The prevalence of being overweight in children under 5 years old has risen from 6·3 to 11·9 % between 1990 and 2016 in China(Reference Yang, Huang and Liu1). By 2015, China had the largest number of children with obesity aged 5 years or under in the world(Reference Di Cesare, Sorić and Bovet2). Epidemiological studies have reported that early obesity was a significant predictor of obesity later in life and the development of cardiometabolic disorders during adulthood(Reference Umer, Kelley and Cottrell3–Reference Simmonds, Llewellyn and Owen6).
Mounting evidence suggests that the first few months of life are critical for the development of obesity (Reference Gillman7). The relationships between early solid food introduction (before aged 4 months) and risk of childhood obesity have been examined previously; however, findings were inconsistent (Reference Woo Baidal, Locks and Cheng8). Several cohort studies reported that the association between the timing of solid food introduction and adiposity varied by milk feeding status (formula fed or breastfed)(Reference Huh, Rifas-Shiman and Taveras9–Reference Moss and Yeaton11). They found the effects of early solid food introduction on later obesity were more significant in formula-fed infants. Infant formula was usually introduced earlier than solid food. A population-based birth cohort study of China, involving 98 097 maternal–infant pairs, showed that in the first month, infant formula exposure rate was 58·8 %; in the third month, the exposure rate was 66·6 % and in the sixth month, the exposure rate reached up to 72·0 % (Reference Yang, Mei and Mei12). The association between formula feeding practice and excess weight gain in early childhood has been examined (Reference Appleton, Russell and Laws13). The explored mechanisms included overfeeding formula, putting a baby to bed with bottle, and compositions (higher protein) in formula (Reference Appleton, Russell and Laws13). However, to our knowledge, there were no studies primarily focusing on the association between the timing of infant formula introduction and early growth. Though cessation of exclusive breast-feeding is essentially correlated with the introduction of infant formula, it is also related to the introduction of solid foods. Therefore, it is necessary to examine the effects of the timing of infant formula and solid food introduction on later growth separately.
This study has examined the hypothesis that the introduction of infant formula at early stage is associated with a higher risk of overweight in early childhood while considering the timing of solid food introduction and breast-feeding duration in a large-scale prospective birth cohort.
Methods
Study population
This is a longitudinal study on singleton births between February 2012 and December 2015 in the Born in Guangzhou Cohort Study (BIGCS), a large-scale prospective observational study in Guangzhou, China. Pregnant women were recruited before 20 gestational weeks from two campuses of Guangzhou Women and Children’s Medical Center (GWCMC) from February 2012. Details of the BIGCS cohort with full inclusion and exclusion criteria can be found in the published protocol(Reference Qiu, Lu and He14). This study was approved by the Institutional Ethics Committee of the GWCMC. All participants signed a consent form at the time of recruitment. The baseline questionnaire was completed before week 20 of pregnancy. Follow-up of the children took place at paediatric clinics at the age of 6 weeks, 6, 12 and 36 months after birth and involved questionnaires (completed by the mother or guardian) and physical examinations. Although those who were unable to attend the appointments in person were interviewed on the telephone, they were excluded from the present analysis due to the lack of information on anthropometric measurements. Children with incomplete feeding data were also excluded (Fig. 1). In addition, all analyses were performed by restricting to full-term (≥ 37 weeks) infants with normal birth weight (≥ 2500 and < 4000 g).
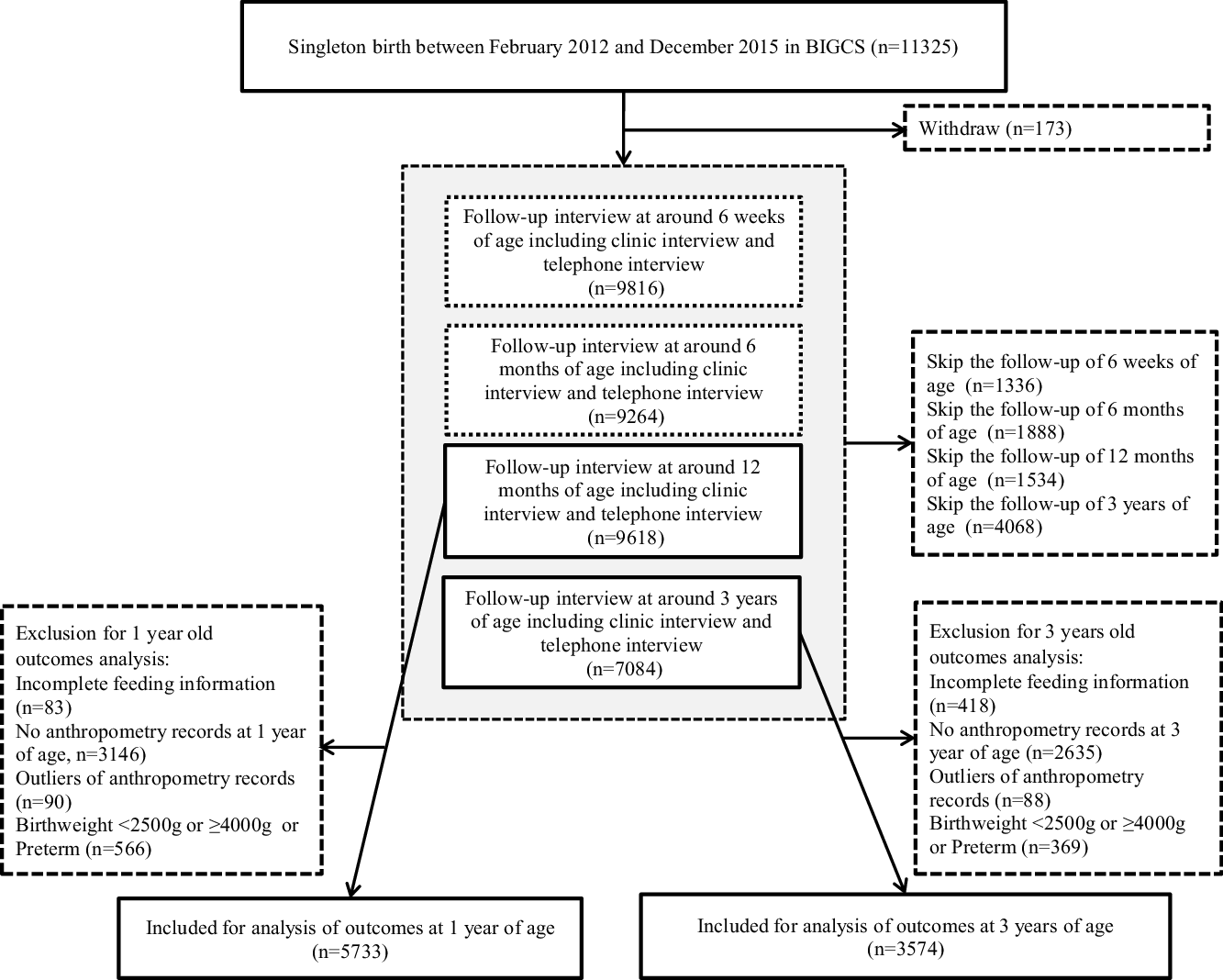
Fig. 1. Flow chart of the study population.
Exposures
Feeding information
The age of first introduction of infant formula and other food and duration of breast-feeding were defined from several variables reported in the self-administered questionnaire at the age of 6 weeks as well as at 6, 12 and 36 months. At each time point, if the response to the question ‘Has your child been fed infant formula?’ was affirmative, the mother was asked to state the type of infant formula (standard cow’s milk formula, hydrolysed formula, preterm formula, other types of formulas) and the age when the child first had the infant formula. If the child has been fed any food other than milk (cereal, rice porridge, vegetables, fruits, meat, offal, fish, other seafood, egg yolk, egg white), the age when he/she first ate the food was recorded and taken as the age of solid food introduction.
Infant outcomes
Anthropometric measurements were undertaken at each follow-up visit by trained fieldworkers. Abdomen circumference and upper arm circumference (cm) were measured in a supine position using a measuring tape to the nearest 0·1 cm. Length (cm) was measured in a supine position using a length board (Shekel Healthweigh™) to the nearest 0·1 cm. Body weight (kg) was measured without shoes and with light clothing (single layer) in a supine position using a stadiometer (Shekel Healthweigh™) to the nearest 0·01 kg. To account for additional weight due to clothes worn, 200 g was subtracted from the weight of each child. BMI was calculated using the formula kg/m2. Children’s sex- and age-specific z-scores of BMI were calculated using a SAS (WHO-source-code.sas) based on the 2006 WHO growth standards(15). According to the WHO classifications for overweight and obesity in younger children (0–5 years), at-risk of overweight was defined as BMI-for-age z-score above +1 sd and less than +2 sd, overweight was defined as above +2 sd and less than +3sd and obesity was defined as above+3 sd (Reference de Onis and Lobstein16). Since the number of children with overweight and obesity was insufficient for reliable analyses, these high BMI statuses were analysed as a single category in this study (overweight). Z-scores for a child’s sex and age for weight and height (length-for-age z-score, weight-for-age z-score, weight-for-length z-score) based on the WHO Growth Charts were also calculated. The cut-offs for extreme z-scores (biologically implausible values) were used as <–5 and >5 according to the WHO criteria (15). The extreme values were excluded from data analysis.
Covariates
Socio-demographic characteristics and potential confounders, including maternal age, maternal educational level, maternal smoking and passive smoking status during pregnancy, maternal pre-pregnant BMI, paternal BMI and other health-related factors, were obtained by the baseline questionnaire before 20 weeks of gestation. Obstetrics-related variables, including delivery date, mode of delivery, gestational age, birth weight and infant sex, were extracted from the hospital clinical records.
Statistical analysis
All statistical analyses were performed using SAS software, version 9.4 (SAS Institute). The timing of infant formula introduction was categorised into three groups, including ≤ 3, 4–6 and > 6 months or never received infant formula during the study period. The participants’ characteristics were stratified by the timing of infant formula introduction (≤ 3, 4–6 and > 6 months). The information on characteristics was presented as mean values and standard deviations for continuous variables or as percentages for categorical variables. The overall associations of timing of infant formula introduction with abdomen circumference, upper arm circumference, BMI z-score, length-for-age z-score, weight-for-age z-score and weight-for-length z-score were analysed with linear regression models and presented as β and 95 % CI. The associations between timing of infant formula introduction and risk of overweight were analysed with logistic regression models and presented as OR and 95 % CI. Results were adjusted for potential confounders including maternal age at delivery (≤ 25, 26–30, 31–35, > 35 years of age), maternal education (high school or below, vocational/technical college, undergraduate, postgraduate), maternal pre-pregnancy BMI and paternal BMI (< 18·5, 18·5–23·9, 24–27·9, ≥ 28 kg/m2)(Reference Chen and Lu17), maternal smoking during pregnancy (yes, no), passive smoking during pregnancy (yes, no), parity (primiparous, multiparous), mode of delivery (vaginal labour, caesarean delivery), birth weight (g, continuous value), infant sex, the duration of breast-feeding (0–6, > 6 months) and age at first introduction to solid foods (≤ 3, 4–6, > 6 months). For the analysis of children’s length-for-age and weight-for-length z-scores, maternal and paternal heights were also adjusted. A two-tailed P value < 0·05 was considered statistically significant. Furthermore, a sensitivity analysis was performed by only including the children with longer breast-feeding duration (> 6 months), because the longer duration of breast-feeding was associated with a lower risk of excess weight gain during early life(Reference Zheng, Cameron and Birken18).
Given the proportion of missing data on confounder variables was from 0·1 to 10·3 %, analyses based on complete cases may be biased. Thus, we used multiple imputation (MI) analysis to cope with missing data (Reference Sterne, White and Carlin19). We used the fully conditional method iterative method for imputation using SAS version 9·4. The following variables were imputed: pre-pregnancy BMI, paternal BMI, maternal smoking during pregnancy, passive smoking during pregnancy, parity, mode of delivery, the duration of breast-feeding and the timing of introduction of any solid food. For the analysis of children’s length-for-age and weight-for-length z-scores, maternal and paternal heights were also imputed. Exposure and outcome variables of each model were considered as observed covariates and used in the models to impute these variables. For each imputation model, ten imputations were run. We ran a procedure called proc mianalyze which combines all the estimates (coefficients and standard errors) across all the imputed data sets and outputs one set of parameter estimates for the model of interest (20). The fraction of missing information analysis was performed to determine potential efficiency gains from MI (see online Supplementary Table S1 and Table S2). Values of fraction of missing information range between 0 and 1. A smaller fraction of missing information (close to 0) indicates low variability between imputed data sets, which means observed data in the imputation model provide much information about the missing values (Reference Madley-Dowd, Hughes and Tilling21).
Results
Characteristics of the study population
Characteristics of the participants included in the 1-year analysis based on the three infant formula introduction groups are shown in Table 1. Compared with infant formula introduction at 0–3 months group, the mothers in infant formula introduction after 6 months group were more likely to be younger and primiparous. The children in the later introduction group were more likely to be female, breastfed longer than 6 months and introduced to solid food later. For the population included in the 3-year analysis, compared with the mothers who introduced formula feeding at 0–3 months, those who introduced formula after 6 months group were more likely to be better educated and multiparous but experience higher levels of passive smoking during pregnancy. The children receiving formula later were, as expected, more likely to be breastfed longer than 6 months and be introduced to solid food later (see online Supplementary Table S3). Characteristics of included and excluded participants of this study are also shown in online Supplementary Table S4. Compared with excluded population, included children were more likely to have higher educated and multiparous mothers, higher birth weight and earlier formula introduction.
Table 1. Baseline characteristics of participants in different timing of infant formula introduction groups in the Born in Guangzhou Cohort Study (BIGCS) study
(numbers and percentages; mean values and standard deviations)

* The children who had never received infant formula during the study period were combined into > 6 months group.
Table 2 shows the anthropometric outcomes including abdomen circumference (cm), upper arm circumference (cm), BMI, the prevalence of at-risk of overweight and overweight, at 1 and 3 years old, respectively. The means of BMI at 1 year and 3 years old were different between the three infant formula introduction groups. The differences also existed in the prevalence of at-risk of overweight at 1 and 3 years old between these groups. Furthermore, we provided the proportions of children were introduced to infant formula at each month after birth, including who had never received formula by 3 years in online Supplementary Table S5.
Table 2. Anthropometric outcomes in different timing of infant formula introduction groups in the Born in Guangzhou Cohort Study (BIGCS) study
(numbers and percentages; mean values and standard deviations)

* The children who had never received infant formula during the study period were combined into >6 months group.
Timing of introduction of infant formula and anthropometric outcomes
Table 3 presents the associations between the timing of infant formula introduction and anthropometric outcomes at 1 and 3 years of age. Compared with formula introduction within the first 3 months, introduction at 4–6 months was associated with lower upper arm circumference (adjusted β − 0·15, 95 % CI − 0·26, −0·05), BMI z-score (adjusted β − 0·18, 95 % CI −0·26, −0·09), length-for-age z-score (adjusted β − 0·09, 95 % CI − 0·17, −0·01), weight-for-age z-score (adjusted β − 0·21, 95 % CI − 0·29, −0·13) and weight-for-length z-score (adjusted β − 0·19, 95 % CI − 0·27, −0·10) at 1 year of age in MI models. Compared with formula introduction at 0–3 months, introduction after 6 months was associated with lower length-for-age z-score (adjusted β − 0·08, 95 % CI − 0·17, 0·00) and weight-for-age z-score (adjusted β − 0·10, 95 % CI − 0·18, −0·01).
Table 3. Linear regression models to evaluate the associations between timing of formula introduction and anthropometric outcomes at 1 and 3 years of age (before and after multiple imputation)
(β-coefficients and 95 % confidence intervals)

MI, multiple imputation.
* Adjusted for maternal age at delivery, maternal education, maternal pre-pregnancy BMI and paternal BMI, maternal smoking during pregnancy, passive smoking during pregnancy, parity, mode of delivery, infant sex, birth weight, the duration of breast-feeding and age at first introduction to solid foods.
† Adjusted for maternal age at delivery, maternal education, maternal pre-pregnancy BMI, maternal height, paternal BMI, paternal height, maternal smoking during pregnancy, passive smoking during pregnancy, parity, mode of delivery, infant sex, birth weight, the duration of breast-feeding and age at first introduction to solid foods.
‡ Adjusted P values for multiple imputation models.
§ The children who had never received infant formula during the study period were combined into > 6 months group.
For 3 years outcome, compared with infant formula introduction within the first 3 months, introduction at 4–6 months of age was associated with lower BMI z-score (adjusted β − 0·14, 95 % CI − 0·24, −0·03), weight-for-age z-score (adjusted β − 0·11, 95 % CI − 0·21, −0·01) and weight-for-length z-score (adjusted β − 0·14, 95 % CI − 0·25, −0·04) in MI models (Table 3).
Timing of introduction of infant formula and weight statuses during the first 3 years
Compared with infant formula introduction within the first 3 months of life, introduction at 4–6 months was associated with the lower odds of at-risk of overweight at 1 year (adjusted OR 0·73, 95 % CI 0·55, 0·95) and 3 years old (adjusted OR 0·52, 95 % CI 0·31, 0·87) in MI models (Table 4). Infant formula introduction at 4–6 months was associated with a lower risk of overweight at 1 year old (adjusted OR 0·43, 95 % CI 0·22, 0·85), but the association was not significant for overweight at 3 years of age (adjusted OR 0·45, 95 % CI 0·14, 1·47). These findings were similar when we restricted the analysis to children with longer breast-feeding duration (> 6 months) (see online Supplementary Table S6).
Table 4. Logistic regression models to evaluate the associations of the timing of formula introduction with at-risk overweight and overweight at 1 and 3 years of age
(numbers and percentages; odds ratios and 95 % confidence intervals)

MI, multiple imputation.
Adjusted for maternal age at delivery, maternal education, maternal pre-pregnancy BMI and paternal BMI, maternal smoking during pregnancy, passive smoking during pregnancy, parity, mode of delivery, infant sex, birth weight, the duration of breast-feeding and age at first introduction to solid foods.
* P values for multiple imputation models.
† The children who had never received infant formula during the study period were combined into > 6 months group.
Discussion
Results of this prospective longitudinal cohort indicated that compared with infant formula introduction within the first 3 months, introduction at 4–6 months was associated with the lower z-scores for BMI, weight-for-age and weight for length at ages 1 and 3 years. We also found that later formula introduction at 4–6 months of age was associated with the lower odds of at-risk of overweight at 1 and 3 years of age and decreased odds of overweight at the age of 1 year but not at the age of 3 years. However, no significant association was observed between later introduction of formula after 6 months and the risk of overweight at ages 1 or 3 years.
Previous studies examining the associations between the timing of solid food introduction and risk of overweight or obesity found that the effects of the timing of solid food introduction on later development of obesity were different between breastfed and formula-fed infants (Reference Huh, Rifas-Shiman and Taveras9,Reference Moss and Yeaton11) . These results suggested the effects of solid food introduction on later weight status may be affected by formula feeding. However, studies focusing on examining the effects of timing of infant formula introduction on later overweight or obesity are limited. A longitudinal cohort study indicated that the risk of overweight or obesity was significantly higher among infants who were introduced to infant formula or solids during the first 4 months of life compared with those introduced later (Reference Mannan22). Nevertheless, they did not distinguish the effects between solid and infant formula introduction. Infant formula usually was introduced to infants much earlier than other solid foods. In our study population, over 80 % infants were introduced to infant formula within the first 3 months of life, highlighting that infant formula is widespread used in this urban area of China. We found that infants who were introduced to infant formula at 4–6 months of age were more likely to have lower BMI, weight-for-age and weight-for-length z-scores at both 1 and 3 years old than those introduced earlier (≤ 3 months), independent of the timing of solid food introduction.
Potential mechanisms of infant formula introduction at early stage on later weight status might be associated with the immature intestinal ecosystem and immune system during the first few months of life. The establishment and interactive development of early gut microbiota are driven and modulated by specific compounds present in breast milk(Reference Milani, Duranti and Bottacini23). Evidence showed that the Bifidobacteria and Lactobacillus were predominant in breastfed infants, whereas the Ruminococcus was predominant in formula-fed infants(Reference O’Sullivan, He and McNiven24). In children, a high concentration of Bifidobacteria during the early stage of life has been reported to have protective effects on later obesity (Reference Kalliomäki, Collado and Salminen25). The bacteria in the gut ferment dietary fibres into SCFA, whose interaction with G-protein-coupled receptors influences insulin sensitivity in several tissues, including liver, muscle and adipose tissue, thus regulating energy metabolism(Reference Pihl, Fonvig and Stjernholm26). Therefore, the introduction of infant formula at early stage of infancy might influence the composition and ecosystem of the gut microbiome, which links to the development of childhood overweight or obesity. Furthermore, infant formula feeding induces uncontrolled excessive protein intake, which overacts the infant’s mammalian target of rapamycin complex 1 (mTORC1) signalling pathways(Reference Melnik27). Overactivated mTORC1 enhances S6K1-mediated adipocyte differentiation. Thus, early formula feeding is considered to be associated with the development of mTORC1-driven metabolic disease, including obesity (Reference Melnik27).
In our study, no significant differences in outcomes between ≤ 3 and > 6 months formula introduction groups were observed. The recommended timing for solid foods introduction is not earlier than 4 months or later than 6 months of life (Reference Jones, Lee and Brown28). Late solid food introduction (≥ 7 months of age) was found to be associated with an increased risk of later childhood overweight/obesity among exclusively breastfed children (exclusive breast-feeding over 6 months)(Reference Papoutsou, Savva and Hunsberger29). After 6 months of age, it is difficult to distinguish the impacts of later introduction of infant formula or solid foods on weight status. Formula feeding and complementary feeding might be not independent decisions and may jointly explain variances in later obesity.
Although breast milk is recommended for all infants, preterm formulas are alternative sources of enteral nutrition for preterm or low birth weight infants when sufficient maternal breast milk and donor human milk are not available(Reference Hay and Hendrickson30). In addition, the association between feeding practice and excess weight during the early stage might be modified by birth weight(Reference Goetz, Mara and Stark31). Therefore, we performed the analysis by limiting it to full-term infants with normal birth weight.
Mothers participating in BIGCS are likely to be more affluent, older and have higher education than the contemporary pregnant women in Guangzhou, hence limiting the generalisability of the findings(Reference Qiu, Lu and He14). However, in this study, a relatively widespread across all socio-economic status indicators can be still observed within the participants of BIGCS, hence enabling us to explore the differences in health consequences across different socio-economic status strata. Our data showed that a large proportion of infants were given infant formula as a supplement to breast milk (mix feeding) during the early months of life. And the main findings of this study remained significant in children with longer breast-feeding duration (over 6 months), though the longer breast-feeding was suggested to protect against subsequent obesity (Reference Zheng, Cameron and Birken18). The aggressive marketing for infant formula and other breast milk substitutes has influenced the parents’ preferences in China(Reference Tang, Lee and Binns32). A study reporting the factors associated with Chinese mothers’ decision to formula feeding showed that the majority of women choosing formula feeding thought they had insufficient breast milk(Reference Zhang, Tang and Wang33). The authors also found that some mothers had the belief that formula is more nutritious than breast milk(Reference Zhang, Tang and Wang33). This belief has also been described in some studies from other countries(Reference Sheehan, Schmied and Cooke34,Reference Bonia, Twells and Halfyard35) . In addition, child-related factors, such as weight and appetite in early life, can influence the parental feeding practices. A cohort study from the UK reported that mothers of lower birth weight or lower appetite infants, or those perceiving their children are at-risk of underweight tend to overfeed the infant in order to achieve greater weight gain(Reference Fildes, van Jaarsveld and Llewellyn36). The government and health professionals should provide more information on the differences in health benefits between breast milk and infant formula to let the parents understand that there is no better early food than breast milk for their young infants during the early stage.
One strength of our study is the longitudinal study design with a large number of participants, which enabled us to measure the associations with adequate statistical power. A further strength is the repeated assessment of feeding practice, at 6 weeks, 6 and 12 months, allowing specific descriptions of feeding patterns during infancy. A wide range of confounders was adjusted or controlled for in our MI models while assessing our exposure–outcome relationship. However, the associations might be confounded by some potential factors for which we did not adjust, such as the amount and the duration of infant formula consumption. Limitations of this study should be considered. First, the population size in 3 years age group was smaller than 1 year age group. Thus, there was a relatively lower power to detect differences at 3 years of age as opposed to 1 year of age. Second, the assessment of feeding practices was based on parental self-report, but recall of infant feeding practices is regarded as sufficiently accurate(Reference Launer, Forman and Hundt37). Third, a proportion of the cohort did not have anthropometry measured at 1 (37 %) and 3 (51 %) years, which limits the generalisability of our findings. In addition, a lower proportion (71·8 %) of children without anthropometry data at 1 year were introduced to formula within the first 3 months, compared with that of those with anthropometry data (82·2 %) (see online Supplementary Table S3). Based on our findings, it is possible that the included population is at a higher risk of overweight than those in the full cohort due to the higher proportion of children who have infant formula exposure at early stage. However, it is difficult to specify whether this difference would affect the associations that we found due to the absence of outcomes in the excluded population. Therefore, these results need to be replicated in other cohort studies before more firm recommendations can be made. Fourth, the information on the specific quantity of infant formula and solid food introduced was absent in this analysis. We also have no information on whether the consumption of infant formula was sustained after the introduction. Further evidence is needed to explore the short-term and long-term effects of the timing and quantity of infant formula introduction on the risk of overweight or obesity in later life.
Conclusion
Overall, compared with infant formula introduction within the first 3 months, introduction at 4–6 months was associated with the lower z-scores for BMI, weight-for-age and weight for length at both 1 and 3 years old. Also, introduction after 3 months was associated with decreased odds of at-risk overweight at the ages of 1 and 3 years. Although the results need to be replicated in other well-designed studies before more firm recommendations can be made, avoiding unnecessary infant formula introduction, particularly in the first 3 months, should be promoted to reduce the possibility of excess or rapid weight gain during early childhood.
Acknowledgements
We are grateful to all the families who took part in this study and the whole Born in Guangzhou Cohort Study team, which includes interviewers, research scientists, nurses, computer and laboratory technicians, clerical workers and volunteers.
This study was supported by the Guangzhou Municipal Science and Technology Bureau, Guangzhou, China (grant number: 201807010086) and National Natural Science Foundation of China (grant numbers 81673181, 81703244 and 81903311).
M. Y., G. N. T., X. Q. and K. K. C. conceived the study design; M. Y., M. L., Y. G., J. L., J. H., S. S. and D. W. collected the data; M. Y. conducted the data analysis and wrote the initial manuscript. Y. G., J. L., K. B. H. L. and J. H. assisted with the statistical analysis. All authors contributed to data interpretation and the writing of the manuscript and critically reviewed and approved the final manuscript.
There are no conflicts of interest.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S000711452200071X








