Book contents
- Alzheimer’s Disease Drug Development
- Alzheimer’s Disease Drug Development
- Copyright page
- Dedication
- Contents
- Contributors
- Foreword
- Acknowledgments
- Section 1 Advancing Alzheimer’s Disease Therapies in a Collaborative Science Ecosystem
- Section 2 Non-clinical Assessment of Alzheimer’s Disease Candidate Drugs
- Section 3 Alzheimer’s Disease Clinical Trials
- Section 4 Imaging and Biomarker Development in Alzheimer’s Disease Drug Discovery
- Section 5 Academic Drug-Development Programs
- Section 6 Public–Private Partnerships in Alzheimer’s Disease Drug Development
- Section 7 Funding and Financing Alzheimer’s Disease Drug Development
- Index
- References
Section 4 - Imaging and Biomarker Development in Alzheimer’s Disease Drug Discovery
Published online by Cambridge University Press: 03 March 2022
- Alzheimer’s Disease Drug Development
- Alzheimer’s Disease Drug Development
- Copyright page
- Dedication
- Contents
- Contributors
- Foreword
- Acknowledgments
- Section 1 Advancing Alzheimer’s Disease Therapies in a Collaborative Science Ecosystem
- Section 2 Non-clinical Assessment of Alzheimer’s Disease Candidate Drugs
- Section 3 Alzheimer’s Disease Clinical Trials
- Section 4 Imaging and Biomarker Development in Alzheimer’s Disease Drug Discovery
- Section 5 Academic Drug-Development Programs
- Section 6 Public–Private Partnerships in Alzheimer’s Disease Drug Development
- Section 7 Funding and Financing Alzheimer’s Disease Drug Development
- Index
- References
Summary
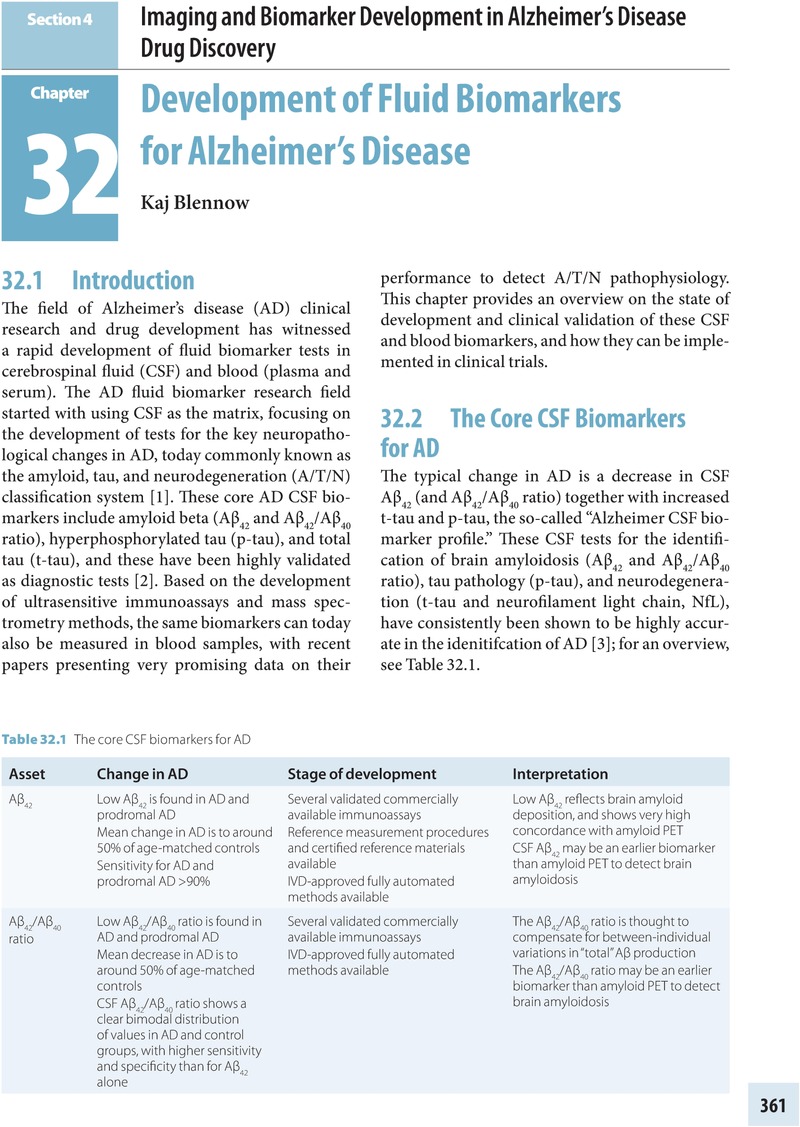
- Type
- Chapter
- Information
- Alzheimer's Disease Drug DevelopmentResearch and Development Ecosystem, pp. 361 - 428Publisher: Cambridge University PressPrint publication year: 2022

