Introduction
Appendicitis is the most common non-traumatic surgical emergency in children.Reference Reynolds and Jaffe 1 , Reference Scholer, Pituch and Orr 2 Despite the high incidence of appendicitis, the diagnosis remains challenging, as patients often lack the classic historical and physical examination findings.Reference Becker, Kharbana and Bachur 3 This has led to substantial reliance on diagnostic imaging,Reference Pines 4 including ultrasound (US), computed tomography (CT), and staged protocols.Reference Krishnamoorthi, Ramarajan and Wang 5 , Reference Ramarajan, Krishnamoorthi and Barth 6 Due to increased availability of US and increased awareness of potential adverse outcomes associated with ionizing radiation, particularly in young children,Reference Brenner, Elliston and Hall 7 many health care providers choose ultrasonography as their first line imaging modality to diagnose appendicitis in the pediatric population.Reference Thompson, Schuh and Gravel 8
The diagnostic accuracy of ultrasonography is subject to visualization of the structures to be assessed, which in the case of appendicitis is often limited.Reference Ross, Liu and Netherton 9 In an attempt to optimize visualization of pelvic and intra-abdominal structures, some institutions require bladder filling prior to pelvic US examination for suspected appendicitis. This can be uncomfortable for patients and leads to delays in test acquisition and subsequent diagnosis.Reference Poonai, Gregory and Thompson 10 While there is some evidence that delays in diagnosis and treatment make little difference to clinically important outcomes,Reference Poonai, Gregory and Thompson 10 - Reference Taylor, Emil and Nguyen 13 other studies suggest treatment delays may lead to increased rates of perforation.Reference Papandria, Goldstein and Rhee 14
Our objective was to determine the value of bladder filling prior to pelvic US in children with suspected appendicitis. Specifically we examined the impact of a full versus sub-optimally filled bladder on the proportions of diagnostic pelvic US studies in males and females as well as proportions of fully visualized ovaries.
Methods
Study design
We performed a retrospective health record review, combining data that were available from a study previously reported by our teamReference Ross, Liu and Netherton 9 with US images to calculate bladder size. This study was approved by the Conjoint Health Research Ethics Board of the University of Calgary.
Study setting and population
This study was conducted in the departments of Pediatric Diagnostic Imaging and Pediatric Emergency Medicine at the Alberta Children’s Hospital (ACH). ACH is the pediatric tertiary care facility serving southern Alberta, western Saskatchewan and eastern British Columbia, with an annual emergency department (ED) census of approximately 72,000 visits and a catchment area of 1.8 million.
Diagnostic imaging studies were reviewed for children aged 2-17 years who received an US for suspected appendicitis during the predefined inclusive time period of January 1, 2007, through December 31, 2008. Eligible subjects were identified using electronic patient tracking databases hosted by the department of radiology. Databases were searched for records of children receiving an US with the “US Appendix” protocol code. US studies were performed by trained US technicians and reported by staff radiologists. At our pediatric center, US imaging of the pelvis is limited to the transabdominal approach. Therefore, no transvaginal USs were evaluated.
Study protocol
Baseline demographic and clinical data were available from our previously published health record review,Reference Ross, Liu and Netherton 9 in which we collected demographic data, ED visit details, results of laboratory investigations, surgical considerations, frequency of return visits to the ED, and imaging reports. These data were used in a previous studyReference Ross, Liu and Netherton 9 to examine the outcomes of children with suspected appendicitis after US examination failed to identify the appendix. In particular, we studied children’s outcomes, including their disposition, the proportion returning for care, the proportion undergoing surgical intervention, and the number of “missed” appendicitis cases, as well as the test characteristics of secondary signs of inflammation in this population. For the purpose of this study the existing database was expanded by reviewing all available US images and diagnostic imaging reports. One of our authors (S.S.) received standardized training in research ethics, methodologies, and data entry, and collected additional data for all US images available on PACS (Picture Archiving and Communications System), including bladder shape, bladder dimensions, appendix visualization, ovarian visualization, and alternative diagnoses using a standardized data collection form. Radiology reports were reviewed to assess for ovarian visualization. Predictor and outcome variables were operationalized as much as possible to reduce the potential for bias.
Definitions
An “incompletely visualized appendix” was defined as any US study that failed to visualize the entire appendix. A “normal” US fully visualized a normal appendix in males or a normal appendix and ovaries in females and found no alternate diagnosis. An “alternative diagnosis” was defined as a finding on US that was considered the primary diagnosis on the ED record other than appendicitis. A “diagnostic US” included: a normal US, was diagnostic of appendicitis, or made an alternative diagnosis. All scans that did not meet diagnostic US criteria were classified as non-diagnostic. We considered patients to have a full bladder if the percent of expected bladder capacity (PEBC) was greater than or equal to 75%. Those with PEBC less than 75% were considered to have sub-optimally filled bladders. We considered a radiology report that included a term such as “ovaries are fully visualized” as positive for ovarian visualization. We did not directly collect data on full adnexal visualization but collected data from positive adnexal findings under “alternative diagnosis.”
Estimating bladder size, age-based normal and bladder fullness
In order to estimate bladder size on US we collected data on anterior-posterior diameter (APd) and the width (W) of the bladder from the transverse view. The bladder cranio-caudal diameter (CCd) was determined from the sagittal view. Accurate estimation of bladder volume must take into consideration the bladder shape.Reference Bih, Ho and Tsai 15 , Reference Kuzmić, Brkljacić and Ivanković 16 As outlined in detail by Kuzmic et al.Reference Kuzmić, Brkljacić and Ivanković 16 we classified bladder shape as round, ellipsoid, cuboid, triangular, or undefined. Estimated bladder volume (EBV) was then calculated with the following equation:
where k varied with bladder shape. Specifically, the k values used were 0.561 for round, 0.923 for cuboid, 0.802 for ellipsoid, 0.623 for triangular, and 0.749 for undefined, as recommended by Kuzmic et al.Reference Kuzmić, Brkljacić and Ivanković 16
Estimated bladder capacity (EBC) was defined using the following validated age-based equation as originally presented by Kaefer et al.:Reference Kaeffer, Zurakowski and Bauer 17
EBC (in mL) = 133.08 × Age0.4
We then calculated the percent of expected bladder capacity (PEBC) expressed as a percentage by dividing the EBV by the EBC as follows:
All PEBC greater than 100% are reported as 100%.
Calculating the effect of bladder fullness on the rate of diagnostic US
The primary outcome variable was the proportion of diagnostic USs. We hypothesized that the group with sub-optimally filled bladders would be non-inferior to the group with full bladders. We defined a priori subgroup analyses based on sex for the primary outcome variable in groups with both full and sub-optimally filled bladders. The secondary outcome variable was the proportion of complete ovarian visualization in females.
We compared proportions of diagnostic USs in patients with filled versus sub-optimally filled bladders using statistical analysis often used in non-inferiority trials. Given the retrospective nature of our study we, by definition, did not perform a formal non-inferiority trial. Rather, we utilized a statistical technique commonly employed in non-inferiority trials to examine for a clinically significant difference or lack thereof in our primary outcome measure. Specifically, we calculated the difference in mean proportions of diagnostic USs in those with full and sub-optimally filled bladders. We considered a 10% difference in mean proportions of diagnostic USs to be clinically significant and set this as our delta value.Reference Wiens 18 In other words, we considered the performance of US with sub-optimally filled bladders to be non-inferior to US with full bladders if the mean proportion of diagnostic USs was no lower than 10% compared to the mean proportions in those with full bladders. The same strategy was used in our sub-group analysis by sex as well as to assess ovarian visualization.
Results
Of 978 records reviewed in our original study,Reference Ross, Liu and Netherton 9 we were able to obtain sufficient images to calculate bladder size in 678 patients. In 55 cases, the US images were insufficient in areas scanned to estimate bladder size. In 245 cases, we were unable to obtain any images from the diagnostic imaging database. Patient identification numbers from our original study often had written US reports available but no cached images in our diagnostic imaging database. We were therefore unable to calculate bladder size and include these studies in our final analysis. However, no statistical demographic differences were found between those included and not included in the study (Appendix 1). A flow diagram of reviewed charts appears in Figure 1.
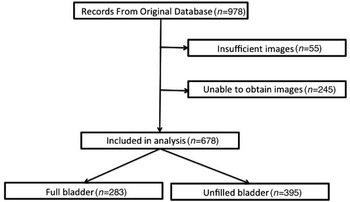
Figure 1 Patients included in final analysis
Demographic parameters and US classifications are presented in Table 1. The proportion of diagnostic US studies did not vary significantly between groups with a full or sub-optimally filled bladder (47% [132/283] vs. 52% [205/395] respectively, p=0.17). This observation held true in both male and female cohorts (p=0.24 and p=0.58 respectively). Rates of ovarian visualization were higher in females with a full bladder compared to those with a sub-optimally filled bladder (96% [196/205] vs. 81% [180/223] respectively, p<0.01). There was a greater proportion of males with sub-optimally filled bladders as compared to females (69% [172/250] vs. 52% [223/428] respectively, p<0.01). Further sub-classifications of diagnostic USs are reported in Table 2.
Table 1 Proportions of diagnostic ultrasound results and odds ratios
Odds ratios report the odds of having a non-visualized scan with an unfilled bladder.
CTAS: Canadian Triage Assessment Score
95% CI: 95% confidence interval
SD: standard deviation
* Z-tests were used to calculate p values
Table 2 Specific diagnostic ultrasound results
Results of the primary outcome are displayed graphically in Figure 2. The group with sub-optimally filled bladders was non-inferior to the group with full bladders. This finding was true in both our male and female subgroups. The group with unfilled bladders had significantly lower rates of ovarian visualization than those with full bladders. However, it is plausible that the true treatment difference is less than our clinically relevant delta value of 10%.Reference Piaggio, Elbourne and Altman 19
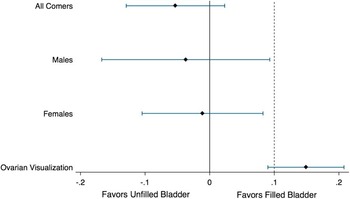
Figure 2 Non-inferiority Analysis Delta of 10% represented with dashed line
Discussion
In this study, we examined the relationship between bladder volume and a diagnostic US examination in children with suspected appendicitis. Our data demonstrate that the proportion of diagnostic US studies does not vary significantly with a full or sub-optimally filled bladder and this observation held true across sex.
These results suggest that omitting routine bladder filling from diagnostic protocols for suspected appendicitis may not change diagnostic accuracy. Omitting routine bladder filling could improve emergency department flow, prevent patients from enduring a painful full bladder, and decrease the need for invasive procedures at institutions that fill bladders using catheterization. While the American Institute of Ultrasound in Medicine still recommends bladder filling for pelvic ultrasonography in their 2010 guidelines, 20 other experts in the field have cogently argued that this practice may be unnecessary with modern US technology,Reference Benacerraf 21 albeit in an older population. Consideration should be made for discontinuing the practice of routine bladder filling in pediatric patients with suspected appendicitis.
In contrast to the appendix, we found that full ovarian visualization was significantly higher in those with full bladders as compared to those with unfilled bladders. This is likely due to the acoustic window created by a fluid filled structure. Therefore, it is reasonable to consider bladder filling in female patients presenting with abdominal and/or pelvic pain in whom appendicitis and ovarian pathology are in the differential diagnosis (i.e., post-pubertal females). Further study is required to delineate the value of ovarian visualization in guiding management. Our data demonstrate that if ovarian pathology is not suspected, bladder filling may not be routinely required prior to US examination. In collaboration with radiology departments, emergency physicians should consider implementing protocols that do not require bladder filling in male patients and female patients with no clinical concern for ovarian pathology. This may speed throughput and improve patient satisfaction. However, these process measures and patient-reported outcome measures, such as time to US and patient comfort, were not available in this study.
The higher proportion of males with unfilled bladders was an unexpected finding. It may be that the bladder filling protocol was less strictly adhered to in the male population due to absence of clinical concern for pathology in pelvic organs.
Limitations
Our study faces limitations due to incomplete and missing images. This is unlikely to significantly bias our results, given similarities between groups with and without available complete images, as described in Appendix 1.
Our definition of a full bladder being greater than 75% of the PEBC is arbitrary. However, this value was felt to be clinically appropriate and a change in the cutoff would be unlikely to change our results. Likewise our delta value of 10% for non-inferiority is arbitrary but is clinically reasonable.
Our statistical analysis was performed on retrospective data available from a previous trial. As such this study is not a non-inferiority trial but rather a retrospective analysis using non-inferiority statistical techniques to analyze available data.
Other limitations include our inability to fully characterize and adjust for other patient factors that may have limited diagnostic accuracy, such as patient cooperation, position of the appendix, such as retrocecal, and body habitus, as these data were not available. Classification of bladder shapes and bladder measurements was performed by a single author, and so we were unable to calculate an interclass correlation coefficient, and significant error may have occurred.
Conclusion
The presence of a full bladder prior to US for suspected appendicitis was not associated with higher proportions of diagnostic USs for pediatric appendicitis in our population. However, the proportion of USs with fully visualized ovaries was significantly higher when the bladder was full. Administrators and clinical decision makers should consider omitting routine bladder filling from current pediatric appendicitis protocols in males and in pre-pubertal females where ovarian pathology is not suspected. Selective bladder filling prior to US should be performed in females when ovarian pathology is suspected. Further studies are required to fully delineate the role of a full bladder in US studies for suspected pediatric appendicitis.
Competing Interests: None declared.
Supplementary Material
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/cem.2016.23