Introduction
The association of Wilder Penfield with McGill University and the Montreal Neurological Institute (MNI) is well known, but Penfield did not alight on fallow ground. As early as 1867, Reference Reddy1 surgeons affiliated with McGill University operated to elevate depressed skull fractures, remove inwardly driven bone fragments, and drain extradural blood clots and pus. 2–Reference Bell10 Few dared to breach the dura for fear of blindly damaging vital structures.
The localization of specific functions to distinct parts of the brain was the determining factor that led surgeons to venture intracranially. That knowledge of the structure–function relationship of the brain could guide the surgeon’s trephine was first demonstrated by Pierre-Paul Broca in 1876. Reference Broca11 Most important in the localization of surgically amenable lesions was the recognition of the somatotopic organization of motor functions to the human precentral gyrus by Jean-Martin Charcot and Charles Pitres, in a series of papers published between 1877 and 1879. Reference Charcot and Pitres12–Reference Charcot and Pitres14 Just as crucial to the development of intracranial surgery was Charcot’s realization that if a patient was not paralyzed between Jacksonian seizures, the offending lesion was only in the proximity of the sensorimotor area and merely irritated it, and could then be resected. Reference Leblanc15 If the limb was paralyzed interictally, resection was foolhardy. Charcot’s work was known to William Macewen, Reference Macewen16 Rickman Godlee, Reference Bennett and Godlee17 John Hughlings Jackson, Victor Horsley, and William Osler Reference Leblanc15 and led Macewen, Godlee, and Horsley to incise the brain to remove mass lesions. Reference Leblanc15 The ability to localize cortical lesions and to ascertain their operability led Osler to write a series of influential papers between 1884 and 1889 Reference Osler18–Reference Osler20 in which he encouraged surgeons in North America Reference Osler21 to operate on the brain for a variety of structural lesions. As a result of Osler’s endorsement, physicians and surgeons of Montreal’s newly opened Royal Victoria Hospital (RVH) united their efforts toward the diagnosis and treatment of intracranial mass lesions. The argument is made that the collaboration of physicians and surgeons James Stewart and James Bell and their successors Colin Russel and Edward Archibald created an institutional culture at McGill that favored the integration of neurology, neurosurgery, and allied disciplines within an autonomous Department of Neurology and Neurosurgery under Wilder Penfield’s leadership.
Materials and Methods
The early history of neurosurgery at McGill is chronicled in cases reported to the Montreal Medico-chirurgical Society (MMCS) and published in the Montreal Medical Journal. These and publications in other journals are reviewed Reference Brennan22 (Table 1). The collaborative culture created by Stewart and Bell, and Russel and Archibald reflected in their publications is highlighted.
Table 1: Prominent Canadian medical journals, 1864–1928

* The Canada Medical Journal continued publication as The Canada Medical and Surgical Journal.
** The Montreal Medical Journal and The Maritime Medical News fused to form The Canadian Medical Association Journal.
*** The Canadian Journal of Medical Science continued publication as The Canadian Practitioner.
William Osler and Intracranial Surgery
Osler’s interest in neurosurgery can be dated to a tragic case that he reported to the MMCS in 1883. Reference Osler18 The case was of a 14-year-old girl who suffered from focal motor seizures beginning in the left hand and arm that spread to the leg before becoming generalized, and who died in status epilepticus. Osler found ‘a hard, resistant mass in the right hemisphere, occupying the upper end of the [right] ascending frontal convolution,’ which he diagnosed as a ‘fibro-glioma’ and was most likely a pilocytic astrocytoma. Osler concluded from this case that, “operation would have been justifiable and possibly have been the means of saving her life.” Reference Osler20 Osler was profoundly affected that a 14-year-old girl had died from what he considered to have been a operable lesion and he referred to her case in a most influential paper that he published in the Canadian Journal of Medical Sciences in 1889, entitled ‘On the conditions of the brain suitable for operative interference.’ Reference Osler21
Osler considered that the decision whether a lesion was suitable for surgery rested with a physician, whose responsibility was to localize the lesion, diagnose its nature, and decide if it was amenable to surgery. The surgeon’s role was to agree to the physician’s diagnosis and operate. Based on localization and presumptive etiology, Osler considered that certain tumors, most notably fibromas (meningiomas) and fibro-gliomas, were potentially operable, as were abscesses, and especially those associated with purulent otitis media, which were easily localized. Osler was most enthusiastic for surgery in cases of Jacksonian epilepsy, ‘which,’ he wrote, echoing Charcot, ‘usually [results from] a localized growth, a source of irritation upon the cortex, causing a discharging lesion,’ and concluded, ‘The field here is wide open.’ Reference Osler21
Stewart and Bell
When the RVH opened its doors in 1894, it was the finest and best-equipped hospital on the continent Reference Terry23 (Figure 1). It was there that neurology and neurosurgery began in Canada, through the combined efforts of James Stewart and James Bell. Osler’s enthusiastic support of intracranial surgery had a determinant effect on Stewart, a physician, and Bell, a surgeon who shared an interest in the diagnosis and treatment of neurological patients. Reference Hanaway, Cruess and Darragh24 James Stewart (Figure 2) graduated in medicine from McGill in 1869. He rapidly established himself as ‘the most important consultant in medicine in Montreal, [and] the first neurological consultant at McGill,’ qualities that led to his appointment as the first physician at the RVH, ‘where his best work was done [and where] most of his papers [on] disease of the nervous system’ were written. 25 James Bell (Figure 3) obtained his doctorate in medicine from McGill in 1877, where he befriended William Osler. He was appointed Surgeon-in-Chief at the RVH in 1894. Bell matched Stewart’s interest in neurology, and he was quickly assigned neurosurgical cases. Reference Bell8,Reference Bell10,Reference Bell26,Reference Bell27 He was the first to use x-rays as a guide in the treatment of penetrating head injuries, a technique so novel at the time that he reported the patient’s case at the 1896 annual meeting of the Canadian Medical Association. Reference Bell10

Figure 1: The Royal Victoria Hospital, 1917. Courtesy of the McCord Museum of Canadian History.

Figure 2: James Stewart. Courtesy of the McCord Museum of Canadian History.

Figure 3: James Bell. Courtesy of the McCord Museum of Canadian History.
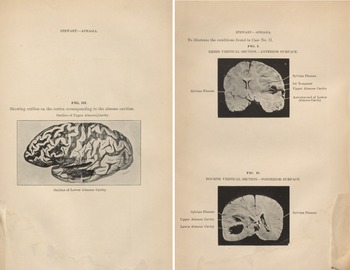
Functional Localization—The First Case Reports of Wernicke’s Aphasia in Canada
Pierre-Paul Broca had used his knowledge of the seat of articulate language to localize and operate upon a cerebral abscess in 1876. Reference Broca11 James Stewart reported two similar cases in 1900,Reference Stewart 28 not of Broca’s aphasia, but of Wernicke’s. Both patients suffered from purulent otitis media of the left ear. The first could not name objects but understood spoken and written language and could express his thoughts by writing. His ability to speak normally returned after draining of a temporal lobe abscess. The second patient had suffered from pain in the left ear for 6 months, during which ‘she seemed for a few moments to have forgotten what she wanted to say and only by an effort would she say what she wanted …When shown a pen, a key, a watch, etc., she is quite unable to recall their names either in French of English. All spoken commands appear to be clearly and perfectly understood although the response is slow.’ The patient died of respiratory failure while awaiting surgery. Autopsy revealed two abscesses within the left temporal lobe that overlay a ‘carious petrous bone.’ (Figure 4) Stewart concluded his presentation of the case by stating, ‘a form of aphasia characterized by an inability to remember the names of objects or to recollect names may arise from a destructive lesion confined to the temporo-sphenoid [temporal] lobe. This form of aphasia present in any suspected case of brain abscess, would therefore, be of value in determining its location.’ This was also true for Broca’s aphasia from brain tumors.

Figure 4: Left. Lateral (left) and frontal (right) views of Stewart’s second case showing two temporal lobe abscesses. From Stewart J. On the forms of aphasia met with in abscess of the left temporal lobe. Montreal Medical Journal. 1900; 29 (11): 829–834. Public Domain.
The First Resection of a Brain Tumor in Montreal
James Bell performed the first operation for a brain tumor in Montreal on 9 March 1901, on a patient under Stewarts’s care, who suffered from headaches and ‘temporary attacks of complete loss of speech.’ Reference Stewart29 He developed clonic seizures of the right face, a right facial droop, and weakness of the right arm and leg. The presence of continuous headaches and of bilateral papilledema, the rapid evolution of his condition, and the origin of the seizures in the face led to the diagnosis of glioma of the lower part of the precentral convolution. Reference Leblanc15 It is sobering to read that a glioma was diagnosed only after a syphilitic gumma had been eliminated because of ‘the failure of active anti-syphilitic treatment … to influence in any way favourably the disease.’
At surgery, Bell palpated a hard, resistant mass ‘over the first part of the horizontal arm of the Sylvian fissure [Broca’s area] … The brain substance over this mass was incised to the depth of a quarter of an inch, the finger introduced, and a hard, irregular tumour was enucleated and removed.’ A glass drainage tube was inserted into the cavity and remained in pace for a few days. The patient ‘rallied well after the operation.’ His speech gradually improved, as did his ability to write, and the facial weakness disappeared. Edward Archibald was Bell’s resident at the time. Archibald, who would become Canada’s first neurosurgeon, Reference Penfield30,Reference Zehri, Belykh, Zhao, Leblanc and Preul31 examined the resected specimen and observed ‘a new growth … consisting of cells fairly uniform in size, about twice that of an ordinary lymphocyte, but varying considerably in shape, some being round, others oval, pear-shaped, or even stellate. These cells lie in a very loose stroma of fibrils…. New-formed vessels are found in abundance, together with frequent small local hemorrhages.’ The center of the tumor was necrotic, ‘showing practically nothing but a tangle of neuroglial fibres, stained deep violet by Mallory’s stain.’ Based on these findings, Archibald diagnosed a tumor ‘of gliomatous nature.’ The modern reader recognizes the characteristic features of a glioblastoma multiforme, a tumor that had not yet been named.
19th Century Epilepsy Surgery at McGill
Wesley Mills, a physiologist at McGill University and a protégé of William Osler addressed the MMCS on ‘Experiments on cortical localization,’ Reference Mills32 in the cat on 22 March 1895. During the ensuing discussion, James Bell stated that he had removed ‘the hand area [of a patient], after first locating it accurately, … with the object of arresting the convulsive attacks which always began in the hand.…’ Bell does not say how localization was achieved, but one can presume that it had been by cortical stimulation, which was performed at McGill at the time. This is illustrated by a case reported by George Armstrong in 1896. Reference Armstrong33
Armstrong graduated in medicine from McGill in the same class as James Bell, whom he succeeded as Surgeon-in-Chief at the RVH upon Bell’s untimely death in 1911, from appendicitis that his colleagues had failed to diagnose. Reference Murphy34 Armstrong’s patient was an eight-year-old boy who had sustained a depressed skull fracture on the left side of the head at 15 months of age. His attacks were characterized by turning of the head and eyes to the right, and clonic movements of the right arm and leg, followed by unconsciousness.
Armstrong operated 23 October 1895 under chloroform anesthesia and elevated a bone flap centered on the posttraumatic skull defect. ‘Beneath the gap in the skull were found two thin-walled cysts, each containing about one ounce of clear fluid…. Electrical stimulation of the cerebral cortex in the floor of the cyst and also in the neighborhood failed to cause any muscular contraction.’ When asked about the strength of the current that he had used, Armstrong replied, ‘the current was too strong to be borne upon the lips.’ The resection of the cysts arrested the patient’s seizures. The chloroform may have contributed to Armstrong’s failure to generate movements by electrocortical stimulation. The other likely possibility is that he was too timid in the extent of stimulation about the cyst to reach the motor strip. The intensity of the current seems to have been adequate, as Fedor Krause in Berlin obtained motor responses with a current ‘so mild that applied to the tongue of an assistant, it was perceived by him as only a mild burning sensation accompanied by a slight acid taste.’ Reference Leblanc35
Colin Russel
Neurology and neurosurgery at McGill University made giant strides with the appointment of Colin Russel and Edward Archibald at the RVH, as designated physician and surgeon, respectively, assigned to the diagnosis and treatment of patients with neurological disorders. Colin Russel (Figure 5) graduated from McGill’s medical school in 1901. Reference McNaughton36 He interned under James Stewart and studied with William Osler at Johns Hopkins Hospital, both of whom influenced him pursuing a career in neurology. From Baltimore, Russel traveled to Zurich to study neuroanatomy and neuropathology with Constantin von Monakow, and to Berlin to study clinical neurology with Herman Oppenheim. Oppenheim was a farsighted neurologist who collaborated closely with neurosurgeon Fedor Krause. Paris followed, where Russel attended the clinics of Jules Dejerine, Pierre Marie, and Joseph Babinski. He then went to London’s National Hospital for the Paralyzed and Epileptic at Queen Square when David Ferrier and William Gowers were still active, and Victor Horsley was at his peak. It was at Queen Square that Russel first collaborated with a neurosurgeon when he analyzed the effects of Horsley’s resections within the postcentral gyrus on sensation, and established that its somatotopic organization mirrors that of the motor strip. Reference Russel and Horsley37

Figure 5: Collin Russel, neurologist-in-chief of the MNI. Photograph from the author’s collection. All rights reserved.
Influenced by Oppenheim and Krause in Berlin, and Horsley and the neurologists at Queen Square, Russel was open to a similar relationship with neurosurgery when he returned to Montreal, where he found a willing partner in Edward Archibald. Russell was appointed neurologist-in-chief at the RVH upon James Stewart’s death in 1906, where he pursued his interest in the localization of cortical function and the semiology of epileptic seizures that he had developed at Queen Square.
Alexia and Agraphia
Jules Dejerine had localized alexia and agraphia to the left angular gyrus in 1891. Reference Dejerine38 Russel had the opportunity of describing a similar case soon after his return from Europe, at the Canadian Medical Association’s 1908 annual meeting. Reference Russel39 The patient was a 59-year-old man who had a left peritonsillar abscess and headaches, papilledema, and hemianopsia. ‘He could not always remember names of people or objects … although he could understand fairly well everything that was said to him,’ Russel observed, but he could not understand what he read, nor could he express himself by writing. ‘An abscess of the brain was diagnosed and on account of the partial word deafness, complete word-blindness and the hemianopia, it was located between the angular gyrus and the posterior part of the first temporal convolution,’ as Dejerine had described. Immediate surgery was recommended, but the patient died before it could be undertaken. Autopsy revealed that Russel had been correct in his localization. And thus, Broca’s prediction that aphasia could lead the surgeon to the site of the pathology was reaffirmed.
The Dreamy State
Russel had seen a patient at Queen Square who experienced a rare manifestation of Jackson’s ‘dreamy state,’ consisting of formed visions at the start of a seizure. Reference Anderson40 Russel encountered such a patient at the RVH and reported the case – it was only the fourth such case to be reported at the time – to the MMCS. Reference Russel41 The patient was a 17-year-old woman who had episodic feelings of dread during which ‘she saw as if in a dream a woman apparently trying to save a child from drowning.’ She complained of headaches and was deaf in the left ear. Russel found that she had papilledema and had lost sensation on the left side of the face. He concluded that she had an intracranial tumor and that ‘the dreamy states points to the temporo-sphenoidal lobe.’ Surgery was limited to a decompressive subtemporal craniectomy. ‘Unfortunately, this did not give the desired relief, and the patient died in the course of a few weeks.’ A meningioma compressing the anterior and mesial temporal lobe and the Gasserian ganglion was found at autopsy, explaining the manifestations of her seizures and her sensory loss.
Edward Archibald: Canada’s First Neurosurgeon
As Stewart had discovered a kindred spirit in James Bell, so did Russel in Edward William Archibald (Figure 6). Archibald was born in Montreal in 1872 and obtained his medical degree from McGill University in 1896. Following graduation, he trained with Bell in surgery and later traveled to the clinic of Johannes von Mikulicz-Radecki, Theodor Billroth’s student and successor, in Breslau, Germany. His stay with Mikulicz, from whom he learned that ‘advances in surgery could only come from research and familiarity with the basic sciences,’ Reference Entin42 was determinant in Archibald’s future career and led him to recruit Wilder Penfield to McGill three decades later. Reference Feindel and Leblanc43 Archibald trained in neurosurgery with Bell at the RVH and with Victor Horsley at Queen Square. Bell relinquished the field to him in 1905. Russel and Archibald enjoyed a fruitful collaboration. Russel, the diagnostician, referred patients who he thought would benefit from surgery, and Archibald operated upon them. Archibald recognized the value of this collaborative effort, especially in the diagnosis, localization, and treatment of brain tumors, as he stated in his first publication: ‘I think it is important that in hospital the neurologist should be called in consultation early for … tumour cases. He may perceive the finer localizing signs which the surgeon may miss…. In these cases, we are now getting brilliant results.’ Reference Archibald44

Figure 6: Portrait of Edward Archibald. Photograph from the author’s collection.
Surgical Affections and Wounds of the Head
Archibald wrote one of the first neurosurgical textbooks in the world, entitled ‘Surgical Affections and Wounds of the Head,’ Reference Archibald, Bryant and Buck45 in 1908, which was greatly influenced by Osler’s 1889 paper advocating intracranial surgery. Despite its restrictive title, the text is comprehensive and unique among its peers in underscoring pathology and pathophysiology. Archibald is farsighted in his treatment of intracranial hypertension and brain tumors. Archibald classified gliomas into two types, based on their degree of differentiation. The more differentiated form was slow growing, had profuse astroglial fibers, and was referred to as a fibro-glioma. We would refer to such a lesion as a low-grade astrocytoma. The malignant ‘glio-sarcoma’ evolved more rapidly, was hypervascular, and subject to hemorrhagic transformation and necrosis. This tumor was later referred to as a glioblastoma multiforme. The fibro-glioma, Archibald astutely realized, could de-differentiate into a glio-sarcoma with the passage of time. As for treatment, Archibald recognized that ‘a few gliomata show some tendency to localize and their confines are easily determined: in such, operation may be attempted.’ To attempt the complete resection of a glio-sarcoma, however, was as useless as ‘to try to prevent fruit from rotting.’ Tumors of the frontal lobe were most frequently operated upon because they betrayed their location by their effect on the motor strip. The next were tumors of the cerebellum because they too were easily localized by their clinical presentation. Most often, however, the surgeon had to be content with a palliative decompressive subtemporal craniectomy, with the denuded brain covered only by the skin flap, to mitigate the effects of intracranial hypertension and the cephalocaudal shift of the brain. As for the epithelioma (meningioma), Archibald recognized it to be composed of ‘spindle cells in which lie scattered about peculiar concentrically arranged bodies called whorls.’ Archibald recognized the psammoma as a particular type of epithelioma, ‘in which microscopic whorls become calcified.’ Archibald considered epitheliomas to be eminently amenable to surgery. So were pituitary adenomas, which he was particularly adept at removing. He was also recognized for his treatment of trigeminal neuralgia. Archibald considered that Jacksonian epilepsy was often caused by a mass lesion or posttraumatic scar that could often be resected. In these cases, Archibald wrote, ‘the cortical center … in which the fits [begin] should be determined by Faradism, and the center thereupon excised to the white matter.’
The Great War
Russel’s and Archibald’s work at McGill was interrupted as they answered the call to the colors and joined the Royal Canadian Army Medical Corps in France during the First World War. Russel added neuropsychiatry to his practice as he was called upon to treat young men who had reached the limits of human endurance under fire and suffered from what the British referred to as shell shock and the Germans as grenade fever. His dedication to his patients and his pioneering work in the field earned Russel a Military Citation. Reference McNaughton36 His experience and insights were so valued that he was asked in 1919 to address the American Medical Association on the diagnosis and treatment of war neuroses. Reference Russel46
Archibald also served in France, at McGill University’s General Hospital No. 3, and in a Casualty Clearing Station in Boulogne. There he learned first-hand the effects of high velocity missiles and shrapnel on the human brain, as he wrote,
The type of head injury that reached us at the base … was, in the great majority of instances, that of the tangential wound. A man suffering from a direct hit going through and through the head rarely lived to get to the base. There were in addition a certain number of shell wounds in which the fragment, generally of small size, had penetrated the bone, and was lodged at varying depths inside the brain. These last remained without further development of serious symptoms with surprising frequency, and many were sent home to England. Reference Archibald47
It is upon such patients that Otfrid Foerster operated for posttraumatic epilepsy, and from whom Wilder Penfield learned the technique. Reference Leblanc48
The Society of Neurological Surgeons: The Birth of a New Specialty
The War had a profound effect on neurosurgery, and the need was felt, in North America, for an organization to guide its progress. Reference Cushing and Penfield49 This was the impetus that led Harvey Cushing and Ernest Sachs (a student of Osler’s at Johns Hopkins) to found the Society of Neurological Surgeons (SNS). Membership was selective and restricted to surgeons whose practice was devoted to neurosurgery. Reference Alexander, Russel and Patterson50 The SNS held its first meeting at the Brigham Hospital, Boston, in March 1920, following which Edward Archibald was invited to join. Archibald attended the Society’s meeting the following year and was appointed to the nominating committee. Archibald was an active participant in the Society’s affairs for 8 years, until his retirement from neurosurgery in favor of Penfield, whom he recruited to McGill and the RVH in 1928. Reference Feindel and Leblanc43
The Department of Neurology and Neurosurgery at McGill University
McGill offered Penfield protected time for research and laboratory accommodations in which to perform it. He and Russel were kindred spirits. It was Russel who diagnosed Penfield’s sister’s brain tumor and who accompanied her to the operating room when Penfield operated upon her. The success that Stewart and Bell and Russel and Archibald had achieved continued under Russel and Penfield. Penfield soon outgrew the facilities at the RVH and planned the construction of the MNI and the creation of an autonomous Department of Neurology and Neurosurgery that he would head, with Russel as Neurologist-in-Chief. The proposal met with the approval of the governance of McGill University and the blessings of the Heads of Medicine and of Surgery. When the MNI opened its doors in September 1934, Reference Penfield51 McGill had the only Department of Neurology and Neurosurgery on the continent.
Archibald dedicated the remainder of his career to thoracic surgery and the surgical treatment of pulmonary tuberculosis, for which he was recognized internationally. He died on 17 December 1945. Penfield marked his passing with these words: ‘I cannot close this report without paying tribute to Canada’s first neurosurgeon. Edward Archibald… It may be said that more than any other man, he created neurosurgery here and laid the groundwork for the development of the Institute… We mourn his passing and acknowledge him as the founder of this school of neurosurgery.’ Reference Penfield52 Russel worked with Penfield until the end. He died on 4 May 1956, having seen the Department and Institute that he had helped to create attain international renown. Penfield ended his eulogy with these heartfelt words at the passing of his friend, ‘God bless you, Colin Russel.’ Reference Penfield53
Conclusion
The close collaboration between physicians and surgeons in their efforts to broaden the treatment of neurological patients forged an institutional culture at McGill University that favored the creation of a comprehensive and autonomous Department of Neurology and Neurosurgery and the Montreal Neurological Institute.
Conflict of Interest
None.