No CrossRef data available.
Article contents
Decrease in antipsychotic and other psychotropic medication during 30 months of lifestyle intervention among outpatients with schizophrenia
Published online by Cambridge University Press: 23 March 2020
Abstract
Patients with schizophrenia have 3-fold higher mortality from lifestyle diseases, and a long-lasting exposure to antipsychotic medication may contribute to the development of somatic illnesses. Region of Central Jutland was inspired by European initiatives to establish a lifestyle intervention program in an attempt to reduce mortality among individuals with severe mental illness.
To investigate whether this intervention could possibly lower the need for antipsychotic treatment, and to provide a unique view of actual medication practice.
To investigate the influence of a lifestyle intervention program on changes in antipsychotic medication and polypharmacy in an unselected cohort of patients with newly diagnosed schizophrenia.
Observational study of outpatients participating in a program with individual consultations, group sessions and exercise groups.
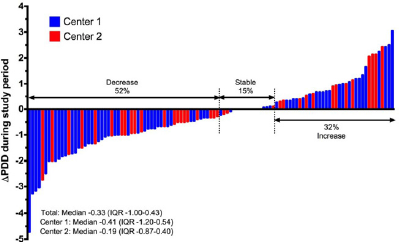
One hundred and eleven patients were eligible for analysis. Fifty-four percent of the patients were subject to antipsychotic monotherapy. Median Defined Daily Dose (DDD) of antipsychotics was 1.3 at index (interquartile range [IQR] 0.67–2.00). Fifty-two percent of the patients experienced a decrease in DDD during the period with median change of −0.33 DDD (IQR −1.00 to 0.43). We found no significant difference in baseline variables or extend of participation between patients with decrease in doses and patients with increase (Fig. 1).
Most patients decreased or stabilized their doses of antipsychotic medication during the study period. Half of the patients were subject to antipsychotic polypharmacy. Extend and type of participation in the lifestyle intervention program did not correlate to changes in dosing of antipsychotic medication.
The authors have not supplied their declaration of competing interest.
Fig. 1
Change in total DDD from index to follow-up (111 patients).
- Type
- e-Poster Walk: Psychopharmacology and pharmacoeconomics and psychoneuroimmunology
- Information
- European Psychiatry , Volume 41 , Issue S1: Abstract of the 25th European Congress of Psychiatry , April 2017 , pp. S368
- Copyright
- Copyright © European Psychiatric Association 2017



Comments
No Comments have been published for this article.