Low-grade gliomas (LGGs) refer to astrocytomas or oligodendrogliomas classified by the World Health Organization as grades I or II. Reference Louis, Perry and Reifenberger1 Compared to the most aggressive glial tumors, LGGs are present in younger patients, often with minor symptoms, and have a more variable clinical course. Reference Ostrom, Gittleman and Fulop2,Reference Forst, Nahed, Loeffler and Batchelor3 Our knowledge of the genetic alterations within LGGs has dramatically increased over the past 2 decades, and current treatment paradigms generally favor surgical resection with some adjuvant therapy over “watchful waiting.” Reference Rezvan, Christine and Christian4–Reference van Veelen, Avezaat, Kros, van Putten and Vecht13 However, the optimal management of patients remains an area of active research.
The benefits of adjuvant therapies were studied in the Radiation Therapy Oncology Group (RTOG) 9802 trial which enrolled patients over the age of 40 or those with a partially resected LGG. This randomized control trial found that patients who received adjuvant procarbazine, CCNU, and vincristine (PCV) in addition to radiation therapy (RT) had longer progression-free and overall survival than those who received RT alone. Reference Buckner, Shaw and Pugh14,Reference Shaw, Wang and Coons15
Here, we present the findings of a national survey which was distributed to consultant neurosurgeons in 2020 to evaluate the current practice patterns in treatment of LGG. In addition to assessing surgeon demographics and their management strategies, we sought to evaluate the impact of the RTOG9802 trial findings on the approach to treatment.
An English-language questionnaire was created in compliance with the Freedom of Information and Protection of Privacy Act (Supplementary Figure 1). Questions were chosen in consultation with the senior authors and with reference to previously published Canadian and German surveys. Reference Khan, Mason, Kongkham, Bernstein and Zadeh16,Reference Seiz, Freyschlag and Schenkel17 Three characteristic cases and their corresponding imaging studies (Supplementary Figures 2, 3, 4) were selected from the previous studies and included in the present survey. Reference Khan, Mason, Kongkham, Bernstein and Zadeh16,Reference Seiz, Freyschlag and Schenkel17
Case 1 was a 24-year-old right-hand dominant female presenting with two generalized seizures with MRI demonstrating a left superficial frontal lobe lesion that did not enhance with gadolinium.
Case 2 was a 52-year-old right-hand dominant male with focal aware seizures with motorized aphasia and no further neurologic deficits with MRI revealing a left deep frontal lobe lesion that did not enhance with gadolinium.
Case 3 represented a 49-year-old right-hand dominant male with a history of focal unaware seizures and no neurological deficits with MRI displaying a left insular lobe lesion that did not enhance with gadolinium.
Consultant neurosurgeons in Canada were sent an invitation to complete the survey. The survey was available for 7 weeks, with reminders being sent on weeks 3 and 6. The Canadian Neurosurgical Society shared a reminder to complete the survey on Week 4. Junior and senior neurosurgeons were defined as those with < 15 and > 15 years’ experience, respectively. The survey examined the participant’s case volume, pre-operative investigations, intraoperative techniques, and the influence of the RTOG9802 findings on their practice patterns.
A total of 171 email invitations were sent to neurosurgeons in Canada. Four neurosurgeons indicated that they do not treat LGGs. Of the remaining potential participants, 40 neurosurgeons submitted their surveys resulting in a response rate of 24%.
The majority of respondents practiced in academic settings (90%, n = 36), and most respondents were senior neurosurgeons with > 15 years’ experience (60%, n = 24). Participants followed < 10 LGGs per year (35%, n = 14), between 11 and 20 (18%, n = 7) and between 20 and 50 (28%, n = 11). Notably, eight respondents followed a very high number of LGG cases (>50 patients per year). Most respondents biopsied or resected between 1 and 5 LGGs per year.
All respondents routinely determined 1p/19q status in LGG patients. Several additional biomarkers were regularly assessed including IDH status (94%, n = 29), p53 (84%, n = 26), ATRX (77%, n = 24), and IDH sequencing in select cases (74%, n = 23). Intraoperative techniques used when resecting LGGs near eloquent brain included awake craniotomy (62%, n = 21), motor evoked potentials (47%, n = 16), functional MRI (38%, n = 13), phase reversal (35%, n = 12), other (18%, n = 6), and none (18%, n = 6). Other intraoperative techniques suggested were intraoperative MRI and subcortical stimulation.
Asymptomatic patients were most often (35%, n = 12) initially managed by referral to oncology and serial imaging, while others preferred aggressive resection (25%, n = 8) and stereotactic biopsy (9%, n = 3). Symptomatic LGGs were frequently initially managed with aggressive resection (67%, n = 22) or stereotactic biopsy (12%, n = 4). Other options included referral to oncology and serial imaging.
As shown in Figure 1, the RTOG9802 trial variably impacted the approach of junior and senior neurosurgeons. Among junior consultants, 36% indicating that the trial impacted very much (n = 5), 36% somewhat (n = 5), and 29% not at all (n = 4). Senior neurosurgeons reported that the trial influenced their practice somewhat (56%, n = 10), not at all (33%, n = 6), and very much (11%, n = 2).

Figure 1: Influence of RTOG9802 study on Canadian junior (n = 14) and senior (n = 18) neurosurgeons’ approach to patients with LGGs.
Surgeons were asked to identify the factors that most affected their decision to offer adjuvant treatment. Among junior respondents, residual tumor (40%, n = 15), IDH status (26%, n = 10), age >40 years (20%, n = 8), and 1p/19q co-deletion (15%, n = 6) were most commonly reported. Senior neurosurgeons felt that the most important factors were significant residual tumor (45%, n = 20), 1p/19q status (20%, n = 9), age >40 years (18%, n = 8), and IDH mutation status (16%, n = 7).
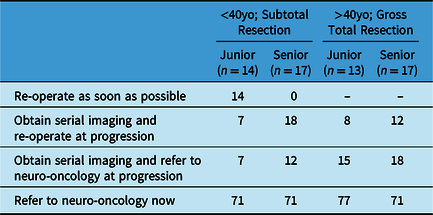
As shown in Table 1, for patients < 40 years old with a 5%–10% residual tumor after resection, most neurosurgeons would “refer the patient to neuro-oncology,” and options like “reoperation” and “serial imaging” were less commonly chosen. Similarly, for patients > 40 years old with gross total resection (GTR), most junior (77%, n = 10) and senior (71%, n = 12) neurosurgeons favored referral to neuro-oncology while others chose serial imaging and referral to neuro-oncology at progression.
Table 1: Initial approaches to patients > 40 years of age with gross total resection and < 40 years of age with subtotal resection by Canadian junior and senior neurosurgeons after the RTOG9802 publication. Values represent proportion (%) of survey respondents
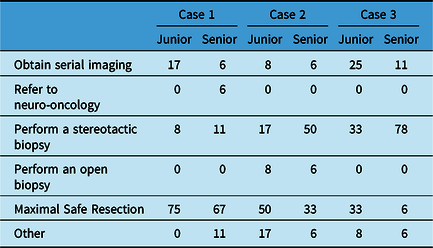
The management paradigms chosen for each characteristic case are shown in Table 2. The majority of neurosurgeons would attempt to achieve GTR for case 1, but the choices for case 2 and 3 were more variable. For case 3, 33% of junior surgeons would attempt aggressive resection (compared with only 6% of senior surgeons) while 78% of senior surgeons chose to proceed with a stereotactic biopsy.
Table 2: Initial approaches to representative LGG cases by Canadian junior (n = 12) and senior (n = 18) neurosurgeons after the RTOG9802 publication. Values represent proportion (%) of survey respondents
Respondents stated that the RTOG9802 trial had several shortcomings including 1) lack of differentiation between astrocytoma and oligodendroglioma (59%, n = 17), 2) emphasis on patient age (55%, n = 16), and 3) choice of chemotherapeutic and RT regimens. A minority (three respondents) felt that the current recommendations were appropriate.
This survey study demonstrated that the overall approach to management of LGGs and the integration of the RTOG9802 study findings into the treatment paradigm remains heterogenous. Senior neurosurgeons were less influenced by the RTOG9802 findings relative to their junior colleagues. Correspondingly, senior neurosurgeons were less likely to refer patients to neuro-oncology when indicated by the RTOG9802 protocol. Junior neurosurgeons were more aggressive in the management of LGGs with a greater preference for resection and reoperation.
Khan et al. described Canadian practice patterns in 2013 prior to the RTOG9802 study with a similar survey response rate of 25%. Reference Khan, Mason, Kongkham, Bernstein and Zadeh16 Both studies similarly demonstrated an increased propensity for more aggressive surgical management by junior neurosurgeons. This diversity in treatment choice becomes pronounced with increasing case complexity such as with lesions near eloquent brain. A previous study by Seiz et al. surveyed German neurosurgeons and predictably found that the management of simple cases is generally agreed upon, whereas challenging cases pose therapeutic dilemmas. Reference Seiz, Freyschlag and Schenkel17 However, compared with previous studies, we found that fewer neurosurgeons opt for conservative management of the presented cases. Reference Khan, Mason, Kongkham, Bernstein and Zadeh16
Unlike the study by Khan et al., our survey was restricted to practicing neurosurgeons without input from trainees. Reference Khan, Mason, Kongkham, Bernstein and Zadeh16 As such, despite having similar survey response rates, this study is strengthened by capturing the responses of those surgeons with greatest experience in the field. Furthermore, this study likely underestimates the response rate as many neurosurgeons are subspecialized, and it was not possible to determine which neurosurgeons routinely manage LGGs a priori. The current study also benefits from being able to integrate and follow up on questions utilized by previous LGG survey studies thereby enabling a direct comparison.
The RTOG9802 trial published in the New England Journal of Medicine was the first randomized trial that demonstrated progression-free and overall survival benefits in patients diagnosed with LGG treated with adjuvant chemotherapy. This study demonstrates meaningful uptake of the RTOG9802 findings by Canadian neurosurgeons, particularly by those earlier in their careers. This may be due to younger neurosurgeons relying upon clinical trials to augment their personal experience. Despite the observed differences, neurosurgeons consistently requested further elaboration of LGG management algorithms. When asked about specific areas that require further study, respondents mentioned “exploring differences between astrocytomas and oligodendrogliomas.” “re-evaluating the arbitrary patient age criterion” and “attempting to match treatment intensity with tumor aggressiveness.” The findings of this study are limited to neurosurgical practice patterns within Canada and cannot be extrapolated to an international landscape.
In conclusion, our cross-sectional study demonstrates that the findings of the RTOG study have been integrated into the practice of Canadian neurosurgeons. However, there remains heterogeneity in management preferences, especially when treating patients with lesions in eloquent areas or those patients presenting with minimal symptoms and deficits. There is a persistent desire for further personalization and risk stratification of LGGs not adequately described by the current RTOG9802 criteria. Future investigations are necessary to further differentiate the management of LGGs based upon individualized patient factors.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/cjn.2022.2
Authors’ Contributions
Mostafa Fatehi and Leeor S. Yefet contributed equally to this work. All authors made significant contributions to this manuscript. All authors contributed to the development of the survey. MF, LY, and SP identified and contacted potential participants. MF and LY analyzed the survey responses. LY wrote the initial draft of the manuscript. All authors reviewed and revised the manuscript.
Disclosures
The authors have no conflicts of interest to declare.





