure in the intervention group. The intervention used a health nutritional education approach within the family and focused specifically on diet and nutrition, physical activity, cigarette smoking and alcohol drinking. In addition, in the intervention group, the wives who usually cooked for the family were educated to adopt healthy cooking habits.
Our study showed that, 6 months after the baseline physical examination, there was a significant decrease in SBP among pre-hypertensive and hypertensive subjects after receiving the family-based nutrition health education intervention. In addition, a similar effect on DBP was observed among hypertensive subjects in both groups at the 6-month follow-up. The study provides strong evidence that lowering of blood pressure among hypertensive and pre-hypertensive subjects through a family-based nutrition health education programme is possible in patients without taking antihypertensive drugs. Our data also show that younger subjects had higher motivation to pursue health and had significant lowering of SBP and DBP in the intervention group. In addition, significantly favourable changes in blood lipid profiles, dietary behaviour and indices of body weight were found among study subjects during the intervention. Through improvement of the study subjects’ knowledge of stroke-related risk factors including blood lipid profiles, fruit and vegetable consumption, WHR and waist, significant decreases in SBP and DBP were observed in the study, especially for hypertensive subjects.
The PREMIER clinical trial also showed that pre-hypertensive and stage 1 hypertensive individuals can make multiple lifestyle changes that lower both SBP and DBP for up to 6 months(8). However, that intervention was provided in an individual session. Compared with the PREMIER clinical trial, the intervention strategy in the present study focused on a family-based nutrition health education programme. The reason to adopt a family-based nutrition health education programme in our study was that the person who is usually in charge of cooking for a family and makes choices of foods and cooking oil is the housewife. In addition, the cooking habit of the study subjects, mean age over 50 years, was Chinese type rather than Western type in our study. Compared with Western-type diet, the Chinese-type diet is considered to have less oil and more vegetables. Therefore, it is very important to stress that the intervention effect of nutrition health education on blood pressure control occurred in subjects with Chinese-type diet. Our study shows that study subjects with reductions of total cholesterol, LDL cholesterol and waist also lowered their SBP by more than 7.0 mmHg after the 6-month intervention. A systematic review of antihypertensive trials confirmed that subjects who lowered their SBP by 5–6 mmHg would rapidly achieve 42 % stroke risk reduction within 3 years(Reference Straus, Majumdar and McAlister2). Thus, in our study, the study subjects are expected to reduce stroke risk more than 42 % after the 6-month intervention of family-based nutrition health education programme.
The beneficial effect of regular physical activity on blood pressure is widely recognized and documented(Reference Pereira, Folsom, McGovern, Carpenter, Arnett, Liao, Szklo and Hutchinson10, Reference Hu, Barengo, Tuomilehto, Lakka, Nissinen and Jousilahti11). In the present study, however, a significantly decreasing effect on blood pressure was found in hypertensive subjects with or without habitual exercise activity, showing a null effect of physical activity on blood pressure in both groups. There are some possible reasons that might explain this observation. First, among thirty-four hypertensive subjects without the habit of exercise activity, 50·0 % and 88·2 % of them, respectively, consumed at least one serving of vegetables and fruits daily. We think that people who have good habits of consuming vegetables and fruits would also have healthy behaviour. Therefore, the null effect of physical activity on blood pressure might be found in our study. However, significant decrease of SBP and DBP would then also be observed in our study for study subjects with habits of fruit and vegetable consumption. Second, although the definition of physical activity in our study was to exercise for at least 20 min each time and at least once weekly, the null effect of physical activity on blood pressure observed might be due to the lack of more precise measurements of exercise, such as the degree and types of exercise.
To our knowledge, ours is the first study to provide a significant lowering effect on blood pressure through a family-based nutrition health education programme in Asia. Previous studies reported that SBP continued to decline but DBP stopped declining through treatment of hypertension(Reference Vartiainen, Jousilahti, Alfthan, Sundvall, Pietinen and Puska12, Reference van Leer, Seidell and Kromhout13). The present study also showed significant effects on lowering SBP in the intervention group not only in pre-hypertensive subjects but also in hypertensive subjects through a family-based nutrition health education programme. However, DBP was decreased significantly in both intervention and non-intervention groups among hypertensive subjects, showing a null effect of the intervention on DBP. There might be several possible explanations. First, the hypertensive participants might have strong motivation to adopt a healthy lifestyle once they got the report of their abnormal blood pressure through physical examination. Second, there were 17·5 % and 9·9 % of subjects whose age was greater than 65 years in the non-intervention and intervention group, respectively (P < 0·05). An interesting finding in our study was a significant decreasing effect on DBP among elderly subjects with lifestyle changes in the non-intervention group, which could decrease the effect of the intervention on blood pressure. However, a further study will be needed to elucidate this.
The Eastern Stroke and Coronary Heart Disease Collaborative Project implied it would be possible to contribute to the reduction of stroke risk by lowering blood pressure through a family-based nutrition health education programme(3). A recent study showed that the effect of the health education programme on knowledge and warning signs of stroke decreased at 3 months of follow-up(Reference DeLemos, Atkinson, Croopnick, Wentworth and Akins14). However, the present study showed that a family-based nutrition health education programme on blood pressure lowering had significant effectiveness at 6-month follow-up. Our data also showed that hypertensive subjects, without taking antihypertensive drugs, could decrease their SBP to 140 mmHg approximately, and their DBP to less than 90 mmHg, through a family-based nutrition health education programme. Therefore, we proved that to give antihypertensive drugs should not be the only strategy for the treatment of hypertension.
Although significant reductions of SBP and DBP among the intervention group were shown in the present study, there were several limitations. First, this was an urban community study and the sample size was not big enough. The intervention effects obtained in the study might not be applicable to the general population especially for residents in rural areas. Second, this was only a 6-month follow-up study. These study subjects will need to be followed up in the future to examine the long-term effect of the family-based nutrition health education programme on blood pressure. Third, more details other than frequency should be added, such as indices of habit for physical activity and consumption of vegetables and fruits, to examine the association with reductions of SBP and DBP. Further study should be emphasized on the degree or the type of physical activity and the specific items of vegetables and fruits to evaluate their effects on reducing blood pressure.
Conclusions
In conclusion, the SBP and DBP of hypertensive subjects who did not take any antihypertensive drugs but received a family-based nutrition health education programme to improve the knowledge of stroke-related risk factors, such as decreases of total cholesterol, LDL cholesterol and waist, could be significantly lowered by more than 7·0 mmHg and 4·3 mmHg, respectively. The blood pressure of hypertensive subjects and their stroke risk could also be reduced by employing the same health education programme. This represents that education has played an important role in stroke prevention.
Acknowledgements
Competing interests: The authors declare that they have no competing interests.
Authors’ contributions: Y.-C.H. supervised data collection and analysis, and drafted the manuscript. C.-T.H. provided support during the development of the intervention and participated in revision of the manuscript. L.-M.L., W.-H.C. and H.-C.C. provided support during the development of the intervention. C.-H.B. contributed intellectual input into the main ideas of study design, data collection and analysis. C.-Y.Y., Y.-H.C. and F.-I.H. provided support in the design of the study and statistical consultant. H.-Y.C. and C.-Y.H. contributed intellectual input into the main ideas of study design and obtained financial support. All authors read and approved the final manuscript.
Acknowledgments: We thank Drs Ying-Chin Lin, Hsin-Hon Chen, Chin-I Chen, Chun-Ping Huang and Yu-Hsuan Han, Department of Neuroscience, Wan Fang Hospital, Taipei, Taiwan, who examined the physical examination results for study subjects. The study was supported by the Bureau of Health Promotion, Department of Health, Taipei, Taiwan (DOH92-HP-1113; DOH93-HP-1113; DOH94-HP-1113). Additional supports were received from a Topnotch Stroke Research Center grant, the Ministry of Education, and the Center of Excellence for Clinical Trial and Research in Stroke and TBI (DOH-TD-B-111-002).







