Book contents
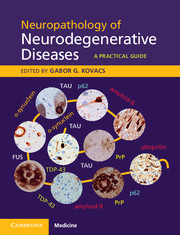
- Neuropathology of Neurodegenerative Diseases
- Neuropathology of Neurodegenerative Diseases
- Copyright page
- Contents
- Contributors
- 1 Introduction
- 2 Clinical aspects of dementia
- 3 Clinical aspects of movement disorders
- 4 Ethical, health and safety considerations
- 5 Practical approach to diagnosis
- 6 Molecular methods
- 7 Alzheimer’s disease
- 8 Tauopathies
- 9 Synucleinopathies
- 10 Human prion diseases
- 11 Neurodegenerative diseases linked to trinucleotide repeats
- 12 Amyotrophic lateral sclerosis and frontotemporal lobar degeneration
- 13 Other neurodegenerative conditions I
- 14 Other neurodegenerative conditions II
- 15 Other neurogenerative conditions III
- 16 Other neurogenerative conditions IV
- 17 Concomitant pathologies I
- 18 Concomitant pathologies II
- Appendix A Molecular classification of frontotemporal lobar degeneration (FTLD) with genetic correlations
- Appendix B Scheme for evaluation of frontotemporal lobar degeneration (FTLD)
- Index
12 - Amyotrophic lateral sclerosis and frontotemporal lobar degeneration
Published online by Cambridge University Press: 05 December 2014
- Neuropathology of Neurodegenerative Diseases
- Neuropathology of Neurodegenerative Diseases
- Copyright page
- Contents
- Contributors
- 1 Introduction
- 2 Clinical aspects of dementia
- 3 Clinical aspects of movement disorders
- 4 Ethical, health and safety considerations
- 5 Practical approach to diagnosis
- 6 Molecular methods
- 7 Alzheimer’s disease
- 8 Tauopathies
- 9 Synucleinopathies
- 10 Human prion diseases
- 11 Neurodegenerative diseases linked to trinucleotide repeats
- 12 Amyotrophic lateral sclerosis and frontotemporal lobar degeneration
- 13 Other neurodegenerative conditions I
- 14 Other neurodegenerative conditions II
- 15 Other neurogenerative conditions III
- 16 Other neurogenerative conditions IV
- 17 Concomitant pathologies I
- 18 Concomitant pathologies II
- Appendix A Molecular classification of frontotemporal lobar degeneration (FTLD) with genetic correlations
- Appendix B Scheme for evaluation of frontotemporal lobar degeneration (FTLD)
- Index
- Type
- Chapter
- Information
- Neuropathology of Neurodegenerative DiseasesA Practical Guide, pp. 209 - 248Publisher: Cambridge University PressPrint publication year: 2014
- 4
- Cited by