Malnutrition affects 195 million children under the age of 5 years (U5C) worldwide and is associated with increased risk of child morbidity and mortality( Reference Black, Allen and Bhutta 1 – Reference Rahman, Howlader and Masud 3 ). It accounted for nearly 97 million disability-adjusted life years among U5C in 2017, of which 98 % occurred in low- and middle-income countries( 4 ). Malnutrition limits cognitive and physical development, and reduces immune system function that can increase the risk of child mortality from infections, thereby extracting a high economic cost from individuals and developing economies( 5 , Reference Rice, Sacco and Hyder 6 ).
The determinants of malnutrition are complex and result from the interaction of several risk factors, including low birth weight, poor infant and young child feeding practices, frequent infections, and inadequate access to health care and water and sanitation( Reference Ahmed and Ahmed 7 – 9 ). There is global agreement that children have almost equal potential for growth in their early years and that sociodemographic factors such as low maternal education and household economic status influence growth disparities. Using data from 1970 to 2012 for 116 countries, Smith and Haddad found that nutrition-sensitive factors – which include access to safe water, sanitation, women’s education, gender equality, and the quantity and quality of food available – were key drivers of reductions in stunting. Complementary to nutrition-specific programmes and policies, further reductions in malnutrition will require increased investment in these priority areas( Reference Smith and Haddad 10 ).
Global efforts to reduce child malnutrition have progressed successfully with the setting of the global nutrition targets and the Sustainable Development Goals offering time-bound targets to reduce all forms of malnutrition. Bangladesh has set national nutrition targets aligned to the global nutrition targets 2025, to reduce the prevalence of stunting among U5C (current 36 % to 25 %), wasting (current 14 % to <8 %) and underweight (current 33 % to 20 %) by 2020( 11 , Reference Rahman and Chowdhury 12 ).
The Government of Bangladesh has prioritized and implemented interventions including supporting infant and young child feeding, micronutrient supplementation, food supplementation and other health interventions. There has also been focus on nutrition-sensitive interventions including education, water and sanitation, and social welfare( Reference Hasan, Magalhaes and Williams 13 ). Despite significant improvements in child malnutrition rates in Bangladesh, in 2011, an estimated 5·5 million U5C remained stunted, with 5 million underweight and 2·2 million wasted( 14 ). Although the annual average rate of reduction of malnutrition at the national level is high (approximately 4 % per year), the rate is comparatively low in districts such as Sylhet( Reference Hasan, Magalhaes and Williams 13 ). Thus, geographic distribution, inequalities in wealth distribution and education are likely to significantly affect achievement of malnutrition targets in the country and will have to be taken into account when implementing future policies. To address these challenges, the Ministry of Health and Family Welfare initiated the second Bangladesh National Plan of Action for Nutrition (NPAN2) 2016–2025, which outlines strategies to eradicate all forms of malnutrition( 15 ). This plan takes into consideration the limitations of capacity in government institutions that impede successful implementation of both nutrition-specific and nutrition-sensitive interventions and includes actions to enhance inter-sector collaboration and coordination, as well as strengthen multisector monitoring to track progress. A key strategy is the targeting of vulnerable people living in poor rural and urban areas and in remote locations.
Therefore, information on influences of socio-economic inequality in malnutrition would be useful in developing cost-effective interventions to implement the NPAN2. There is currently a gap in the literature of a comprehensive assessment of the burden of child malnutrition in Bangladesh, and few studies have appraised the socio-economic inequality in childhood malnutrition( Reference Huda, Hayes and El Arifeen 16 , Reference Pulok, Sabah and Enemark 17 ). Earlier studies focus on the inequality in childhood malnutrition for only one indicator or using relatively old data. The present study takes a more comprehensive approach and focuses on the inequality in childhood malnutrition in Bangladesh of multiple indicators using the latest data.
Therefore, with the aim of helping to identify entry points for action and develop strategic actions to inform the NPAN2, the objectives of the present study were fourfold: (i) to estimate the projected prevalence of childhood malnutrition up to the year 2030, to align with the timeline of the Sustainable Development Goals; (ii) to analyse the changes of wealth-based inequalities in child malnutrition over the years from 1996 to 2014; (iii) to explore the degree of contribution of socio-economic determinants to the observed inequalities in child malnutrition; and (iv) to assess the risk factors of malnutrition among U5C in Bangladesh.
Data and methods
Sources of data
The present study used data from Bangladesh Demographic and Health Surveys (BDHS) from 1996 to 2014, which are nationally representative cross-sectional household surveys. Additionally, the study incorporated data from other household surveys such as the Child and Mother Nutrition Survey (CMNS) and the Multiple Indicator Cluster Survey (MICS) for estimating forecasted trends of childhood malnutrition. For risk factor analysis, BDHS 2014 data were used. Details of the sample size and response rate for each survey are presented in the online supplementary material (Supplemental Table S1). Participants with missing information on anthropometrics and other covariates were excluded from the study (Supplemental Fig. S1).
Outcomes
The primary outcomes in the present study were stunting, wasting, underweight, severe stunting, severe wasting and severe underweight among U5C. Stunting, wasting and underweight were defined according to the WHO Child Growth Standards as height-for-age, weight-for-height and weight-for-age two standard deviations (–2 sd) lower than the median of the reference population, respectively. Similarly, children whose height-for-age, weight-for-height and weight-for-age was three standard deviations (–3 sd) lower than the median of the reference population were defined as severely stunted, severely wasted and severely underweight, respectively( 18 ).
Predictor variables
Covariates were considered based on previous literature and the availability of data( Reference Chowdhury, Rahman and Khan 19 – Reference Yisak, Gobena and Mesfin 26 ). The study included three levels of confounding variables: individual, household and community levels. The individual-level covariates included child’s age in months, gender, birth order, mother’s BMI, mother’s education and father’s education. Mother’s BMI was divided into three categories: normal (18·5–24·9 kg/m2), underweight (<18·5 kg/m2) and overweight/obese (≥25·0 kg/m2). The household-level covariates included religion (Muslim, non-Muslim) and socio-economic status (poorest, poorer, rich, richer, richest). Socio-economic status of households was measured based on household characteristics and ownership of assets using principal component analysis( Reference Rutstein and Johnson 27 ). Lastly, the community-level covariates included place of residence (urban or rural) and administrative region of residence (Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Rangpur, Sylhet).
Statistical analysis
The primary analysis involved descriptive statistics, which were presented as percentages with 95 % CI. A Bayesian linear regression analysis with non-informative prior, considering year as a covariate, was used to obtain projections of childhood malnutrition indicators up to the year 2030. The Markov chain Monte Carlo (MCMC) algorithm was used to obtain samples, using two chains, from the posterior prediction distribution of the parameter of interest. The posterior predictive distribution was used to obtain the estimates with 95 % credible intervals (CrI) up to the year 2030. The convergence of MCMC outputs was assessed through visual inspection of trace plots for all models. Additionally, the convergence of MCMC outputs was quantitatively confirmed using Gelman–Rubin diagnostic statistics. We performed sensitivity analysis for the projection of childhood malnutrition after excluding data from surveys other than the BDHS to determine whether inclusion of different types of survey data in the model change the trends and projections. For equity analysis, a regression-based slope index of inequality and relative index of inequality were used to assess the wealth-based absolute and relative inequality in different malnutrition statuses( Reference Barros and Victora 28 – Reference Regidor 30 ). The concentration curve and index were constructed to visualize the extent of wealth-based inequality in different malnutrition statuses( Reference Wagstaff, O’Donnell and Van Doorslaer 31 ). The decomposition of concentration index analysis was used to assess the contribution of various socio-economic factors in the observed wealth-based inequality in different child malnutrition indicators( Reference Wagstaff, O’Donnell and Van Doorslaer 31 ). Multilevel logistic regression models with random intercept at individual, household and community levels were used to identify risk factors for stunting, wasting and underweight among U5C in 2014. All analysis was adjusted for the complex probability sample design. Data analyses were performed using the statistical software package Stata version 14/MP and the JAGS (Just another Gibbs sampler) program.
Results
Prevalence of malnutrition in children under the age of 5 years
Table 1 presents the prevalence of malnutrition indicators among U5C in Bangladesh in 2014. In a total sample of 6939 children, the prevalence of stunting, wasting and underweight was 36·2 (95 % CI 34·4, 38·0) %, 14·3 (95 % CI 13·2, 15·5) % and 32·6 (95 % CI 30·7, 34·5) %, respectively. Furthermore, 11·4 (95 % CI 10·3, 12·7) % of children were severely stunted, 3·1 (95 % CI 2·5, 3·8) % were severely wasted and 7·7 (95 % CI 6·9, 8·6) % were severely underweight. Most of the malnutrition indicators were substantially higher among children whose mothers are underweight, whose mothers or fathers have no education level, who have a rural place of residence or are from the poorest household quintile.
Table 1 Prevalence of malnutrition among children under the age of 5 years in Bangladesh in 2014
Projection of child malnutrition
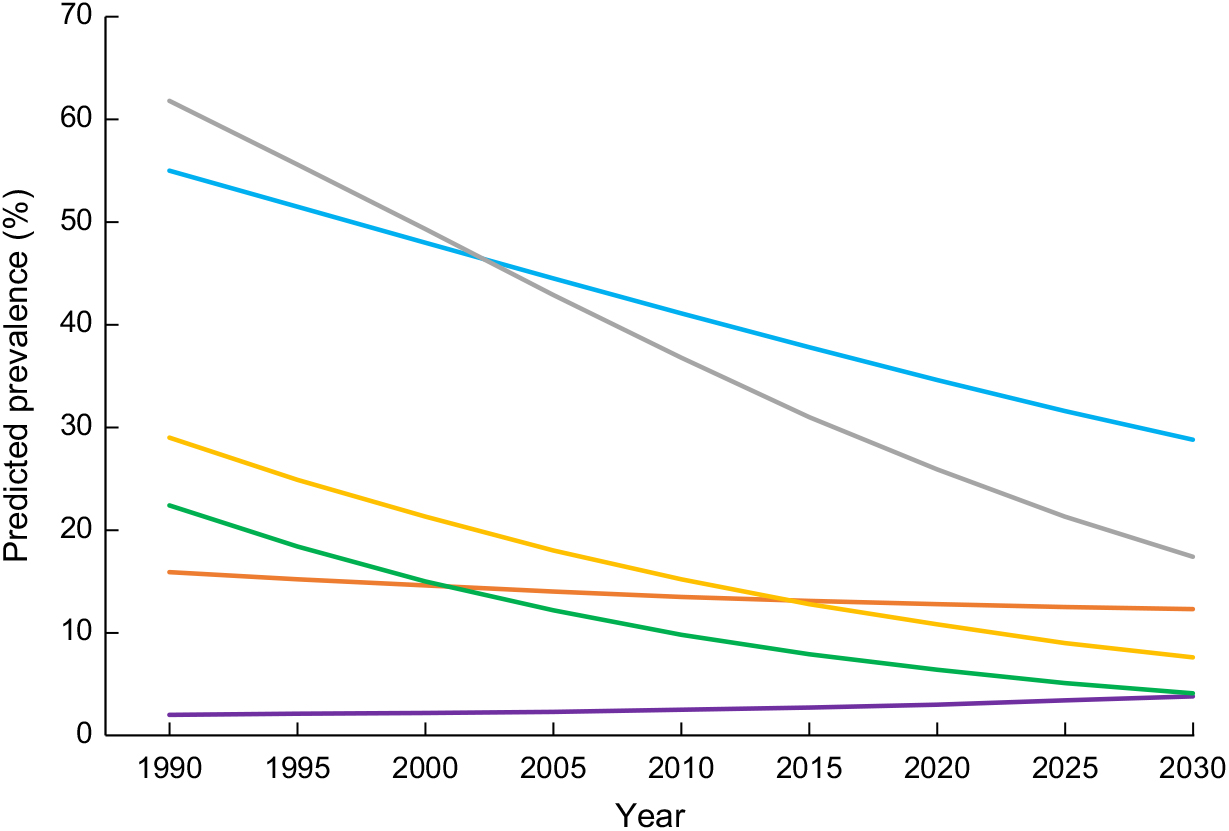
The trends and projections of the prevalence of different malnutrition indicators among U5C are presented in Fig. 1 and the online supplementary material (Supplemental Table S2 and Supplemental Figs S2–S4). If the current trends continue, the predicted prevalence of U5C who are underweight will decline by approximately three-quarters from 61·8 (95 % CrI 54·8, 69·3) % in 1990 to 17·4 (95 % CrI 11·6, 24·8) % in 2030. Similarly, the prevalence of stunting and wasting is projected to decline from 55·0 (95 % CrI 45·5, 63·3) % to 28·8 (95 % CrI 19·0, 40·0) %, and from 15·9 (95 % CrI 9·2, 24·8) % to 12·3 (95 % CrI 5·6, 23·2) % between 1990 and 2030, respectively, if recent trends continue. Although the prevalence of severe stunting and severe underweight is projected to decline significantly by four- to fivefold, severe wasting is projected to increase slightly between 1990 and 2030. The highest annual rate of reduction is observed in severe underweight and severe stunting categories (4·09 % and 3·28 %, respectively), and the lowest is in wasting (0·63 %). The only indicator shown to display a negative value of annual rate of reduction is severe wasting (–1·40 %). Sensitivity analysis of all the malnutrition indicators showed a narrower spread in prevalence rates in 2030 after excluding surveys other than the BDHS from the model (online supplementary material, Supplemental Fig. S5).

Fig. 1 Projected prevalence of malnutrition (![]() , stunting;
, stunting; ![]() , wasting;
, wasting; ![]() , underweight;
, underweight; ![]() , severe stunting;
, severe stunting; ![]() , severe wasting;
, severe wasting; ![]() , severe underweight) among children under the age of 5 years in Bangladesh, 1990–2030
, severe underweight) among children under the age of 5 years in Bangladesh, 1990–2030
Inequality in child malnutrition
The results of slope index of inequality, relative index of inequality and concentration index are presented in Table 2. In 2014, the slope index of inequality indicated that the prevalence of stunting, wasting and underweight was 34·3, 6·9 and 32·8 percentage points lower in the richest households, respectively, than the poorest households. Similarly, the proportion of severe stunting, severe wasting and severe underweight among U5C was substantially lower in the richest households than the poorest households. Pro-poor inequality had increased significantly for all malnutrition indicators during 1996 to 2014 (online supplementary material, Supplemental Figs S6–S11).
Table 2 Slope index of inequality, relative index of inequality and concentration index, by malnutrition status, among children under the age of 5 years in Bangladesh, 1996 and 2014
Decomposition analysis
The concentration index of stunting, wasting and being underweight was decomposed into various contribution indices of wealth-based inequalities and year-specific results are presented in Fig. 2. Contribution of all determinants for stunting and underweight was negative between 1996 and 2014, indicating that pro-poor inequality was explained by these variables. The contribution of household wealth index, father’s education and maternal BMI to inequality in stunting and underweight increased over time, whereas the contribution of household wealth index, father’s education and maternal BMI to inequality in wasting fluctuated over time. Contribution of household wealth index alone to absolute inequality increased for stunting (from 39 % to 58 %), wasting (from 65 % to 78 %) and underweight (from 50 % to 60 %) between 1996 and 2014. However, the contribution of mother’s education to pro-poor inequality in stunting and underweight decreased over time, with the lowest contribution in observed in 2014.
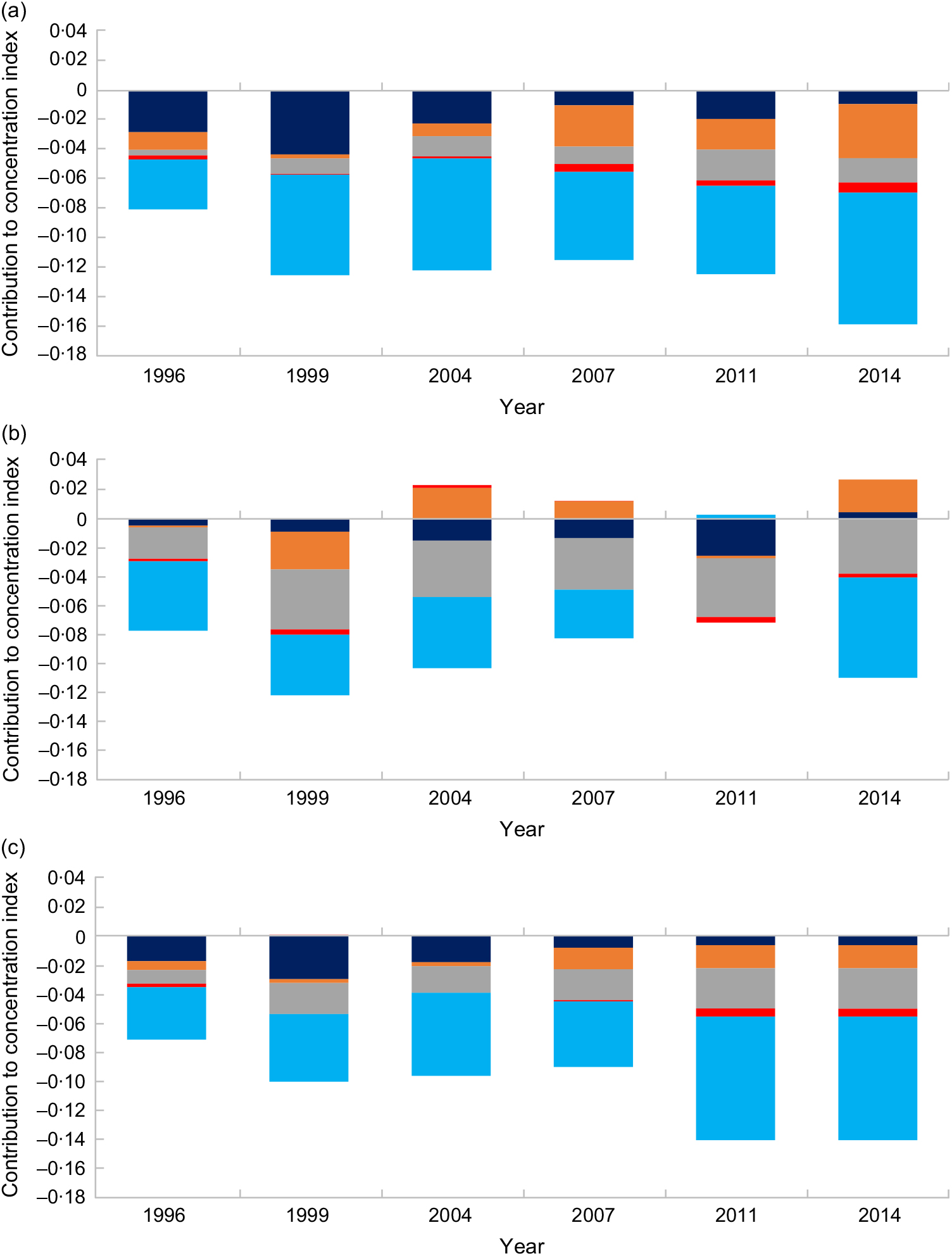
Fig. 2 Absolute contribution of wealth-based inequalities (![]() , mother’s education;
, mother’s education; ![]() , father’s education;
, father’s education; ![]() , mother’s BMI;
, mother’s BMI; ![]() , birth order;
, birth order; ![]() , wealth index) to concentration index of (a) stunting, (b) wasting and (c) underweight among children under the age of 5 years in Bangladesh, 1996–2014
, wealth index) to concentration index of (a) stunting, (b) wasting and (c) underweight among children under the age of 5 years in Bangladesh, 1996–2014
Risk factors for child malnutrition
The results of multilevel logistic regression models for stunting, wasting and underweight are presented in Table 3. Increasing age was associated with increased risk of stunting and being underweight, but decreased risk of wasting. The risk of stunting increased significantly by nearly sixfold in age group of 36–47 months (OR = 5·82; 95 % CI 4·47, 7·56), followed by 24–35 months (OR = 4·91; 95 % CI 3·80, 6·36) and 12–23 months (OR = 4·10; 95 % CI 3·22, 5·22). The risk of being underweight was significantly higher by up to threefold with increasing age group: 2·30 times in 12–23 months (95 % CI 1·86, 2·85), 3·21 times in 24–35 months (95 % CI 2·57, 4·01), 3·32 times in 36–47 months (95 % CI 2·64, 4·18) and 3·45 times in 48–59 months (95 % CI 2·74, 4·35). On the contrary, the risk of wasting was significantly lower in higher age groups compared with 0–11 months. The risk was lower in the age groups of 24–35 months (OR = 0·65; 95 % CI 0·51, 0·83) and 36–47 months (OR = 0·67; 95 % CI 0·53, 0·86).
Table 3 Determinants of malnutrition among children under the age of 5 years in Bangladesh, 2014
Gender was significant only in stunting, with female children having lower odds (OR = 0·87; 95 % CI 0·76, 0·98) compared with males. The adjusted and unadjusted multilevel models indicated that children with an underweight mother and children with no education level in the mother or father were associated with increased risk of stunting and being underweight by up to twofold. Household wealth quintile displayed an association in risk of stunting, wasting and being underweight, with increasing risk in the poorest wealth quintile (Table 3 and online supplementary material, Supplemental Table S3). Similar results were also observed for severe stunting, severe wasting and severe underweight models (Supplemental Tables S4 and S5). Birth order and religion did not display a significant association in risk of stunting, wasting and underweight.
Discussion
The present study assessed current and projected prevalence of malnutrition, the contributing determinants of inequalities to malnutrition status, and associated factors in U5C in Bangladesh using nationally representative data. Our findings suggest that, if the trends continue, the prevalence of malnutrition is projected to decrease significantly by nearly 2-fold and 3·5-fold for stunting and underweight, respectively, between 1996 and 2030, while the prevalence of wasting will decrease by one-quarter. Pro-poor inequality increased with time and the poorest quintile had more malnutrition as time progressed. During this time, the contribution of household wealth index increased inequity in child malnutrition, while mother’s education decreased inequity. The risk of malnutrition was significantly higher among children who were aged 12 months or greater, had a mother who was underweight, were from families with a low level of maternal or paternal education, were of rural residence and were from households with lower socio-economic status.
The latest nutrition data among U5C in Bangladesh indicate that stunting and underweight are major public health problems as per the WHO criteria, and wasting is at a borderline critical level( Reference De Onis and Blossner 32 ). Projections to 2025, based on current levels of decrease, show that the situation is only somewhat alleviated. A continued moderate level of stunting (projected 31·6 %; target 27·4 %) is indicated, with wasting (projected 12·5 %; target <5 %) remaining a serious public health problem( Reference Chowdhury, Bhuiya and Chowdhury 33 ). The greatest reduction is predicted to occur among stunting and severe underweight. The low rate of reduction that is foreseen for wasting possibly reflects insignificant differences in the rates of food shortage and disease over time. While access to essential primary health care including nutrition services has improved in Bangladesh( Reference Chowdhury, Bhuiya and Chowdhury 33 , 34 ), a greater focus on socio-economic determinants, especially pro-poor strategies for improving household income, and a greater focus on education are required to further accelerate improvements in nutrition status.
Wealth status was a key factor influencing child malnutrition. Children from the richest households have significantly lower risk of being malnourished compared with those from the poorest households, similarly to previous studies( Reference Chowdhury, Rahman and Khan 19 , Reference Khan, Turab and Khan 21 , Reference Siddiqi, Haque and Goni 22 ). The higher risk of malnutrition among poor households may be due to limited capacity to access essential health-care services, lack of potable water and adequate sanitation, poor housing facilities and nutritionally inadequate diets( Reference Chowdhury, Rahman and Khan 19 , Reference Khan, Turab and Khan 21 ). This has been understood by policy makers, hence the intensive focus and monitoring of multisectoral policies and programmes in the NPAN2.
We present the contribution of wealth-based inequalities in malnutrition indices which display an increasing pro-poor inequality over the years. Equality analysis found that households from lower wealth quintiles continue to be disproportionately affected by malnutrition among U5C than those from higher quintiles, displaying concordance with other studies( Reference Huda, Hayes and El Arifeen 16 , Reference Pulok, Sabah and Enemark 17 , Reference Novignon, Aboagye and Agyemang 35 , Reference Uthman 36 ). Similar to our study, Uthman( Reference Uthman 36 ) found that household wealth was the largest contributing factor to pro-poor inequality of malnutrition, followed by father’s education, in Nigeria. Household income is an important indicator for child nutrition as it influences food security, allocation of resources and selection of foods purchased. Here we present an interesting observation as our analysis found that the contribution of household wealth increased absolute inequality between 1996 and 2014 despite national decreases in the poverty headcount ratio from 57 % in 1992 to 32 % in 2010( Reference Jolliffe, Sharif and Gimenez 37 , Reference Das, Chisti and Malek 38 ). Our findings demonstrate that possibly due to the likely unequal distribution of national income growth, if the trends continue, malnutrition will still be prevalent by 2030 and be unequally distributed, being observed more among the poorest households.
Vollmer et al. in 2014 reported a very small to null association between increases in per capita gross domestic product and reductions in early childhood undernutrition in low- and middle-income countries, including Bangladesh( Reference Vollmer, Harttgen and Subramanyam 39 ). Specifically, no association was observed between increases in per capita gross domestic product and improved nutrition in the poorest household wealth quintile. Since wealth index, parental education and maternal BMI are the most closely associated risk factors, the findings of the present study highlight that malnutrition indices are most unsatisfactory within vulnerable areas. Further improvements in national prevalence rates of malnutrition are likely to be more effective through targeted nutrition interventions to poor households with one or more uneducated parent(s) and maternal underweight.
Having higher than primary level of education in the mother and father significantly reduced the risk of stunting and underweight. While the contribution of mother’s education decreased pro-poor inequality of stunting and underweight, its greatest contribution was in earlier years, with a steady decline in its relative contribution in recent years, with the lowest contribution being in 2014. Father’s education has a greater role in more recent years together with wealth index. This could be explained by the fact that the current net enrolment rate of primary-level education for girls is close to 100 % in Bangladesh( 40 , Reference Hasan, Soares Magalhaes and Williams 41 ) and when primary education for girls was lower in the early years, the contribution to malnutrition would have been greater than at present.
In our study, we found that the contribution of wealth quintile and father’s education to the inequality in malnutrition has increased over the past decades. Father’s education and household wealth have become relatively more important in recent years as, naturally, education would be expected to impact on household income generation. Bangladesh Bureau of Statistics indicated that the country’s net enrolment rate at the primary school level increased from 80 % in 2000 to 98 % in 2015( 40 ), yet about 5 million Bangladeshi children between the ages of 6 and 13 years – mostly from poor families, urban slums and hard-to-reach areas – remain out of school. It is vital to target this group for education. The role of parents’ education in reducing risk of stunting and underweight is most likely explained by attaining higher knowledge about health and nutrition for their children, likelihood of higher household income and the role in decision making for food selection. Education also provides a platform to obtain protective childcare behaviours such as completing childhood immunizations, better feeding and sanitation practices, and use of iodized salt( Reference Hasan, Soares Magalhaes and Williams 41 ). Therefore, the government’s endeavours to promote further education beyond primary school education would positively affect intergenerational nutritional status. Women continue to lag behind men in higher secondary and tertiary education with secondary school net enrolment of about 54 %, up from 45 % in 2000. Higher educational attainment in mothers is likely to promote female empowerment and partaking in household decision making, which has been shown to reduce malnutrition indices by 15–32 % in Bangladesh( Reference Rahman, Saima and Goni 42 ). It is important for Bangladesh to emphasize wealth creation, father’s education and mother’s education within poor households so that malnutrition can be minimized among children from vulnerable households.
Other associated factors for stunting and underweight were gender, rural residence and maternal underweight, which are comparable with other studies( Reference Chowdhury, Rahman and Khan 19 , Reference Das and Gulshan 20 , Reference Siddiqi, Haque and Goni 22 , Reference Das and Sahoo 23 , Reference Kandala, Madungu and Emina 25 , Reference Dani, Satav and Pendharkar 43 – Reference Tariku, Mulugeta and Tsadik 47 ). Mother’s BMI was a significant contributor to malnutrition, indicating that in households where the mother is exposed to a poor diet, the children too are vulnerable and emphasizing the need for identifying households for targeting. Usually urban areas have greater accessibility and range of health services, as well as greater choices and opportunities for livelihood, and this in turn may assist children and their parents for the betterment of nutritional practices( Reference Srinivasan, Zanello and Shankar 48 – Reference Van de Poel, O’Donnell and Van Doorslaer 50 ). However, given that the determinants of child nutritional status are similar across urban and rural areas, while similar programmes can be implemented, efforts to improve the key socio-economic constraints specific to each area should be prioritized. Our study found gender differences to be significant for stunting only, with no differences in other parameters, and therefore indicates that growth monitoring needs to focus on both genders.
The present study has several strengths. First, we used multiple nationally representative household survey data points which have a high response rate. Through this, our study was able to generalize and predict forecasts for Bangladesh with limited sample bias. Second, the study considered appropriate statistical tools such as multilevel modelling to assess the risk factors of stunting, wasting and underweight. Finally, we used Bayesian regression analysis to estimate future projections for child malnutrition based on recent trends, which will be helpful for health policy makers for introducing new interventions to reduce the prevalence as well as the burden of childhood malnutrition. However, along with the above-mentioned strengths, our study has certain limitations. We were unable to establish a causal relationship between risk factors and the dependent variables due to the cross-sectional nature of the study. In addition, due to the unavailability of data on potential confounders including diet, food insecurity, physical exercise and smoking behaviour of the parents, these were not included in analysis. The Bayesian models projected prevalence of malnutrition indicators assuming a linear trend of previous years. This assumption is strict and might not be realistic if changes occur in health policy. However, we aimed to inform policy makers about the magnitude of the malnutrition problem in the future if current trends continue, and thereby highlight the need for interventions to change this trend. The assumed linearity of the trend is a simple assumption which can easily be understood. Although speculative, one could imagine that the lower the prevalence of malnutrition, the harder it is to address the remaining pockets of malnutrition. In such case the reduction in prevalence could be expected to decrease (rather than be constant as implied by the linearity assumption). If this is true, then the present analysis underestimates the gaps between projected and targeted prevalence of malnutrition.
Conclusion
In conclusion, although the prevalence of U5C malnutrition declined between 1990 and 2015, it is projected to continue to exist in a large proportion of children up to 2030, if the same linear trend persists. The risk of stunting, wasting and underweight in U5C is significantly higher among poorer households and children of lower educated parents. To accelerate reduction of malnutrition by 2030, education programmes and income-generating activities targeted to poor households, in addition to targeted nutrition care of the mother and child, should be supported as stated in the national policy agenda.
Acknowledgements
Acknowledgements: The authors are grateful to MEASURE DHS for providing the data set. In addition, they would like to acknowledge all individuals and institutions in Bangladesh who were involved in implementing the BDHS. The authors gratefully acknowledge the Department of Global Health Policy, The University of Tokyo, Japan, where this study was conducted. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: There are no conflicts of interest. Authorship: M.R.I., M.S.R. and M.Mi.R. conceptualized the basic idea for the study. M.R.I. performed the statistical analysis together with M.S.R. and M.Mi.R. M.R.I. and M.S.R. prepared data for analysis. M.R.I. prepared the first draft the manuscript. J.J. and M.Mi.R. checked the consistency of the manuscript. J.J., M.S.R., M.Ma.R., S.N., A.d.S., P.L. and M.Mi.R. critically revised the manuscript for intellectual content. All authors have reviewed and approved the final manuscript. Ethics of human subject participation: This study used publicly available secondary data sets (BDHS, MICS and CMNS). Informed consent was obtained from the participants by the survey authority. Ethical approval was not required.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S136898001900140X