Introduction
Due to reasons such as increasing numbers of chronic diseases and weakening of the immune system with ageing and environmental factors, increases in the prevalence and severity of infections are observed in older populations. The most cost-effective method for the reduction of mortality, particularly with respect to infections, is primary prevention. As a result of vaccination, a reduction is observed in the frequency and spread of infections. Accordingly, there are decreases in hospitalisation rates, workforce reductions, morbidity and mortality rates, and economic losses (Koldas, Reference Koldas2017; Toprak et al., Reference Toprak, Koksal, Sargin and Akan2018).
The vaccines that should be administered to individuals who are 65 years of age and older include the seasonal influenza, pneumococcus, tetanus, and hepatitis B vaccines. These vaccines confer protection within 1–2 weeks of administration. These vaccines are provided free of charge for individuals who are aged 65 years and older (Sunay and Demirel, Reference Sunay and Demirel2011). When necessary, other vaccines (tetanus, diphtheria, pertussis, chickenpox, hepatitis, meningococcus, rabies, typhoid, and cholera) are also recommended for elderly adults based on their level of risk (Hogue and Meador, Reference Hogue and Meador2016; Peck et al., Reference Peck, Gacic-Dobo, Diallo, Nedelec, Sodha and Wallace2019).
Pneumococcal disease incidence and mortality increase at the age of 50 years and significantly increase after the age of 65 years. For this reason, it is recommended that individuals aged 65 years and older receive a pneumococcal vaccine. It is also advised that an initial conjugate vaccine (PCV13) and then a polysaccharide vaccine (PPSV23) should be consecutively applied at least 1 year apart, if possible. Booster shot doses are not needed (Ekmud, 2016; Falkenhorst et al., Reference Falkenhorst, Remschmidt, Harder, Hummers-Pradier, Wichmann and Bogdan2017).
The annual rate of pneumococcal vaccination in a vaccination clinic in India was determined to be 7% (Lahariya and Bhardwaj, Reference Lahariya and Bhardwaj2019). Similarly, the rate of vaccination in Turkey is 6.4% (Yılmaz et al., Reference Yilmaz, Yilmaz, Ceyhan, Kasim, Kaya, Odabas, Sargin, Bahadir and Ozkara2018). The immunisation programmes for elderly individuals are still inadequate in Turkey, and despite the availability of effective vaccines, vaccination coverage rates remain low among the elderly population. In our study, we observed the impact of doctor recommendations of the pneumococcal vaccine to individuals on the phone or during face-to-face interviews on vaccination rates.
Materials and methods
Our study is a cross-sectional study that included 200 patients who were older than 65 years and registered at the Dogantepe Education Family Health Center of the Ankara Training and Research Hospital. Prior to conducting the study, written approval was obtained from the Ethics Board of the Ministry of Health Ankara Training and Research Hospital (22/February/2017 – meeting no. 0675 and no. 5673). The study aimed to include 231 patients who were older than the age of 65 years. Eighteen patients could not be reached due to missing contact information and changes in address. Thirteen patients did not participate in the study. Two hundred patients who were reached and agreed to participate in our study after having been informed about our questionnaire constituted our study sample.
In the questionnaire, which was prepared by the researchers after reviewing the relevant literature, the sociodemographic attributes of the participants (age, sex, educational status, income status, social security status, marital status, number of people living in the house, smoking status, and presence of chronic disease) were collected. The participants were asked if they knew their vaccination status, and if they knew it, they were asked about the source of their knowledge and their knowledge of and attitudes towards the tetanus, influenza, hepatitis, and pneumococcal vaccines.
The questionnaire was administered to 103 patients who attended the polyclinic between 1/March/2017 and 31/May/2017 through face-to-face interviews with their doctors. Ninety-seven patients who did not attend our family health centre were also asked to complete the questionnaires over the telephone. These questionnaires were administered by their family doctors. Following the completion of the questionnaire, the patients were informed about the pneumococcal vaccine and were asked whether they wanted to be vaccinated. The patients who agreed to be vaccinated were prescribed the polysaccharide pneumococcal vaccine at the family health centre.
Statistical analysis
The statistical evaluation was performed with IBM SPSS 15.0 (SPSS Inc., Chicago, IL, USA). Numerical variables were given as averages ± standard deviations, while categorical variables were given as frequencies (percentages). The relationships between groups were determined with Pearson’s chi-square test and Fisher’s exact chi-square test analyses. Moreover, the factors affecting the dependent variable were determined with logistic regression analysis. In the analyses with multiple variables, P < 0.20 was accepted as sufficient for statistical significance in the selection of a covariate. For other sources, P < 0.05 was considered to be statistically significant.
Results
A total of two hundred people who were 65 years of age and older were included in the study. A total of 113 (56.5%) of the participants were women, and the average age was 72.26 years. Regarding education levels, 113 of the participants (56.5%) were literate, while 87 (43.5%) were not. A near-majority of participants (45%) had a monthly income between 1000 and 1499 TL. The average monthly income was 1182 TL. Thirty-eight (19%) of the participants did not receive social security benefits. A total of 66.5% of the participants in the study were married. Statistically significant relationships were not found between pneumococcal vaccination rates and sex, educational status, monthly income, social insurance, marital status and number of people living in the house (P > 0.05).
Seventy-three percentage of the participants smoked. The prevalence of chronic disease was 85%. While a statistically significant relationship was not found between smoking status and pneumococcal vaccination rates, the pneumococcal vaccination rates of the patients who had a chronic disease were higher than that of those who did not have a chronic disease (P < 0.05). The prevalent chronic diseases were hypertension, diabetes and benign prostatic hyperplasia (Table 1).
Table 1. Demographic characteristics

The knowledge statuses of the participants regarding adult vaccination are shown in Table 2. A total of 86.5% of the participants knew about the vaccines, and more than half of them (59.5%) stated that they had obtained information about the vaccines from doctors or healthcare professionals.
Table 2. Awareness of vaccination status among adults and sources of information
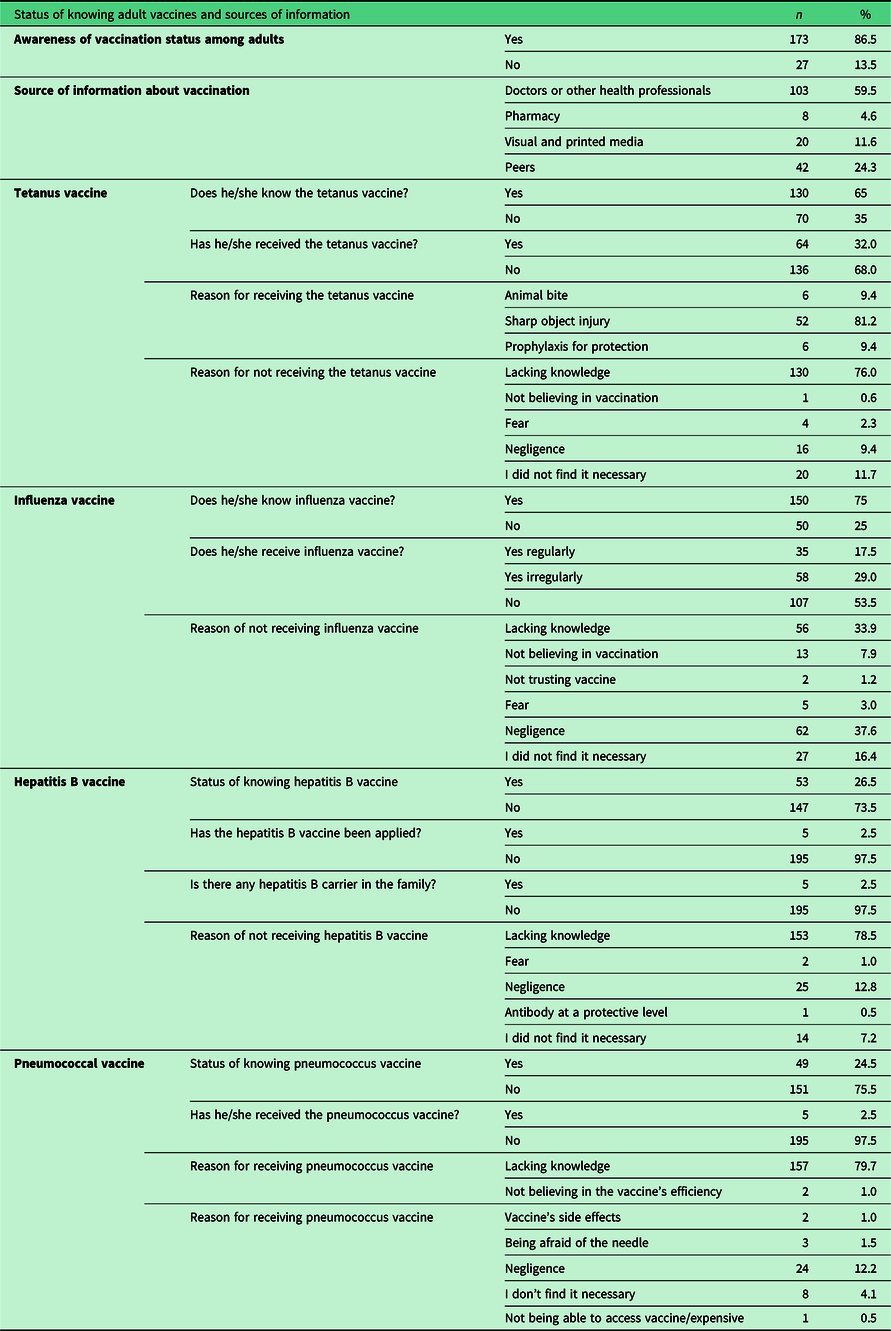
In total, 24.5% (n = 49) of the participants stated that they knew about the pneumococcal vaccine. Only 2.5% of the participants had received the pneumococcal vaccine. The predominant reason for not receiving the pneumococcal vaccine was a lack of information (79.7%), and similar results were observed for the other vaccines. It was observed that significantly (P < 0.05) more individuals who had chronic diseases than those who did not have chronic diseases had received the pneumococcal vaccine.
After receiving information about the pneumococcal vaccine, 71% (n = 142) of the participants agreed to receive the pneumococcal vaccine (Figure 1).

Figure 1. The participants’ rates of receiving the pneumococcal vaccine before and after they received information about it.
This study was conducted with 200 patients. One hundred three patients (51.5%) attended the polyclinic and participated through a face-to-face interview. Ninety-seven patients (48.5%) who did not attend the polyclinic participated via a telephone call. In total, 58 of the 97 patients (59.8%) who completed the questionnaire via a telephone call and 84 of the 103 patients (81.6%) who completed the questionnaire via a face-to-face interview received the pneumococcal vaccine. The vaccination rate was significantly higher in the group who participated in face-to-face interviews (P < 0.001).
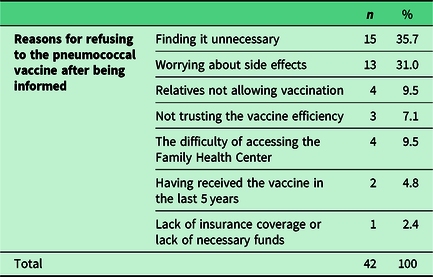
The most frequent reasons for refusing to receive the vaccine (35.7%) were finding it unnecessary (35.7%) and worrying about side effects (31%) (Table 3).
Table 3. The participants’ reasons of not receiving the pneumococcal vaccine after they received information about it
According to the results of the logistic regression analysis, those without chronic diseases received the pneumococcal vaccine 2.8 times less frequently than those with chronic diseases. Compared to those who did not receive the influenza vaccine regularly, those who did receive the influenza vaccine regularly received the pneumococcal vaccine five times less frequently. Those who received the influenza vaccine irregularly received the pneumococcal vaccine 5.6 times less frequently than those who did not receive the influenza vaccine. The patients who completed the questionnaire during face-to-face interviews received the pneumococcal vaccine 3.2 times more frequently than those who completed the questionnaire over the phone.
Discussion
The Global Immunization Vision and Strategy of the World Health Organization, ratified by 194 member states in May 2012, was developed to prevent millions of deaths before 2020 by means of increasing access to existing vaccines in all communities. Unfortunately, adult vaccination rates continue to be below the objectives for 2020 for most of the routinely recommended vaccines, in contrast to other preventive services.
In a study that included 2918 patients, it was found that 2.8% received both the pneumococcal and influenza vaccines. The rate of influenza vaccination was 12.3%, whereas 3% of the participants had received the pneumococcal vaccine (Erbay et al., Reference Erbay, Kade, Ede, Suher, Akyol, Intepe, Borekci, Yildirim and Erbay2018). In our study, 17.5% (n = 35) of the participants regularly received the influenza vaccine, 32% (n = 64) received the tetanus vaccine, 2.5% received the hepatitis B vaccine and 2.5% received the pneumococcal vaccine. Compared with the data reported in the literature, these data reveal the necessity of exerting more effort to ensure adequate adult immunisation coverage.
At the state level, the “Extended Immunization Program” was initiated to provide immunisation to sensitive age groups to control and even eliminate invasive pneumococcal diseases and other specific diseases. With this system, a consistent 95% vaccination rate was the target among adults (Kim et al., Reference Kim, Riley and Hunter2018). However, it is difficult for this endeavour alone to achieve this goal. Healthcare professionals and society must also participate. It is important for doctors to focus on consultations and educational services to convey the message to the target audience. In our study, the pneumococcal vaccination rate increased after face-to-face interviews and phone calls.
When the obstacles to adult vaccination are examined, the target audience’s initial vaccination status is not known and patients do not ask to be vaccinated. In addition, patients’ lack of knowledge about vaccines and concerns about the reliability of the vaccines are among the factors that decrease immunisation rates (Hillson et al., Reference Hillson, Barash and Buchanan2011; Szilagyi et al., Reference Szilagyi, Shone, Barth, Kouides, Long, Humiston, Jennings and Bennett2005). An experienced family doctor who is willing to vaccinate can overcome this obstacle.
Peetermans et al. reported that having a chronic disease is a primary predictive factor for pneumococcal vaccination (Peetermans and Lacante, Reference Peetermans and Lacante1999). In our study, it was found that having a chronic disease affected the pneumococcal vaccination rate. Unfortunately, these rates are not sufficient. Follow-up for chronic diseases should include vaccination reminders.
In the study by Ozisik et al., the lack of knowledge cited as the reason for not receiving the vaccine by 71.4% (n = 85) with regard to the pneumococcal vaccine and 64% (n = 64) with regard to the influenza vaccine (Ozisik et al., Reference Ozisik, Yekeduz, Tanriover, Helvaci, Basaran and Unal2016). The failure of healthcare professionals to recommend the vaccine was cited by 21.8% (n = 26) with regard to the pneumococcal vaccine and 18% (n = 18) with regard to the influenza vaccine. With respect to patients’ knowledge of their pneumococcal vaccination status, 49 of 200 (24.5%) patients participating in our study knew their status. Akman et al. found that knowledge of vaccines and vaccination status were very low among the participants (Akman et al., Reference Akman, Sarisoy, Uzuner, Cifcili, Uc, Guzel and Dikmen2014). The results of our study show that adults’ awareness of their vaccination status was poor, which is similar to the findings in other studies. Increasing awareness of vaccines can increase vaccination rates.
When the source of information for the acquired knowledge of adult immunisation was examined, it was observed that knowledge is most frequently obtained from doctors. This was also observed in our study, although the rates in the literature differed from those in our study (Mutlu et al., Reference Mutlu, Coskun and Sargin2018). In the study by Asik et al., it was stated that 27% of the participants had obtained information about adult vaccines from doctors and/or pharmacists (Asik et al., Reference Asik, Cakmak and Bilgili2013). In the study by Skowronski et al., this proportion reached 54% (Skowronski et al., Reference Skowronski, Pielak, Remple, Halperin, Patrick, Naus and McIntyrea2004). In our study, knowledge was most often obtained from doctors and other health professionals (n = 103; 59.5%).
Although the source of knowledge about adult vaccines was mostly doctors or other health professionals, an insufficient proportion of the study population had adequate knowledge of vaccination, given that a lack of knowledge is a critical reason for not receiving vaccinations. This situation indicates that more information about adult vaccines must be given to patients, and the importance of vaccines must be emphasised. In a study by Larson et al. (Reference Larson, Bergman, Heidrich and Alvin1982), patient education or patient reminders were shown to be effective at increasing community demand for vaccines (Larson et al., Reference Larson, Bergman, Heidrich and Alvin1982). Healthcare professionals should provide more information about vaccines during visits.
In addition, 158 participants (79%) agreed to undergo vaccination after briefly receiving information. While the proportion of those who were vaccinated after a face-to-face interview was 81.6%, it was approximately 59.8% among those who were reached via phone. It is noteworthy that the proportion of vaccinated participants was 2.5% before our study and 71% after our study. The face-to-face interview was found to be 3.2 times more effective than the phone call. These results demonstrate the importance of providing consultation regarding vaccination to improve vaccination rates. Moreover, the contribution of the patient–doctor meeting is undeniably important.
Adult vaccination plays an important role in preventive medicine, is easily applicable and is efficient and cost-effective. Although chronically ill patients visit their doctors frequently, it is evident that opportunities for vaccination had been missed in this group. Missed opportunities for vaccination in elderly adults represent a very important problem worldwide (Nowalk et al., Reference Nowalk, Zimmerman, Cleary and Bruehlman2005). Our study revealed that it is necessary to pay more attention to the administration of vaccinations, and doctors have important responsibilities with regard to increasing vaccination rates.







