Introduction
Population ageing, chronic diseases and unhealthy lifestyles are among the greatest challenges governments have to address. It is estimated that the older population, which in 2015 represented 8.5% of the world population (617.1 million), will double in the next 25 years (He et al., Reference He, Goodkind and Kowal2016). About 20% of the European population is aged 65 and over (OECD/EU, 2018). As people live longer, they are more likely to develop chronic diseases, which result in deaths that are “double that of all infectious diseases, maternal and perinatal conditions, and nutritional deficiencies combined” (WHO, 2005). Being overweight and obese are recognized as major risk factors for diabetes, cardiovascular diseases and cancer. The prevalence of obesity has increased globally (Malik et al., Reference Malik, Willett and Hu2013) and in almost all European countries since 2000 (OECD/EU, 2018). The rate of increase among the young is higher than among adults (Lobstein et al., Reference Lobstein2004; Wabitsch et al., Reference Wabitsch, Moss and Kromeyer-Hauschild2014; GBD 2015 Obesity Collaborators, 2017). It is estimated that 23% of adults and 81% of adolescents in the world are not sufficiently active (WHO, 2018) and that dietary habits are unhealthy and inappropriate, especially in families of low socioeconomic status. Despite efforts in the health promotion and prevention fields, societies still need more protection from preventable diseases (OECD/EU, 2018) by promoting healthy lifestyles and supporting people in managing their health and disease.
Evidence on the effectiveness of the existing interventions aimed at changing individual behaviour is mixed (Davis et al., Reference Davis2015; Matjasko et al., Reference Matjasko2016; Laverack, Reference Laverack2017). There are concerns over the magnitude of the impact on populations as a whole and individual adherence to programmes, especially following the termination of interventions (Middleton et al., Reference Middleton, Anton and Perri2013; De Poli et al., Reference De Poli2018). Changing behaviour is typically a complex process requiring continuous individual engagement over a long period of time (Prochaska et al., Reference Prochaska, DiClemente and Norcross1992; Bowles, Reference Bowles2016; Matjasko et al., Reference Matjasko2016). There are proposals to use behavioural economics (BE) tools to improve the design, implementation and efficacy of public health interventions (Cialdini et al., Reference Cialdini, Martin and Goldstein2015; Matjasko et al., Reference Matjasko2016; Public Health England, 2018). In fact, BE recognizes the limitations of the classical rational choice model of individuals’ behaviour (Just & Payne, Reference Just and Payne2009; Thaler & Sunstein, Reference Thaler and Sunstein2009; Kahneman, Reference Kahneman2012).
To enhance the efficacy of preventative interventions directed towards behavioural change, the ‘nudge’ approach of Thaler and Sunstein is popularly seen to be what BE can offer. ‘Nudges’ are actions aimed at changing the choice architecture of individuals, making the ‘right’ choices more appealing to ‘quick thinking’ (Kahneman, Reference Kahneman2012) than the ‘wrong’ ones. From 2010, the UK Behavioural Insights Team has worked to apply this method in several public domains, collecting evidence on the effectiveness of the proposed approach. Researchers have begun developing and specifying how and when it is proper to apply nudges. In particular, Oliver (Reference Oliver2013) showed that the work of Nudge Units could be categorized along three different continuums: liberty of action; behavioural or rational model of reference; and orientation towards tackling internalities or externalities related to the targeted behaviours. Three categories of actions result from this analysis: ‘nudges’ (as above); ‘shoves’, which are more forceful than ‘nudges’ and imply explicit regulations limiting individuals’ behaviour (e.g., a ban on selling sugary beverages inside schools); and ‘budges’, which are regulatory interventions aimed at reducing negative externalities that result from individual choices (e.g., regulating cigarette advertising to avoid consumer manipulation; Oliver, Reference Oliver2013, Reference Oliver2015). The first two are based on a paternalistic approach that represents the belief that it is possible “to motivate behaviour change among those who, on reflection, would have liked to have made different choices for themselves” (Oliver, Reference Oliver2015). Nudges and shoves generally address internalities (i.e., choice-related benefits for the individual who chooses), while budges are built to avoid the negative externalities resulting from incorrect individual behaviours (e.g., to avoid the burden of cost of managing choosers’ obesity at the system level; Oliver, Reference Oliver2015).
BE tools tend to focus on individual cognitive biases rather than cultural orientation and social network dynamics (Leggett, Reference Leggett2014; Davis et al., Reference Davis2015; Van Der Linden, Reference Van Der Linden2018), which constantly influence people's choices (Boudon, Reference Boudon1981; Bourdieu & Passeron, Reference Bourdieu and Passeron1990; Weber, Reference Weber1999; Täube, Reference Täube2004; Barden, Reference Barden and Samson2015). Adding this broader perspective to the redesign of preventative interventions can enhance their effectiveness (Cialdini et al., Reference Cialdini, Martin and Goldstein2015; Public Health England, 2018; Van Der Linden, Reference Van Der Linden2018).
Redesigning services and the actors’ role
This paper proposes a framework with principles that are useful for improving the design and implementation of health promotion and preventative interventions in terms of the magnitude and duration of their impact (Figure 1). An alternative model of managing health promotion services and practices is proposed on the basis of a rethinking of the roles of health professionals and people in general, based on a collaboration between them.
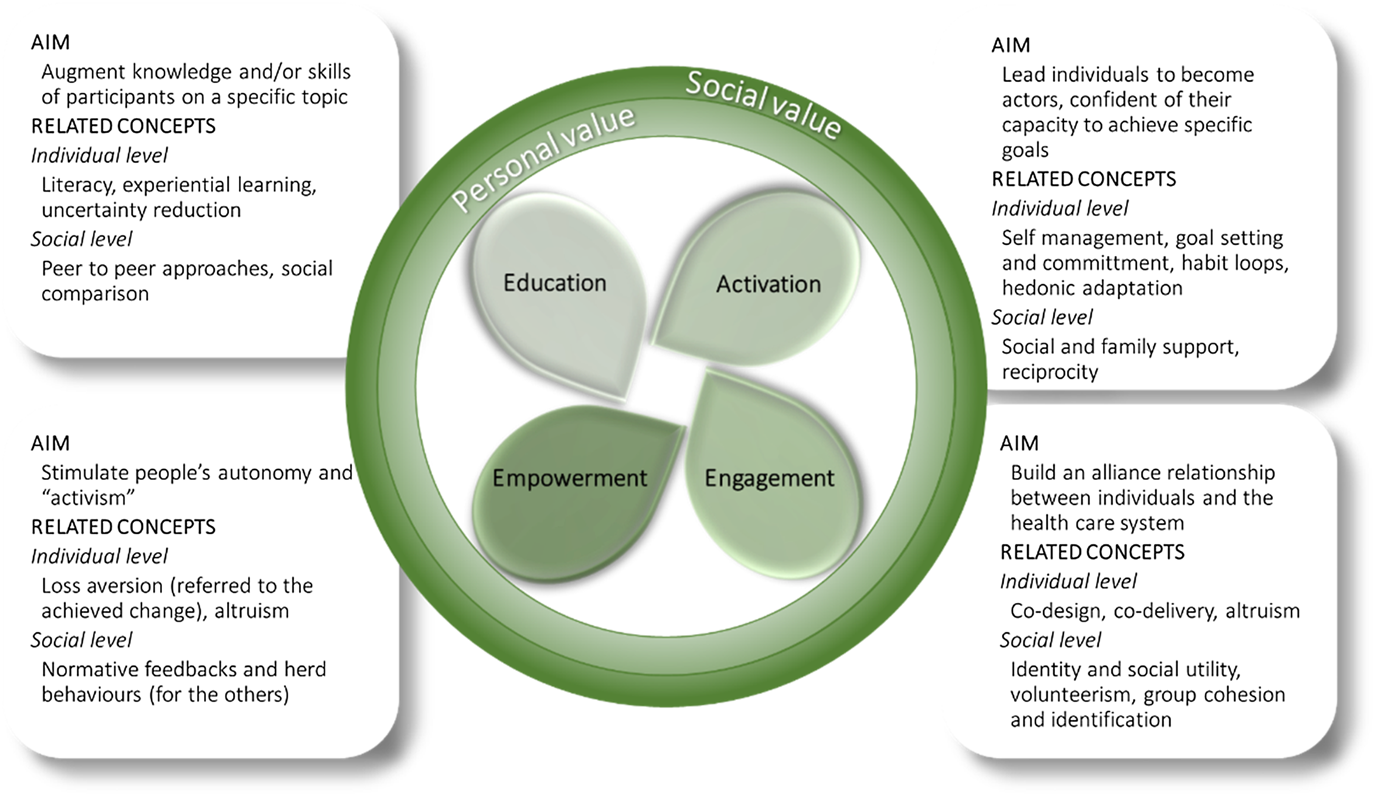
Figure 1. Framework for improving the design and implementation of health promotion and preventative interventions.
The authors propose that improving health outcomes and creating broader individual and collective value from preventative actions require a programme organized around behavioural and social mechanisms and inspired by some or all the principles of education, activation, engagement and empowerment.
The aim of education is to increase people's amount of knowledge and/or skills. To be effective, it needs to be more than simply about conveying information passively (Middleton et al., Reference Middleton, Anton and Perri2013; Laverack, Reference Laverack2017), such as experiential and social learning (Knowles, Reference Knowles1989; Dudley et al., Reference Dudley, Cotton and Peralta2015). It has been demonstrated that group-based interventions are more effective than individual-based ones, even when participants expressed their preference for individual treatments (Middleton et al., Reference Middleton, Anton and Perri2013). Education also needs to be designed to make people aware of their cognitive limits and to teach them how to counteract such limits (Battersby & Bailin, Reference Battersby and Bailin2013; Croskerry, Reference Croskerry2013).
Active individuals develop confidence in their capacity to achieve health goals (Hibbard et al., Reference Hibbard2007) and achieve positive outcomes in health interventions more often (Mosen et al., Reference Mosen2007); this includes the efficient and appropriate use of resources, improvements in quality of care, etc. (Hibbard & Greene, Reference Hibbard and Greene2013; Lorig et al., Reference Lorig2016a). Furthermore, active individuals have greater awareness of their sociocultural context and are therefore able to better control day-to-day behaviours, in addition to self-management, commitment to applying practical knowledge and sticking to pursuing behavioural goals. Professionals can enable this process of activation through social mechanisms, such as through social learning and peer influences or raising awareness of social responsibility stemming from the broader consequences of an individuals’ behaviour (Cialdini et al., Reference Cialdini, Martin and Goldstein2015).
Engagement involves building strong relationships among individuals and with the health care system (NICE, 2016). For example, professionals could collaborate with past participants of interventions to improve their design and deliver them together (i.e., past participants would act as peer workers or peer promoters). These practices of co-design and co-delivery are among the most effective ways of engaging laypeople in active participation (Bovaird & Loeffler, Reference Bovaird and Loeffler2014; Osborne et al., Reference Osborne, Radnor and Strokosch2016; Vink et al., Reference Vink2016). Engagement can be enhanced by using mechanisms such as identity and social utility, goal framing and pre-commitment to feel involved and willing to invest time and energy in actively participating (Samson, Reference Samson2015).
Empowerment builds autonomy and ‘activism’ (Wallerstein, Reference Wallerstein1993; De Vos et al., Reference De Vos2009). The idea is that the appraised knowledge, the collected experiences and the social networks that have been developed become resources that participants will rely on to maintain the effort required to improve their habits and to participate in community actions. The increased sense of control enhances the diffusion of ‘positive’ herd behaviours and habits at the community level. Therefore, participants in health promotion interventions can become members of social networks that encourage them to continue adhering to the programme, to sustain them and to contribute to their redesign (Wallerstein, Reference Wallerstein1993).
In an ideal process, which would go from a first phase of education to a fourth and final stage of empowerment in a ‘linear’ fashion, professionals help participants understand what knowledge is needed to become active and engaged in the system, to feel empowered and to maintain what they have learned in their everyday lives (Middleton et al., Reference Middleton, Anton and Perri2013). However, in actuality, these four phases and principles are not mechanically applied to the interventions, which are designed with some phases either collapsed or skipped. Indeed, people are often involved in only one or two of the four phases of the ideal framework.
This paper presents three action research projects (Adelman, Reference Adelman1993; Whitehead et al., Reference Whitehead, Taket and Smith2003) as examples of reframing a health promotion intervention to work better in terms of impact and adherence over time by paying attention to social and cultural elements in well-identified target populations: teenagers (Case 1); chronic patients (Case 2); and elderly people (Case 3). The specific overall goals of each intervention were: promotion of healthy lifestyles in Case 1; self-management of type 2 diabetes in Case 2; and promotion of physical activity in Case 3. The three experiences were implemented in Italy, mainly by the Tuscany Regional Health System (TRHS), with the collaboration of Laboratorio Management e Sanità (Pisa, Italy) research teams.
In the last 10 years, the region of Tuscany has put considerable effort into promoting healthy behaviours across its population with targeted campaigns and interventions directed at improving the management of chronic patients by adopting the Chronic Care Model (Wagner, Reference Wagner1998; Glasgow et al., Reference Glasgow, Orleans, Wagner, Curry and Solberg2001). At the local level, three Local Health Authorities (LHAs) are in charge of the health promotion/prevention and care for Tuscany's 3.7 million inhabitants. Health promotion is a responsibility of the local Department of Prevention of each LHA, and chronic care is delivered by general practitioners (GPs), who act as both the patients’ gatekeepers to specialist care and the providers of primary care (including health promotion and prevention, as well as follow-up of chronic conditions). GPs are not employees of the TRHS, but work as independent contractors; they are generally paid by capitation.
The beFood case
In the Italian population aged from 2–19 years, obesity affects 7.24% of males and 5.86% of females, and the prevalence rates of being overweight are 21.00% and 16.75%, respectively (GBD 2015 Obesity Collaborators, 2017). In 2015, the proportion of overweight adolescents in Tuscany was more than 12% (Agenzia Regionale di Sanità della Toscana, 2015). Obesity in younger populations has increased in the last 10 years by 1.5%, affecting 3.1% of Tuscan teenagers.
In response to these increases in prevalence, several policies have been adopted to prevent the young population from becoming obese and overweight. There is, however, contradictory evidence regarding the effectiveness of interventions targeted at young people (Wijtzes et al., Reference Wijtzes2017). This is because social environment- and network-related factors appear to be crucial in reaching the goals of initiatives aimed at preventing obesity (Wang Y. et al., Reference Wang2013; Wang M. et al., Reference Wang2014). There is some preliminary evidence on the effectiveness of peer influence, peer support and peer education in promoting health-related behaviours for young people (Lau et al., Reference Lau, Quadrel and Hartman1990; Borsari & Carey, Reference Borsari and Carey2001; Salvy et al., Reference Salvy2012; Tolli, Reference Tolli2012; Jenkinson et al., Reference Jenkinson, Naughton and Benson2014; Whipp et al., Reference Whipp2015; Aceves-Martins et al., Reference Aceves-Martins2017). Internet- and innovation-based initiatives, as well as programmes that appeal to adolescents, may also enhance the effectiveness of preventative interventions by improving health-related behaviour change (Whittemore et al., Reference Whittemore, Jeon and Grey2013; Chen & Wilkosz, Reference Chen and Wilkosz2014; Aceves-Martins et al., Reference Aceves-Martins2017).
New models of intervention for promoting health and healthy lifestyles among children and adolescents have been recently tested in Tuscany. These models use behavioural and social mechanisms to enhance traditional interventions, which are often delivered in educational environments. The ‘beFood’ project was an action research project within a mandatory work-related learning pathway for high school students, called ‘Alternanza Scuola-Lavoro’ (ASL). The ASL projects provide students with professional opportunities and train them for a specific job according to their preferences and attitudes.
The main aim of the beFood project was to involve a group of forty-nine 16- and 17-year-old students in peer-to-peer action research. Their ‘job’ assignment was to inform their peers about healthy lifestyles by conducting a large-scale participatory survey within the ASL programme.
In the first phase, the 49 students took part in a training and educational week outside of their schools. A peer-to-peer and digital-based method was adopted to build a dialogue with adolescents regarding their habits and preferences related to nutrition, physical activity and sports. In addition, they examined a range of influences on unhealthy behaviours (e.g., food marketing, techniques for framing default choices, present and habit loop biases) and analysed communication preferences (e.g., preferred sources of information), environmental aspects, self-esteem and self-perception.
The education phase was based on a collaborative approach focused on a pathway that put the students at the heart of the learning process and thus helped them to better retain and internalize the contents (Knowles, Reference Knowles1989). Experts and researchers actively involved students in practical activities aimed at ‘learning by doing’, nudging them to make healthier choices in terms of nutrition, sports and physical activity. The high school students were engaged in research topics, such as helping the researchers validate the questionnaire and test the web app used for administering the survey. The web-based survey was developed as a ‘test’ of each teenagers’ lifestyle, which ended by providing a cartoon profile with suggestions for improving their habits by activating mechanisms of informational feedback, warnings and past choices (Eysenbach & Wyatt, Reference Eysenbach and Wyatt2002; Sunstein, Reference Sunstein2014; Samson, Reference Samson2015). The teenagers were divided into ten groups (one for each Tuscan province) to improve peer group pressure and team-working skills and to stimulate competitive and collaborative mechanisms among them. During this first week, researchers consistently explained the importance of the students’ role in the beFood research project to leverage mechanisms such as identification, increasing salience and building on social utility (Cialdini et al., Reference Cialdini, Martin and Goldstein2015; Samson, Reference Samson2015). The students were made aware that their work was fundamental to spreading the new knowledge they learned and that the dissemination of the ‘healthy message’ could improving their peers’ lifestyle. They understood the importance of producing robust research results in order to have a concrete effect on lifestyles and inform policy-makers. A survey showed that almost 80% of the students completely agreed that the project provided them with knowledge and competency in adopting a healthy lifestyle. More than 73% completely agreed they had acquired a greater awareness of the ‘value of the research’ in public policy-making. The 49 students were informed that the last phase of the project included their presentation of the completed research and of the project's results directly to Tuscan policy-makers. These two aspects of responsibility and accountability towards official representatives were fundamental in empowering the students for the second phase of the project (Nuti et al., Reference Nuti2017).
In the second phase, the students were engaged in peer-to-peer interactions aimed at amplifying the magnitude of the impact of the intervention throughout the region. By applying what they had learned in the previous training week and with the support of their tutors, each of the ten groups was assigned the responsibility of informing a minimum sample of peers within their respective province of residence about healthy lifestyles. They chose how to accomplish the task using the beFood web app, which counted the numbers exposed to beFood messages and enabled easy participation by their peers in the beFood survey. Over 4 months, 5029 people completed the survey using the beFood web app, of which 4749 were 16- and 17-year-olds. These data were used to analyse teenagers’ habits and preferences. The preliminary results were included into a report (Nuti et al., Reference Nuti2017). In the final phase of the project, the same 49 students presented the results to policy-makers, high school principals and teachers, researchers and experts.
Almost 70% of the 49 students gave a positive or very positive evaluation of the task they had been given, and 80% of them assessed the responsibility linked to this task as positive or very positive. Almost 59% of the students felt that they were a key part of the initiative. Two out of five reported that the influence their work had on their peers’ lifestyle-related behaviours may have been significant. Half of the students reported having paid greater attention to nutrition and 30% to physical activity and sports. One out of four students had also given advice for a better lifestyle regarding nutrition on their own initiative, and 22% did so with regard to physical activity and sports. Almost 44% offered advice to peers who were friends, and more than 30% offered advice to their adult relatives.
Fifty-four percent of the participants stated that they had improved their nutrition-related behaviours after having participated in beFood, and 48% had improved their regularity in performing physical activities.
A short survey was sent to the respondents contacted by the students using the beFood web app. This second questionnaire has been answered by 147 teenagers. More than half of them (51.5%) reported their intention to change their food-related behaviours, and 20.5% intending to change their physical activity habits after reading the beFood feedback. Four out of ten respondents indicated an improvement in their lifestyle behaviours. Sixty percent of those who had expressed intentions of changing their lifestyle reported having done so.
The Diabetic Patients’ Self-Management case
For diabetes, self-management is vital. In 2014, the Funding Program of the Italian Center for Disease Control, a department of the Italian Health Ministry, allocated a grant to three Italian Regional Health Systems: the autonomous province of Bolzano and the regions of Tuscany and Basilicata. They were willing to systematically implement an education programme for diabetes under the coordination of the Laboratorio Management e Sanità. The main aim of the Diabetic Patients’ Self-Management (DPSM) programme was to promote healthy behaviours (diet and physical activity) through self-management in order to achieve an improvement in the health of diabetic patients.
The DPSM created by the Stanford Patient Education Research Center (Lorig et al., Reference Lorig2016a, Reference Lorig2016b) was adopted for educating patients. The programme aims to promote competencies in the three tasks involved in self-managing the disease (therapeutic management, which includes lifestyle; management of emotions; and management of the social role). The seminars are structured in six workshops each having a duration of 2.5 hours and delivered interactively, including goal-setting and reinforcement practices, to enhance individuals’ self-efficacy (Bandura, Reference Bandura1997; Samson, Reference Samson2015). This design has been tested in a Spanish version, but implementation takes context into account (Lorig et al., Reference Lorig2009). For the Italian version, the contents have been adapted by including reference to the Mediterranean diet pattern in order to foster participants’ identification with the programme and to give consideration to specific cultural habits. The workshops are conducted in small groups (about 14–16 patients per group) either by health professional leaders or by trained lay leaders.
DPSM programme received strong support from each of the three Italian regions involved on the basis of its value in engaging and empowering patients themselves and their communities. In each region, laypeople, enrolled either from the community or from diabetes patient associations, were trained to be ‘expert patients’ and to lead a diabetes education programme. They were in charge of organizing and leading the six meetings and giving support to participants in need, either individually or assisted by a health professional.
A total of 76 seminars were held throughout the three regions, facilitated by 108 leaders and involving 909 diabetics and 72 caregivers. The seminars covered self-management, diet, physical activity, managing diabetes symptoms, self-efficacy and depression. Participants were on average 67 year of age and had, on average, 9.6 years of education. More than the half were men (54%).
After 6 months of seminars, when a problem occurred, participants felt more confident in managing their disease at home most of the time: the self-efficacy score changed from 6.4 to 8.0 (p < 0.0001). As a consequence, participants modified their diets (e.g., they reduced consumption of red meat and increased that of fish), spent more time walking and improved their adherence to prescribed drugs. In addition, participants showed a reduction in their number of visits to their doctors (hospital specialist or family doctor; p < 0.0001), as well as the use of hospitals and emergency departments (not statistically significant).
After 6 months of seminars, improvements in participants’ health status were noted (reductions in the HbA1c indicator and body mass index (p < 0.0001) and depression scores (p < 0.01)). The expert patients who were peer instructors reported higher scores on self-sacrifice motivation, intrinsic motivation and sense-making. Participants gave positive feedback in terms of both the involvement of the lay leaders and their effective support during the programme.
At the end of the pilot project, each Regional Health System sought to include the education programme as part of their diabetes patient care pathways. Systemic strategies have been adopted (e.g., the Tuscany programme called IDEA – ‘Incontri di educazione all'autogestione’ (‘Self-management education workshops for chronic patients’)) to promote community engagement in the education programme and to achieve patient and family activation and empowerment.
The Adapted Physical Activity case
Population ageing means more people have chronic diseases and comorbidities (He et al., Reference He, Goodkind and Kowal2016). About a third of people living in Tuscany are physically inactive (Istituto Superiore di Sanità, 2016), with pernicious effects for those suffering from chronic diseases due to social exclusion, loss of autonomy and poor quality of life (Greaves and Farbus, Reference Greaves and Farbus2006; James et al., Reference James2011; He et al., Reference He, Goodkind and Kowal2016). The aim of promoting healthy lifestyles for people who are ageing is to increase physical activity levels by providing interventions that also tackle social exclusion and its consequences (Benvenuti, Reference Benvenuti2009; Speroni et al., Reference Speroni2011; Lim et al., Reference Lim2012; Vainieri et al., Reference Vainieri2016).
In 2005, Adapted Physical Activity (APA; in Italian, AFA) has been tested in Tuscany with the aim of giving elderly people a way to become and stay active in a safe context. The experience was a success and, over time, it has become a diffused and effective intervention throughout the region (Stuart et al., Reference Stuart2009; Ministero della Sanità, Reference della Sanità Italiano2011; Songthai et al., Reference Songthai2014; Rachlis et al., Reference Rachlis2016).
The APA programme is a community-based, progressive, supervised group exercise programme adapted to chronic alterations of functional status for the prevention and mitigation of disability (Stuart et al., Reference Stuart2009; Benvenuti, Reference Benvenuti2014). This programme is based on the Chronic Care Model (Wagner, Reference Wagner1998), allowing people to stay together and to take care of their own physical and mental health by building effective networks of social support (Consiglio Regionale Toscana, 2008; Giunta Regione Toscana, 2009; Early Action Task Force, 2014).
APA is offered as a social rather than clinical activity and facilitates adults taking part in regular exercise through a social learning model (Sofi et al., Reference Sofi2011). Conventional preventative interventions (e.g., physiotherapy sessions) are limited in duration and treat participants as passive recipients. These characteristics lead to low adherence in patients continuing to exercise at home (Sofi et al., Reference Sofi2011; Litt et al., Reference Litt, Kleppinger and Judge2002). Instead, the APA programme is based on regular attendance by participants who are responsible for performing the exercises at home. During the weekly lessons, trainers provide participants with experiential knowledge on how to exercise, thus working to create a habit that becomes easy to sustain. Adherence is stimulated by social support developed through building and maintaining local social networks (Middleton et al., Reference Middleton, Anton and Perri2013). Being part of a social group context means participants can support each other in following instructions, in attending the sessions regularly and in repeating exercises at home (Sofi et al., Reference Sofi2011; Litt et al., Reference Litt, Kleppinger and Judge2002).
At the 6-month follow-up, a controlled study of the APA programme found that “the intervention group improved whereas controls declined in gait velocity, balance, Short Physical Performance Battery, and Stroke Impact Scale social participation domains” (Stuart et al., Reference Stuart2009). The depression score of participants improved by an average score of 4.4 (p < 0.003), while people in the control group did not move from their baseline scores. Adherence and distance are highlighted as essential factors in achieving positive outcomes at the end of the programme (Sofi et al., Reference Sofi2011; Hicks et al., Reference Hicks2012). Indeed, ensuring that the assimilated habits are maintained over time and that local contexts are organized to guarantee access to the programme are fundamental to achieving beneficial and sustained outcomes.
After a successful pilot conducted in the LHA of Empoli, the programme was extended to the whole region, thus becoming a systemic action. To ensure easy access throughout Tuscany, APA providers can be either for-profit or non-profit, and the activities can take place wherever is accessible and suitable (e.g., gyms, churches, buildings of political parties and local associations, municipalities). Groups of volunteers guarantee access by providing transportation where necessary. Every May, an ‘APA day’ is organized at the regional level with the aim of promoting participation in the programme through social and recreational activities (e.g., ‘the healthy walk’ or listening to previous participants’ personal experiences). The activities are open to all.
After 10 years, the APA programme has become an established intervention with mass participation of 30,000 people throughout Tuscany (Vainieri et al., Reference Vainieri2016). This high rate of uptake is the result of various social influences (peer-to-peer word of mouth, me-too processes, social reputation), the availability of the programme locally in familiar settings (e.g., gyms, theatres, churches) and the assistance provided to those in need of transportation. Those who take part in APA courses become members of active local social groups, which remedies loneliness and improves health (Stuart et al., Reference Stuart2009; Hicks et al., Reference Hicks2012), improving their happiness, empowerment and self-confidence, while providing a means to make use of underemployed spaces (i.e., in otherwise empty gyms in the morning).
Results
Table 1 shows the results of the three case studies compared on the basis of the education, activation, engagement and empowerment principles. In this section, the authors describe common and divergent elements pertaining to the three cases.
Table 1. Comparative scheme of the implemented framework in the three case studies.

Education always took place in small groups in which individuals practiced the new habits (‘by doing’) through a participatory and engaging approach facilitated by peer interactions and laypeople. Education and communication strategies were aimed at supporting learning processes by increasing the salience of healthy messages and motivating participants towards their internalization. The educators/trainers created conditions for participants to be involved in first-hand experiences so that the subsequent behavioural change would be more effective than that of the traditional curricula (Knowles, Reference Knowles1989; Prochaska et al., Reference Prochaska, DiClemente and Norcross1992; Dudley et al., Reference Dudley, Cotton and Peralta2015; Samson Reference Samson2015). Each educational intervention was developed based on participants’ knowledge, experience and level of ability, thereby improving their self-confidence and sense of responsibility for their own health and quality of life. The new skills and knowledge were translated into a positive change of behaviour, which became a positive example for their networks of friends and relatives. In the beFood and DPSM experiences, laypeople were explicitly trained to become trainers of and messengers for their peers. In the APA case, only experts conducted the lessons. However, in all three cases, participants became advocates, messengers and testimonials of their healthy choices, especially in the beFood and APA cases, where the effect is amplified in terms of lifestyle-related behaviours. Each intervention activates three levels of social ‘nudges’ to encourage movement to healthier choices (Van Der Linden, Reference Van Der Linden2018). Experts and laypeople ‘nudge’ participants; participants ‘nudge’ their peers and networks of friends and family; and changes in practice to the choice architecture nudge those who have not been involved.
The three interventions differ on the applicability of the four principles of education, activation, engagement and empowerment. The APA programme was first thought of simply as a clinical intervention with a small activity component for participants. However, the elements characterizing its activities transformed it into an innovative preventative intervention that increasingly enables participants to develop autonomy and responsibility in taking care of themselves and involving others. Participants are not involved in designing and delivering the APA intervention at an early stage, but they can participate in witnessing the programme in their networks. For beFood, the initial training week of the 49 students has been structured with overlapping education and engagement activities, involving simultaneous knowledge transfer and collaboration between researchers and teenagers in designing and conducting the intervention. DPSM works on education, activation and empowerment throughout the workshops, but engagement depends on the future availability of some participants to become lay or peer instructors.
Discussion and conclusions
The three experiences described in this paper show how health promotion interventions can be redesigned to exploit behavioural and social mechanisms in order to create the right conditions to make individuals, patients and communities able to improve their health and well-being and increase both individual and social value. In particular, the education–activation–engagement–empowerment framework has been tested as a way of implementing and analysing behaviourally and socioculturally informed interventions (see Figure 1).
The development of each intervention was not based on a mechanical application of the four principles of the framework. On the contrary, each includes specific features that meet the needs and preferences of the targeted population according to their sociocultural context, intervention goals and lessons learned from previous experiences. Two of the three cases, namely the DPSM and APA programmes, have detailed structures, have been repeatedly tested and are replicated at low cost. APA has shown its flexibility in different non-clinical settings and has succeeded in reaching large numbers of people in a short period of time, improving their health and quality of life. In contrast, beFood is a first explorative experience in drawing on digital technologies and collaborative processes to conduct a health promotion intervention, and so has yet to be replicated.
All three interventions have addressed the issues of magnitude of impact, adherence and social and cultural variables in behaviourally informed interventions. The attention paid to these aspects differentiates these programmes from conventional actions like as National Diabetes Preventive Programme. This national programme implemented in England is an example of a traditional preventative intervention that, even if it were cost effective, would prevent few of those who enrol in it from developing diabetes because of its limited impact on substantive and enduring behavioural change (De Poli et al., Reference De Poli2018).
Alternatively, experiential learning, social support and community engagement, the possibility of participants getting ‘officially’ engaged within the system's activities and empowerment can be key principles for enlarging the magnitude of impact of health promotion interventions. The implemented participatory group-based learning methods and the peer processes allowed each intervention to have a greater impact in terms of the number of people they ‘touched’, thanks to the active role of participants. Engaged and empowered participants have directly or indirectly reached a number of other people in their networks, becoming effective collaborators with the system by spreading the knowledge and skills they acquired during the education and activation phases. The APA participants’ engagement with institutional activities is mostly informal and based on their voluntary initiative, but it has been very effective in building supportive networks that ensure long-term adherence following the termination of the intervention. Participants in DPSM activities can choose to be engaged in delivering the programme to future classes of diabetic patients, and their participation as lay leaders increases participants’ satisfaction with the programme. Finally, students who participated in beFood gained early access to practical knowledge and were considered as protagonists of the project from the beginning, collaborating with researchers in the design and delivery of the intervention. Identification and peer comparison stimulated them to spread the beFood message to peers and relatives.
Adherence is also fundamental to maintaining behavioural changes over time (Middleton et al., Reference Middleton, Anton and Perri2013). The processes of education, activation, engagement and empowerment of individuals, implemented by the health services providers, laypeople and peers, coupled with the implied behavioural and social mechanisms, are essential for enabling and facilitating participants to continue after the intervention ends by enhancing adherence in their daily lives at both the individual and social levels. Social support and normative feedback dynamics were used to enhance people's long-term adherence to the newly established routines. The possibility of sharing everyday challenges with other participants leads to the creation of supportive social networks that can work, after the intervention ends, as ‘extended care’ structures (Middleton et al., Reference Middleton, Anton and Perri2013).
Each intervention has been developed specifically for the targeted population by taking into account the social and cultural dimensions influencing their behaviour. As Van Der Linden (Reference Van Der Linden2018) showed, this adds to the effectiveness of BE approaches directed at individuals by exploiting the power of social nudges. Indeed, redefining identity through social norms is a powerful mechanism that is easy to implement for changing behaviour (Cialdini et al., Reference Cialdini, Martin and Goldstein2015). In this way, individuals develop a new health literacy to guide their actions in making their daily environments healthier.
The implementation of interventions similar to those described above implies a redefinition of health care professionals’ role from providers to solution-finders, context-makers or directors and supporters of people. Taking into consideration the patients’ perspectives is not sufficient: the patients themselves should be actively involved and engaged at both the individual and community levels by working on the behavioural and social mechanisms that affect their motivation to change. This approach is based not on the traditional assumption of agency for the citizen, but on the acknowledgement of the active roles of different stakeholders in the entire process of health value creation. The concept of the patient–doctor relationship needs to be revised for preventative interventions by working on the behavioural and cultural dimensions and by changing the paternalistic educational approach to learning processes in order to give greater autonomy to people. This means health care professionals need to build the right conditions (i.e., choice architectures, social contexts, etc.) to engage and empower people by increasing or improving their knowledge and skills, building on their capabilities and nudging and supporting them in maintaining, advocating for and spreading new, healthier habits and knowledge. To this end, professionals need to recognize the potential roles of individuals, their networks and the benefits people can produce at the individual and collective levels. They also need to learn how to highlight the available individual and social resources for creating value in the specific action context in order to adapt and reshape the intervention design and implementation in terms of learning, enabling processes and contents. Health care services can create enabling contexts for designing interventions focused on useful behavioural and social dynamics in order to build, improve and support the knowledge, skills and motivation of people, thus allowing them to become the main actors in generating value at the individual and collective levels. The professionals’ role changes from determining what might be valuable for passive recipients to coordinating and promoting individuals’ participation, supporting behavioural changes and facilitating advocacy and reciprocity effects (Knowles, Reference Knowles1989; Middleton et al., Reference Middleton, Anton and Perri2013; Cialdini et al., Reference Cialdini, Martin and Goldstein2015).
This proposal differs from the ‘nudge’ interventions that assume that the ‘nudgers’ know what are the best choices to propose. However, this vision can easily lead policy-makers to adopt a paternalistic approach (Matjiasko et al., Reference Matjasko2016). In contrast, the three interventions described above have been built on a person-centred and person-driven model (Leggett, Reference Leggett2014; Oliver, Reference Oliver2015) based on collaborative processes and specific attention being paid to the cultural and social contexts (Middleton et al., Reference Middleton, Anton and Perri2013; Laverack, Reference Laverack2017).
Acknowledgements
The Region of Tuscany financed both the beFood and the APA projects. The Italian Minister of Health financed the DPSM project (CCM program).
Author contributions
All of the authors were involved in designing the overall contents of this paper, wrote the manuscript and were involved in interpreting the findings. In particular, all of the authors were responsible for writing the manuscript, with the following contributions on: introduction and discussion (SN, FP, AMM, SDR); theoretical background (FP); beFood case (SDR); DPSM case (AMM); AFA case (FP). All of the authors approved the final manuscript.




