Anticholinergic medications have been shown to worsen cognition in the elderly and their use has been associated with lower Mini-Mental Status Examination (MMSE) scores.Reference Lechevallier-Michel, Molimard, Dartigues, Fabrigoule and Fourrier-Reglat 1 The American Geriatric Society updated Beer’s Criteria in 2012 to give prescribers insight into the potentially harmful properties of common medications with the goal of improving care for the elderly population.Reference Campanelli 2 Patients with Alzheimer’s disease are even more susceptible to anticholinergic effects.Reference Bayón and Sampedro 3 Current literature maintains that benzodiazepines, opioids, and medications with anticholinergic properties are best avoided in the elderly unless absolutely essential because they have been shown to worsen cognition and can cause behavior change.Reference Lechevallier-Michel, Molimard, Dartigues, Fabrigoule and Fourrier-Reglat 1 - Reference Bayón and Sampedro 3 Prescribers must be aware that polypharmacy may affect cognition and should consider this when managing their patients.Reference Bayón and Sampedro 3
Saskatchewan, a western Canadian province, has a population of about one million, with nearly 40% of those people living in rural areas and small towns, defined as centers with fewer than 10,000 people.Reference Elliot 4 Rural centers tend to have higher elderly populations than urban areas, with about one in five people in a typical Saskatchewan town older than age 65.Reference Elliot 4 With a small population dispersed across the province, geographical access has been a critical barrier to equal access to care for people in rural communities.Reference Laurent 5 In 2006, nearly 17% of the rural population was older than age 65.Reference Elliot 4 As age increases, so does risk of dementia. In Canada, 14.9% of people older than age 65 have some form of dementia. 6 To improve access to specialist diagnosis for rural patients, the Rural and Remote Memory Clinic (RRMC) was started in 2004. The initial visit involves assessment by a neurologist, neuropsychologist, physiotherapist, dietitian, and neuroimaging.Reference Crossley, Morgan, Lanting, Dal Bello-Haas and Kirk 7 At the end of the day, patients receive a diagnosis and treatment plan, including information about necessary follow-up via telehealth.Reference McEachern, Kirk, Morgan, Crossley and Henry 8 , Reference Morgan, Crossley and Kirk 9 Telehealth allows patients to receive the care they require without having to leave their home community, thus limiting the burden placed on caregivers and the health care system.Reference Crossley, Morgan, Lanting, Dal Bello-Haas and Kirk 7 , Reference McEachern, Kirk, Morgan, Crossley and Henry 8 The clinic is described in more detail elsewhere.Reference Crossley, Morgan, Lanting, Dal Bello-Haas and Kirk 7 - Reference Morgan, Crossley and Kirk 9
In 2008, Steve et al analyzed the medication lists that 66 patients brought to their first visit at the RRMC.Reference Steve, Kirk and Crossley 10 The focus of that article was on the prevalence of polypharmacy, anticholinergic medication use, and benzodiazepine use.Reference Steve, Kirk and Crossley 10 They found that, at initial presentation, 24% of patients were taking an anticholinergic medication, 14% were taking a benzodiazepine, and the average number of medications per patient was 4.80 (standard deviation [SD], 3.66).Reference Steve, Kirk and Crossley 10 However, it is important to quantify how physicians have changed their practices over time as more information about medication use and cognition has become available. The present study examined medication use by patients at presentation to the RRMC between March 2004 and June 2015 to see whether patterns of medication use have changed over time in patients with cognitive concerns.
Methods and Analysis
The first 444 patients seen at the RRMC between March 2004 and June 2015 were included in this analysis. At each patient’s first visit to the RRMC, patients (or their primary caregiver) are asked to bring a list of current medications. From the reports of the patient’s initial assessment, medications were categorized based on their anticholinergic properties and it was noted if they were already taking a cholinesterase inhibitor.Reference Campanelli 2 , Reference Carrahan, Lund, Perry and Chrischilles 11 Medications considered anticholinergic included the American Geriatric Society’s Updated Beer’s Criteria and ranitidine in an effort to be consistent with Steve et al’s paper and to form an accurate picture of trends over the 11-year period.Reference Campanelli 2 , Reference Steve, Kirk and Crossley 10 We additionally catalogued medications with central nervous system effects (benzodiazepines, hypnotics, non-anticholinergic antidepressants, antiepileptics, and lithium) and recorded each patient’s total number of medications.Reference Campanelli 2 , Reference Bayón and Sampedro 3 , Reference Foy, O’Connell, Henry, Kelly, Cocking and Halliday 12 , Reference Moore and O’Keefe 13
In an attempt to quantify polypharmacy, we totaled the number of medications at initial presentation. We excluded one patient in this analysis who presented on 27 medications and was considered an outlier, as the next closest patient had 15 medications on his or her list. For further analysis, we catalogued the score of the MMSE, which is administered during the initial clinic visit.Reference McEachern, Kirk, Morgan, Crossley and Henry 8 The MMSE is a brief examination that provides a general measure of a patient’s cognitive status rated on a 30-point scale, with a lower score indicating greater impairment.Reference McEachern, Kirk, Morgan, Crossley and Henry 8
Patients were assigned to a 12-month period based on the date of their initial presentation. We then calculated prevalence of anticholinergic medication use, total medications, and medications with central nervous system effects for each period. Statistical analysis of these medication categories was conducted to examine trends in medication use over time. Percentages and frequencies were then calculated for each of these 12-month periods. Spearman correlation coefficient was used to measure the association between medication use and time. Ethics approval for this study was obtained from the Biomedical Research Ethics Board at the University of Saskatchewan.
Results
Between March 2004 and June 2015, 444 patients were seen at the RRMC. Mean patient age was 77.4 years (SD=12.0). Mean MMSE at initial presentation was 22.4 (SD=5.8). The most frequent diagnosis (Table 1) at initial assessment was Alzheimer’s disease (43.5%). Other common initial diagnoses were: mild cognitive impairment (15.3%), frontotemporal dementia (10.3%), Lewy body dementia (4.9%), vascular dementia (4.5%), and vascular/Alzheimer’s dementia (2.7%).
Table 1 Breakdown of diagnosis made at patient’s initial visit (N=444)
Other diagnoses (number of patients): corticobasal degeneration (3), hydrocephalus (3), medication side effects (2), depression (1), epilepsy (1), Fragile X–associated dementia (1), herpes encephalitis (1), hypoxic ischemic encephalopathy (1), multiple systems atrophy (1), Parkinson’s dementia (1), posterior cortical atrophy (1), progressive supranuclear palsy (1), transient ischemic attacks (1).
Ninety-one patients (20.5%) were taking at least one anticholinergic medication (Table 2). Eighty patients (18.0%) were taking one anticholinergic, medication, and eleven patients were taking two. Thirty-two of a total 193 patients with Alzheimer’s disease were taking an anticholinergic medication (16.6%). Of the 91 patients that were taking an anticholinergic medication, 68 had some form of dementia or mild cognitive impairment (74.7%). Eleven of the 91 patients taking an anticholinergic medication were simultaneously taking a cholinesterase inhibitor (12.1%).
Table 2 Breakdown of type of anticholinergic medications at initial presentation (N=444)
Patients were on an average of 5.2 medications each (n=444; range, 0-15; SD, 3.46) (Table 3). Forty patients (9.0%) were on no medications, whereas 339 patients (89.7%) were taking three or more medications.
Table 3 Number of current medications at initial clinic visit (N=444)
We also looked at trends in average number of medications taken over time (Figure 1). There was a weak positive correlation between total medications per patient and time (Spearman’s correlation coefficient =0.11, p=0.017) as the average number of medications per patient increased from 5.3 in 2004 to 7.0 in 2014.
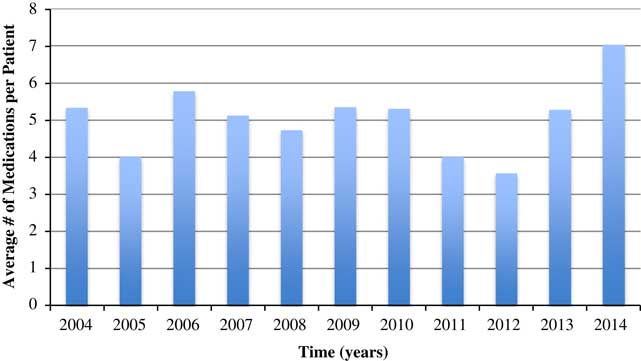
Figure 1 Average number of medications per patient by year of clinic operation.
As shown in Figure 2, we saw a slight decline in percentage of patients presenting with anticholinergic medications over time (Spearman’s correlation coefficient =−0.64, p=0.035).
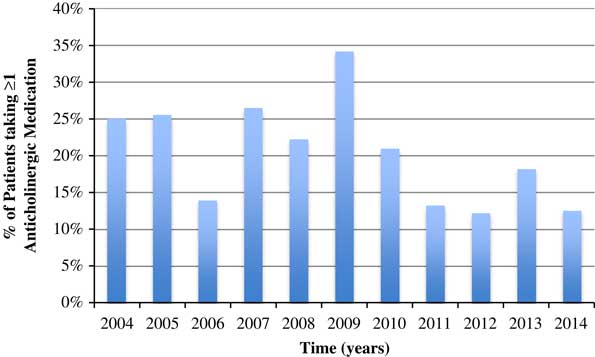
Figure 2 Percentage of patients taking at least one anticholinergic medication over time.
There was no statistically significant relationship between use of medications that affect the central nervous system and time (Spearman’s correlation coefficient =0.09, p=0.790) (Figure 3). Despite the lack of statistical significance, there appears to be an increase in the use of these medications between 2012 and 2014. These medications include benzodiazepines, hypnotics, antidepressants (non-anticholinergic), and antiepileptics.Reference Campanelli 2 , Reference Bayón and Sampedro 3 , Reference Foy, O’Connell, Henry, Kelly, Cocking and Halliday 12
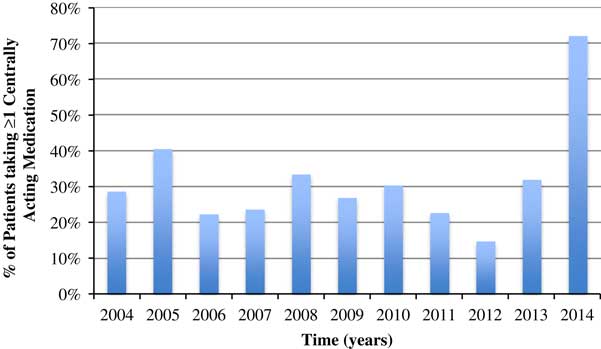
Figure 3 Percentage of patients taking at least one centrally acting medication over time.
Sixty-three patients (14.2%) presented to the RRMC already taking a cholinesterase inhibitor.Reference Carrahan, Lund, Perry and Chrischilles 11 Of these, eight (12.7%) were taking an anticholinergic medication concurrently. Thus, 1.8% (8/444) of patients presented on both an anticholinergic medication and a cholinesterase inhibitor simultaneously.
Conclusion
The most encouraging statistic to come from this study is a decline in anticholinergic medication use by the rural elderly population as they presented to the RRMC. Educating prescribers about the problems of prescribing anticholinergic drugs has been shown to be important for patients older than age 65 years.Reference Campanelli 2 This result suggests that prescribers are becoming more aware of the potentially harmful effects of anticholinergic medications in elderly populations.Reference Campanelli 2 Looking at specific medications, it is important to consider that some medications (eg, bladder medications)Reference Scheife and Takeda 14 may still benefit the patient more than any inherent cognitive risk. However, the solution may be as simple as switching the prescription to a different drug within the same class.Reference Furlan, Kallan, Ten Have, Pollock, Katz and Lucki 15 One example is paroxetine, a selective serotonin reuptake inhibitor antidepressant (6.7% of patients presented with it on their medication list).Reference Campanelli 2 , Reference Furlan, Kallan, Ten Have, Pollock, Katz and Lucki 15 Other selective serotonin reuptake inhibitors have less anticholinergic activity and may be a better choice in elderly populations.Reference Campanelli 2 , Reference Furlan, Kallan, Ten Have, Pollock, Katz and Lucki 15
When Steve et al examined the prevalence of anticholinergic medication use at the RRMC in 2008, they found that 24.0% of the 66 patients they had seen were taking some form of anticholinergic medication.Reference Furlan, Kallan, Ten Have, Pollock, Katz and Lucki 15 Of the 444 patients (including the initial 66 analyzed by Steve et al) who have now been seen at the RRMC, 20.5% were taking a medication with anticholinergic properties at initial presentation.
In 2004, Carrahan et al found that 35.4% of patients with a cholinesterase inhibitor on their prescription list also had an anticholinergic medication on their prescription list from their primary care physician.Reference Carrahan, Lund, Perry and Chrischilles 11 The proportion of RRMC patients is lower than previously reported by Carrahan et al, in which only eight of the 63 patients (12.7%) who presented with a cholinesterase inhibitor on their medication list were also taking an anticholinergic medication.Reference Carrahan, Lund, Perry and Chrischilles 11
Research has shown that polypharmacy may be associated with increased cognitive symptoms.Reference Bayón and Sampedro 3 , Reference Moore and O’Keefe 13 Considering that patients were taking an average of 5.2 medications each, it is critical for caregivers to be aware of the possible impact that polypharmacy may have on a patient’s cognition.Reference Bayón and Sampedro 3 , Reference Moore and O’Keefe 13 Informed prescribing is essential to limit unnecessary side effects, particularly in patients with memory concerns.Reference Campanelli 2 , Reference Bayón and Sampedro 3 , Reference Moore and O’Keefe 13 Prescribers must be properly informed to ensure that the number of medications per patient does not continue to rise, that medications are only used when necessary, and that potentially deleterious medications are avoided.Reference Campanelli 2 , Reference Bayón and Sampedro 3 , Reference Moore and O’Keefe 13
Disclosures
None of the authors have anything to disclose.








