Summations
-
The prevalence of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic was higher in females compared to males; however, this difference was not statistically significant.
-
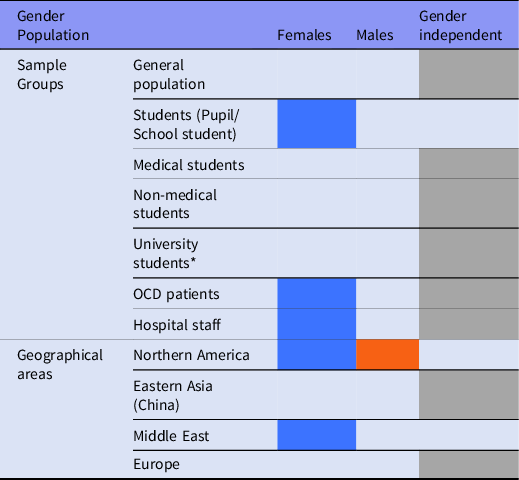
In the following groups, the female gender was identified as a possible risk factor regarding OCD during the COVID-19 pandemic: under-18 years students, hospital staff, and studies in the Middle East. In none of the categories investigated in this study, male gender was clearly identified as a risk factor.
-
Considering the role of differences between geographical regions, cultures, and economic status is essential when studying OCD.
Considerations
-
Assessing the gender differences regarding OCD during the COVID-19 pandemic has not been performed independently. Future studies should examine the differences between the two genders as their main topic, and not as a side factor.
-
Examining the OCD symptoms differences between the two genders has been neglected during the COVID-19 pandemic.
-
The groups in which the female gender has been introduced as a possible risk factor for OCD during the COVID-19 pandemic are not decisive, since the studies conducted in each of the geographical regions or sample groups had different objectives.
Introduction
In December 2019, a new respiratory disease was detected in Wuhan, China for the first time, named Coronavirus disease-19 (COVID-19) and get spread rapidly in other regions and became a global warning all around the world (Hu et al., Reference Hu, Sun, Dai, Deng, Li, Huang, Wu, Sun and Xu2020; Lipsitch et al., Reference Lipsitch, Swerdlow and Finelli2020) and therefore World Health Organization (WHO) declared it as a universal pandemic on 11 March 2020 less than 3 months after its presentation. Up to this moment that we write this article (27 July), about 195M people were infected by this virus and around 4M people were killed due to the current pandemic all around the world, and this statistical information confirmed that we can consider COVID-19 pandemic as one of the biggest public health challenges in the recent history.
The first findings of COVID-19 indicated that Coronavirus can spread in different ways such as respiration, eyes, nose, or mouth (Liu et al., Reference Liu, Ning, Chen, Guo, Liu, Gali, Sun, Duan, Cai, Westerdahl, Liu, Xu, Ho, Kan, Fu and Lan2020; Richard et al., Reference Richard, Kok, Meulder, Bestebroer, T., Lamers, Okba, Fentener van Vlissingen, Rockx, Haagmans, Koopmans, Fouchier and Herfst2020), and with polluted hands, those touched the surfaces that the virus has contaminated them (Kwok et al., Reference Kwok, Gralton and Mclaws2015; Karia et al., Reference Karia, Gupta, Khandait, Yadav and Yadav2020). Additionally, as we experienced some similar conditions like influenza (Jefferson et al., Reference Jefferson, Del Mar, Dooley, Ferroni, Al-Ansary, Bawazeer, van Driel, Nair, Jones, Thorning and Conly2011; Ahmed et al., Reference Ahmed, Zviedrite and Uzicanin2018), and Ebola (Osungbade & Oni, Reference Osungbade and Oni2014), we know this situation needs an emerging action on a major scale to expand public health level to prevent a disaster to human life. So experts published some advice like social distancing (Güner et al., Reference Güner, Hasanoğlu and Aktaş2020; Lotfi et al., Reference Lotfi, Hamblin and Rezaei2020), improving a self-hygiene level like several hands washing (Alzyood et al., Reference Alzyood, Jackson, Aveyard and Brooke2020; Güner et al., Reference Güner, Hasanoğlu and Aktaş2020; Mahmood et al., Reference Mahmood, Eqan, Pervez, Alghamdi, Tabinda, Yasar, Brindhadevi and Pugazhendhi2020; Lotfi et al., Reference Lotfi, Hamblin and Rezaei2020) and wearing masks (Lotfi et al., Reference Lotfi, Hamblin and Rezaei2020; Brooks et al., Reference Brooks, Butler and Redfield2020a), those can be effective to prevent COVID-19.
Forasmuch as we faced with same pandemics and experienced the impact of them on public mental health, like the 2009 H1N1 (Pfefferbaum et al., Reference Pfefferbaum, Schonfeld, Flynn, Norwood, Dodgen, Kaul, Donato, Stone, Brown, Reissman, Jacobs, Hobfoll, Jones, Herrmann, Ursano and Ruzek2012), and 2003 SARS outbreak (Hawryluck et al., Reference Hawryluck, Gold, Robinson, Pogorski, Galea and Styra2004; Cava et al., Reference Cava, Fay, Beanlands, Mccay and Wignall2005; Mak et al., Reference Mak, Chu, Pan, Yiu and Chan2009), we can hypothesis the same results for the COVID-19 pandemic (Hossain et al., Reference Hossain, Tasnim, Sultana, Faizah, Mazumder, Zou, Mckyer, Ahmed and Ma2020; Xiong et al., Reference Xiong, Lipsitz, Nasri, Lui, Gill, Phan, Chen-Li, Iacobucci, Ho, Majeed and Mcintyre2020a). Although it is accepted that everyone has a chance of getting infected by the COVID-19, but some studies concluded that people with mental illness had a greater risk of pneumonia and pneumococcal disease (Seminog & Goldacre, Reference Seminog and Goldacre2013). In addition, for people with mental illness, their underlying mental health may deteriorate or recur due to their high-potential stress compared to the general population (Yao et al., Reference Yao, Chen and Xu2020).
Among all mental diseases, we can point to obsessive-compulsive disorder (OCD) as a common and serious one. OCD had a high level of comorbidity with other mental diseases (Ruscio et al., Reference Ruscio, Stein, Chiu and Kessler2010; Quarantini et al., Reference Quarantini, Torres, Sampaio, Fossaluza, Mathis, Rosário, M., Fontenelle, Ferrão, Cordioli, Petribu, Hounie, Miguel, Shavitt and Koenen2011; Subramaniam et al., Reference Subramaniam, Abdin, Vaingankar and Chong2012), physical disorders (Subramaniam et al., Reference Subramaniam, Abdin, Vaingankar and Chong2012), and also had a connection with suicidal actions (Fernández de la K amath et al., Reference Kamath, Reddy and Kandavel2007; Torres et al., Reference Torres, Ramos-Cerqueira, Ferrão, Fontenelle, do Rosário and Miguel2011; Huz et al., Reference Huz, Nyer, Dickson, Farabaugh, Alpert, Fava and Baer2016; Cruz et al., Reference Cruz, Rydell, Runeson, D’onofrio, Brander, Rück, Lichtenstein, Larsson and Mataix-Cols2017). In several studies in different regions, OCD’s lifetime prevalence range mostly was calculated from 1.8% to 3.3% (Karno et al., Reference Karno, Golding, Sorenson and Burnam1988; Weissman et al., Reference Weissman, Bland, Canino, Greenwald, Hwu, Lee, Newman, Oakley-Browne, Rubio-Stipec and Wickramaratne1994; Mohammadi et al., Reference Mohammadi, Ghanizadeh, Rahgozar, Noorbala, Davidian, Afzali, Naghavi, Yazdi, Saberi, Mesgarpour, Akhondzadeh, Alaghebandrad and Tehranidoost2004; Ruscio et al., Reference Ruscio, Stein, Chiu and Kessler2010; Subramaniam et al., Reference Subramaniam, Abdin, Vaingankar and Chong2012; Jaisoorya et al., Reference Jaisoorya, Janardhan Reddy, Nair, Rani, Menon, Revamma, Jeevan, Radhakrishnan, Jose and Thennarasu2017), and OCD is mentioned as the fourth most common mental disease in some studies (Grant, Reference Grant2014; Veale & Roberts, Reference Veale and Roberts2014; Ansari et al., Reference Ansari, Mishra, Tripathi, Kar and Dalal2020; Asghar et al., Reference Asghar, Rehman, Shafiq, Siddiq, Zehravi, Khan, Asghar and Abedin2020).
OCD is a chronic mental illness that causes unwanted thoughts (obsessions), and repetitive behaviours (e.g. hand washing or checking), or mental acts, or compulsions, which can disrupt patients’ life (Veale & Roberts, Reference Veale and Roberts2014; Brock & Hany, Reference Brock and Hany2021).
As mentioned, the first findings suggested that hand washing is effective in reducing infections and is a preventive one against COVID-19 spreading, and society was encouraged to take this advice seriously, but excessive hand washing is one of the most common symptoms among 50% of OCD patients (Brady et al., Reference Brady, Adams and Lohr2010). So, this extra emphasis on hand sanitation may increase fear of contamination and therefore result in OCD symptoms worsening (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020). Also, various studies indicate that inflammatory cytokines are increased in OCD (Fontenelle et al., Reference Fontenelle, Barbosa, Luna, de Sousa, Abreu and Teixeira2012; Rao et al., Reference Rao, Venkatasubramanian, Ravi, Kalmady, Cherian and Yc2015; Karagüzel et al., Reference Karagüzel, Arslan, Uysal, Demir, Aykut, Tat and Karahan2019; Kutuk et al., Reference Kutuk, Tufan, Kilicaslan, Mutluer, Gokcen, Karadag, Yektas, Kandemir, Buber, Guler Aksu, Topal, Giray, Celik, Acikbas and Kutuk2020). Increased cytokine levels are involved in severe neurological disorders (Bodro et al., Reference Bodro, Compta and Sánchez-Valle2021). The pathophysiology of several psychiatric disorders including anxiety, depression, post-traumatic stress disorder, and OCD, is associated with these changes (Grace, Reference Grace2016; Raony et al., Reference Raony, Figueiredo, C., Pandolfo, Giestal-De-Araujo, Oliveira-Silva Bomfim and Savino2020). OCD patients might have remarkably higher plasma levels of IL-1β, IL-6, IL-17, TNF-α, CCL3, CXCL8, sTNFR1, and sTNFR2 (Fontenelle et al., Reference Fontenelle, Barbosa, Luna, de Sousa, Abreu and Teixeira2012; Rao et al., Reference Rao, Venkatasubramanian, Ravi, Kalmady, Cherian and Yc2015; Karagüzel et al., Reference Karagüzel, Arslan, Uysal, Demir, Aykut, Tat and Karahan2019; Kutuk et al., Reference Kutuk, Tufan, Kilicaslan, Mutluer, Gokcen, Karadag, Yektas, Kandemir, Buber, Guler Aksu, Topal, Giray, Celik, Acikbas and Kutuk2020). When an individual is infected with the coronavirus, depending on the local or peripheral presence of SARS-CoV2, the virus could lead to systemic inflammatory responses (Bodro et al., Reference Bodro, Compta and Sánchez-Valle2021). One of the important stages in the pathophysiology of COVID-19 is the binding of SARS-Cov2 to angiotensin-converting enzyme 2 (ACE2) in respiratory epithelial cells, and then blood vessels’ epithelial cells. This binding allows SARS-Cov2 to trigger a cytokine storm with significantly increased levels of IL-1, IL-6, and TNF (Mehta et al., Reference Mehta, Mcauley, Brown, Sanchez, Tattersall and Manson2020; Xiong et al., Reference Xiong, Liang and Wei2020b). Therefore, considering the higher levels of cytokines in OCD patients, the neuro-inflammatory mechanisms could be involved in the pathophysiology of the neuropsychiatric manifestations (Muccioli et al., Reference Muccioli, Pensato, Bernabè, Ferri, Tappatà, Volpi, Cani, Henry, Ceccaroni, Cevoli, Stofella, Pasini, Fornaro, Tonon, Vidale, Liguori, Tinuper, Michelucci, Cortelli and Bisulli2021).
OCD has become important for various reasons during the COVID-19 pandemic and has been the subject of studies, including this systematic review. The most important reason is the increase in the incidence of this disease (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Cox & Olatunji, Reference Cox and Olatunji2021). OCD-related behaviours are often seen in society, and even some behaviours that were subsequently rejected by health authorities, are performed abundantly by society members, such as washing hands after every contact with the environment, in a situation where the possibility of direct infection with Coronavirus through surface contact and environment has weakened, and now it is assumed that the virus is primarily transmitted from person to person through respiratory and oral aerosols and droplets (Rahman et al., Reference Rahman, Aziz, Hussein, Othman, Omer, S., Khalid, Abdulrahman, Amin and Abdullah2020). At the beginning of the outbreak, governments, public figures, and authorities responsible for health-related matters prompted society to wash their hands frequently (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020). Considering that based on some studies excessive washing, the feeling of being contaminated, and the fear of dirt are the most common cases that affect about 50% of patients (Brady et al., Reference Brady, Adams and Lohr2010), and taking into account the general fear of getting infected with the virus and the recommendations in health advisories regarding hand washing, the contamination fear might increase (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020), and the OCD symptoms might worsen (Reynolds et al., Reference Reynolds, Garay, Deamond, Moran, Gold and Styra2008). In addition, frequent cleaning habits becoming a normal and prevalent protective behaviour might cause contamination-related obsessions and compulsions, especially in individuals who have other types of obsessions and compulsions (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020). Also, according to recent literature, individuals who had been diagnosed with OCD before the current pandemic may be the group most affected by the pandemic among those with mental disorders (Fineberg et al., Reference Fineberg, Ameringen, Drummond, Hollander, Stein, D., Geller, Walitza, Pallanti, Pellegrini, Zohar, Rodriguez, Menchon, Morgado, Mpavaenda, Fontenelle, Feusner, Grassi, Lochner, Veltman, Sireau, Carmi, Adam, Nicolini and DELL’osso2020), and in a situation where many dimensions of mental illnesses, including OCD, are undiagnosed in pandemic conditions and the possibility of conducting targeted studies is weakened, this disease and its various aspects of the relationship with COVID-19 pandemic became the subject of this systematic review. According to recent literature, individuals who had been diagnosed with OCD prior to the current pandemic may be the group most affected by the pandemic among those with mental disorders (Fineberg et al., Reference Fineberg, Ameringen, Drummond, Hollander, Stein, D., Geller, Walitza, Pallanti, Pellegrini, Zohar, Rodriguez, Menchon, Morgado, Mpavaenda, Fontenelle, Feusner, Grassi, Lochner, Veltman, Sireau, Carmi, Adam, Nicolini and DELL’osso2020), and therefore this disease has gained lots of attention from researchers worldwide.
This pandemic will be ended soon or late, but according to previous experiences, its physical and mental consequences will remain for some time. Early intervention is always one of the most effective ways to prevent or control diseases at low levels of progression (Pozza et al., Reference Pozza, Mucci and Marazziti2020). But when society and policymakers face situations like the COVID-19 pandemic that impose enormous and unforeseen costs, early intervention on various issues, especially mental disorders, becomes impossible. Under these circumstances, identifying at-risk groups can direct the limited and damaged resources of society to them and thus achieve greater efficiency. The present study, therefore, aims to identify gender-related risk groups in relation to OCD and to provide resources for early intervention, especially in relation to education (stress management, OCD symptoms, and the COVID-19 pandemic).
Although the OCD has attracted the global attention of researchers due to the clearer demonstrations it has generated in the society during the COVID-19 pandemic, the previous studies performed in this area acted so separately when comes to the objectives of the studies and the demographical sample groups that were investigated. Thus, there was a lack of a systematic review to guide future studies on this basis, and this study seeks to fill this gap. This systematic review aims to evaluate the possible changes in the relationship between the OCD and gender due to the circumstances created by the COVID-19 pandemic. This study also seeks to identify gender-related at-risk groups regarding OCD during the pandemic and to act as a guide for future studies to focus the resources on those who are specified as at-risk in this systematic review. This study also tries to investigate the differences among different geographical regions with regard to mentioned relationship and highlights the importance of cultural differences in OCD, as the peripheral factors are of the most important factors affecting this disease.
Material and methods
The systematic review was performed based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) recommendations for the literature search and screening, including studies and reporting results (Moher et al., Reference Moher, Liberati, Tetzlaff, Altman and P.2009).
Search strategy
In order to carry out this systematic review, we performed a comprehensive search in Medline, Scopus, and Web of Science databases from their inception to the 10th of August 2021 to identify the literature investigating the role of gender on OCD prevalence and symptom severity during the COVID-19 pandemic. A search strategy was performed based on the combination of three groups of OCD, COVID-19, and different forms of keywords relevant to gender. In the first stage, the following keywords were combined through OR: Female, Male, Women, Men, Sex, Sex Factors. Then results from the mentioned step were combined with OCD and COVID-19 keywords through AND. Keywords were chosen by searching MeSH terms, reviewing related articles, and consulting with researchers. In the end, we investigated the reference lists of our included studies to identify and include further relevant literature in case we missed them during the mentioned steps.
On the 23rd and 24th of July and 10th of August 2021, we updated our search and repeated the above steps. Table 1 shows details of the search strategy for each database.
Table 1. Search strategy

The studies included by following criteria:
(1) Studies investigating the risk factors (including gender) for OCD during the COVID-19 pandemic. (2) The article was published in English.
Our exclusion criteria were:
(1) Reviews, letters, conference papers, and editorials. (2) We also excluded studies that examined OCD not independently but as part of mental health, and even identified the role of gender. Because the impact of other mental disorders such as depression, anxiety, etc. on the results cannot be determined.
Two authors (EJ & AA) separately searched the databases and screened the title and abstract of articles based on the inclusion/exclusion criteria. Once the primary screening, potentially eligible articles were screened by two reviewers (EJ & AA) based on reviewing the full text, in keeping with inclusion/exclusion criteria. The disagreement on articles was resolved by discussion between two authors (EJ & AA); otherwise, the third author (MR) would be consulted. Our search method resulted in 197 articles, of which 24 met our inclusion criteria. Figure 1 illustrates the diagram of the literature search and inclusion/exclusion criteria.

Fig. 1. Diagram of the literature search (PRISMA 2009 Flow Diagram).
Data extraction
Two independent authors extracted the required data and reported the findings based on PRISMA (Liberati et al., Reference Liberati, Altman, Tetzlaff, Mulrow, Gøtzsche, Ioannidis, Clarke, Devereaux, Kleijnen and Moher2009). A self-defined table was used for extracting data including first author name, publication date, country, study design, sample number, age and gender characteristics, OCD parameters and measurement tool, Categorical variable’ (Gender) association parameters, Population, and significant results (Table 2).
Table 2. Characteristics of included studies

Risk of bias assessment
We used the Newcastle−Ottawa scale (Stang, Reference Stang2010) to evaluate the cohort studies. This scale consists of three groups: selection, comparability, and outcome. A cohort study can get a maximum of 1 score for each question of selection and outcome, and a maximum of 2 scores for comparability. Thus, a study can get a maximum of 9 scores from the Newcastle−Ottawa scale. Table 3 shows the result of evaluating cohort studies.
Table 3. Results of evaluating cohort studies

We also used an adapted version of the Newcastle−Ottawa scale (Stang, Reference Stang2010) to evaluate the cross-sectional studies. This scale consists of three groups: selection (maximum of 5 scores), comparability (maximum of 2 scores), and outcome (maximum of 3 scores). A cross-sectional study can get a maximum of 1 score for each question of outcome and 3 questions of selection, and a maximum of 2 scores for comparability and one question of selection. Thus, a study can get a maximum of 10 scores from the Newcastle−Ottawa scale. Table 4 shows the result of evaluating cross-sectional studies.
Table 4. Results of evaluating cross-sectional studies

Data synthesis
The prevalence of OCD in the total population and the two genders was pooled in a meta-analysis with a confidence interval of 95%. The Cochrane Q p-value and I 2 statistics were used to define statistical heterogeneity. If there was no significant heterogeneity (I 2 less than 50% or Cochrane Q with a p-value > 0.05), pooled estimates were generated using the fixed-effect model; otherwise, the random-effect model was applied when significant heterogeneity was found. Due to the inappropriate number of studies reporting the prevalence of OCD, publication bias was not performed. Comprehensive Meta-Analysis version 3 was used for all statistical analysis.
Results
By conducting a comprehensive search in Medline, ScienceDirect Scopus, and Web of Science databases using OCD, COVID-19, and gender-related keywords, 197 articles were obtained, of which 24 met our inclusion criteria and we present them based on the study population type, the country where the study was conducted, and the obtained results. Overall, more than half of the articles stated the role of gender in OCD during the COVID-19 pandemic, with 13 articles identifying gender as a risk factor but 11 articles declaring OCD as independent of gender. Several articles referred to the role of the female gender regarding OCD, some to the role of the male gender, and some did not identify gender as a risk factor. Studies have been conducted in North America, Europe, the Middle East, and China. The main part of the articles belonged to two regions of Europe and the Middle East. Except for three cases that were cohort studies, the rest of the studies used the cross-sectional method. In the majority of articles, the participants were more female than male, a difference that was severe in a significant number of studies. Table 2 presented the general characteristics of included studies.
As Table 2 demonstrates, the studies have many differences from each other. They have been carried out in different geographical areas, examined various sample groups, and had different objectives for their study. Therefore, for a better and more targeted investigation, the studies were divided into different subgroups to reduce their heterogeneity from each other, and by examining these subgroups, specific results and conclusions can be reached. These subgroups are presented in detail in the discussion section. One of these divisions was studies that investigated the prevalence of OCD during the COVID-19 pandemic, for which a meta-analysis was conducted.
The total prevalence of OCD during the COVID-19 pandemic was reported in seven studies (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021) and results of quantitative synthesis with random effects analysis found a 41.2% OCD prevalence (95% CIs: 27.8–55.9%; I 2: 99.07%) (Fig. 2).

Fig. 2. Prevalence of OCD in total population.
The prevalence of OCD in both genders was investigated in five studies (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), and the meta-analysis using random effect analysis indicated that the female gender had a OCD prevalence of 47.1% (95% CIs: 30.3–64.5%; I 2: 98.62%), while the male gender had a prevalence of 39.1% (95% CIs: 23.8–56.9%; I 2: 97.38%) (Fig. 3). Therefore, compared to the male gender, OCD prevalence was higher in the females, however, this difference was not statistically significant.

Fig. 3. Prevalence of OCD among genders.
Discussion
The current study is the first one to compare being female or male as a risk factor for OCD during the COVID-19 pandemic. As we know, the COVID-19 pandemic is one of the worst diseases that mankind has faced during the last century. Several studies indicated that the impression of this pandemic on mental health is remarkable (Hossain et al., Reference Hossain, Tasnim, Sultana, Faizah, Mazumder, Zou, Mckyer, Ahmed and Ma2020; Xiong et al., Reference Xiong, Lipsitz, Nasri, Lui, Gill, Phan, Chen-Li, Iacobucci, Ho, Majeed and Mcintyre2020a; Vindegaard & Benros, Reference Vindegaard and Benros2020). The containment measures implemented to reduce the progression of the COVID-19 pandemic can increase the risk of serious mental disorders, including OCD (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020b). The recommendations by WHO and other health organisations can cause difficulties for OCD patients and spread the prevalence of OCD among the general population. One of the most important and troublemaking recommendations in this area is hand washing (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020). A process that is also used to identify OCD in individuals, considering the fact that hand washing is one of the main symptoms of OCD (Brady et al., Reference Brady, Adams and Lohr2010). In a pandemic, government and community resources are under intense pressure, which deprives them of the ability to manoeuver properly when comes to mental health issues. Prolonged quarantines, business downturns, and the deaths of community members put countries in a difficult position. In these circumstances, attention to mental health, which does not show an immediate impact on society, is not a priority for policymakers. Therefore, the mental health of the community suffers more, and its long-term effects are more severe. So, identifying at-risk groups can provide sufficient justification for investment and government attention, and thus, at a lower cost, improve the mental health of the community and reduce its long-term effects. With the explanations provided, it is clear that OCD is one of the disorders that is particularly affected by the pandemic and identifying groups at risk of this disease, especially whether women are at higher risk or men, can create better conditions for community mental health at a lower cost (Chu et al., Reference Chu, Alam, Larson and Lin2020; Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020b; Galea et al., Reference Galea, Merchant and Lurie2020).
Several studies have previously evaluated such correlation as independent of the status of the COVID-19 outbreak. A meta-analysis by Fawcett et al. (Reference Fawcett, Power and Fawcett2020), was performed to investigate the global prevalence of OCD and examine whether females are at higher risk than males and explore alternative moderators of OCD prevalence. Their search was fulfilled until January 2017 and 34 articles were ultimately included. Only the studies were included that the age range of their participants was more than 18 years old. They found that in a typical sample, females are 1.6 times more likely to have OCD compared to males, with a lifetime prevalence rate of 1.5% in females and 1.0% in males. In addition, women are at higher risk of experiencing OCD in their lifetime than men (Fawcett et al., Reference Fawcett, Power and Fawcett2020). Also, a systematic review by Mathis et al. (Reference Mathis, Alvarenga, Funaro, Torresan, Moraes, Torres, Zilberman and Hounie2011) was conducted to investigate the gender differences in clinical, genetic, or familial aspects of OCD. This study indicated that male patients are more likely to present early onset of symptoms and chronic course of the disorder. On the other hand, female patients present more contamination/cleaning symptoms (Mathis et al., Reference Mathis, Alvarenga, Funaro, Torresan, Moraes, Torres, Zilberman and Hounie2011). These two studies have examined the state of OCD among men and women in a normal situation of society, but for the reasons mentioned, examining this relationship in a pandemic situation is a necessity to identify more sensitive groups.
Our search method resulted in 24 articles included, and noteworthy, except for three articles that used the cohort study method (Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021), all the other articles were based on the cross-sectional study method.
The articles reviewed in this systematic review were from different regions and countries, one-third of which belong to the Middle East and the other third to Europe, which could affect the generalizability of the study results.
The human development index (Roser, Reference Roser2014), gender equality (Inglehart et al., Reference Inglehart, Norris, Welzel, Inglehart, Norris and Welzel2002; Ortenblad et al., Reference Ortenblad, Marling and Vasiljevic2017), and the rate of employed women compared to men (Tzannatos, Reference Tzannatos1999; Elder & Schmidt, Reference Elder and Schmidt2004) are the indicators that can influence the stated results. Considering the fact that the rate of all these indicators is different around the world, the Middle East and Europe cannot act as a sample model, and we recommend the Middle Eastern and European researchers investigate the effects of these indicators on the prevalence and symptom severity of OCD between males and females.
Before continuing with the article, we should refer to one of the articles that were done in Portugal and stated that the study population was selected from a Portuguese sample (higher than 18 years old), but then stated that more than 92% of the participants suffered from psychological disorders. Also, nearly 67% of the participants declared that they are suffering from physical disorders. These numbers are unusual for a sample that has selected its members from the general population. Therefore, this study loses the score of the first question (Representativeness of the sample) in our qualitative analysis (Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021).
As mentioned, the studies included in this systematic review have many differences from each other. They have been carried out in different geographical areas, examined various sample groups, and had different objectives for their study. Therefore, for a better and more targeted investigation, the studies were divided into different subgroups to reduce their heterogeneity from each other, and by examining these subgroups, specific results and conclusions can be reached.
As mentioned, in order to better and more targeted investigation, the studies were divided into different subgroups, and in one of them, we investigated the prevalence of OCD during the COVID-19 pandemic. Seven studies assessed the prevalence of OCD (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021) and results of the meta-analysis showed a 41.2% OCD prevalence. All studies were based on the cross-sectional method. Of the seven studies (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), three were conducted in the Middle East (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), one in the United States (McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021), one in Europe (Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020), and one in China (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020). A study also selected its population from all over the world (Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021). These studies used five different methods to assess OCD status. Three studies used the OCI-R method (Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021). The other methods including Y-BOCS (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020), MOCI (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020), and ZF-OCS (Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021) were each selected by one study. A study also stated that it used a self-designed instrument to investigate OCD status, which caused it to lose one point in the selection section of the qualitative analysis (McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021). These studies selected their study sample from three different groups. Two studies were conducted among under 18 years old students (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021), three studies among university students (Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), and two studies among the general population (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021). The largest number of sample groups in studies was 2186, which belonged to a study conducted among the general population in the Middle East (AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021), and the lowest number of sample groups was related to another study in the Middle East with the number of 150, which was conducted among under 18 years old students (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020). In the qualitative analysis (Newcastle−Ottawa scale) conducted for these studies, two studies scored 8 points (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021), three studies scored 7 points (Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), one study scored 6 points (McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021), and one study scored 5 points (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020). The two studies that had the lowest scores also had the smallest number of samples (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021), so one studied 150 people (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020) and the other 280 people (McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021). Both studies were conducted among under 18 years old students (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021). Also, the two studies with the highest scores were both conducted among the general population (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021).
The pre-COVID-19 meta-analysis that was reviewed at the beginning of the discussion section reported that overall current, period, and lifetime estimates of OCD prevalence were 1.1%, 0.8%, and 1.3%, respectively (Fawcett et al., Reference Fawcett, Power and Fawcett2020). Furthermore, in several studies, OCD’s lifetime prevalence was calculated from 1.8% to 3.3% (Karno et al., Reference Karno, Golding, Sorenson and Burnam1988; Weissman et al., Reference Weissman, Bland, Canino, Greenwald, Hwu, Lee, Newman, Oakley-Browne, Rubio-Stipec and Wickramaratne1994; Mohammadi et al., Reference Mohammadi, Ghanizadeh, Rahgozar, Noorbala, Davidian, Afzali, Naghavi, Yazdi, Saberi, Mesgarpour, Akhondzadeh, Alaghebandrad and Tehranidoost2004; Ruscio et al., Reference Ruscio, Stein, Chiu and Kessler2010; Subramaniam et al., Reference Subramaniam, Abdin, Vaingankar and Chong2012; Jaisoorya et al., Reference Jaisoorya, Janardhan Reddy, Nair, Rani, Menon, Revamma, Jeevan, Radhakrishnan, Jose and Thennarasu2017). The results of the current meta-analysis show a significant difference from the results of studies conducted before the COVID-19 pandemic and indicate a sharp increase in the prevalence of OCD. This higher prevalence of OCD during the COVID-19 pandemic might be due to several reasons. One of these reasons can be related to the health recommendations of the authorities at the beginning of the outbreak, who prompted society to wash their hands frequently (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020). Considering that OCD status in a high number of patients is affected by excessive washing, the feeling of being contaminated, and the fear of dirt (Brady et al., Reference Brady, Adams and Lohr2010), and taking into account the general fear of getting infected with the virus, the contamination fear might increase (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020), and the OCD symptoms might worsen (Reynolds et al., Reference Reynolds, Garay, Deamond, Moran, Gold and Styra2008). In addition, frequent cleaning habits becoming a normal and prevalent protective behaviour might cause contamination-related obsessions and compulsions (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020). Another reason can be related to stress and anxiety as two risk factors of OCD (Weingarden et al., Reference Weingarden, Renshaw, Wilhelm, Tangney and Dimauro2016; Adams et al., Reference Adams, Kelmendi, Brake, Gruner, Badour and Pittenger2018; Raposo-Lima & Morgado, Reference Raposo-Lima and Morgado2020), which have increased due to the conditions resulting from the COVID-19 pandemic in various social groups such as hospital staff, university students, etc. (Couarraze et al., Reference Couarraze, Delamarre, Marhar, Quach, Jiao, Dorlhiac, Saadaoui, Liu, A., Dubuis, Antunes, Andant, Pereira, Ugbolue, Baker, Clinchamps and Dutheil2021; Durbas et al., Reference Durbas, Karaman, Solman, Kaygisiz and Ersoy2021; Özdin & Bayrak Özdin, Reference Özdin and Bayrak Özdin2020), which may have subsequently caused an increase in the prevalence of OCD. Another factor can be related to not receiving proper medical and support services during the pandemic. As a result of the quarantine, many support centres for mental patients were forced to close or reduce the provision of services, and people’s access to these centres was disrupted. It is also possible that in order to be less present in society and reduce the possibility of contracting the Coronavirus, people have given up going to medical centres and receiving services, which may have caused mental problems or added to their previous problems. Finally, another reason can be related to the non-adaptation of the methods of assessing the status of OCD with conditions such as the COVID-19 pandemic, which has caused the prevalence of OCD to be falsely shown. For example, some OCD behaviours that have emerged or increased during the pandemic will continue permanently in some people, but they will probably subside after a while in the majority of society. In this situation, it does not seem correct to consider these people as suffering from OCD. Also, some behaviours that are considered OCD behaviour in various assessment tools have inevitably increased during the pandemic, and the sum of these factors has probably caused the prevalence of OCD to be overestimated.
In another part of the meta-analysis, five studies that investigated the prevalence of OCD in both genders during the COVID-19 pandemic were examined (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021). The results of the meta-analysis indicated that the female gender had an OCD prevalence of 47.1%, while the male gender had a prevalence of 39.1%. Therefore, compared to the male gender, OCD prevalence was higher in the females; however, this difference was not statistically significant. These five studies were conducted in three different geographical regions, three of which were in the Middle East (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021). They also used four different methods to evaluate the status of OCD (OCI-R (AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), Y-BOCS (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020), MOCI (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020), and a self-designed instrument (McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021)). Two of these studies were conducted among under 18 years old students (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021), one among medical students, and two among the general population (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021). The studies among the general population got the highest qualitative analysis score (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021),and the studies among under 18 years old students got the lowest qualitative analysis score (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021).
The findings of this meta-analysis are consistence with the meta-analysis that investigated the global prevalence of OCD before the COVID-19 pandemic, which identified the female gender as a risk factor for OCD prevalence (Fawcett et al., Reference Fawcett, Power and Fawcett2020). This higher prevalence of OCD among women can be due to the greater vulnerability of females to risk factors related to OCD during the COVID-19 pandemic. For example, because of the pandemic, increasing anxiety was imposed on society and according to a study by Özdin et al, women suffered more. This study reported that 45.1% of its sample scored above the cut-off point for anxiety, and women had higher levels of anxiety and health anxiety (Özdin & Bayrak Özdin, Reference Özdin and Bayrak Özdin2020). Since OCD was classified as an anxiety disorder until recently and the role of anxiety in OCD is clear (Weingarden et al., Reference Weingarden, Renshaw, Wilhelm, Tangney and Dimauro2016), this factor is one of the justifications for the higher prevalence of OCD among females. On the other hand, the pandemic caused damage to the economy and many people lost their jobs. In this meta-analysis, five studies examined the prevalence of OCD in both genders during the pandemic (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021). Three of these five studies were conducted in the Middle East (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021). Therefore, examining the situation in the Middle East in terms of these factors can be helpful. According to the World Bank, the unemployment rate of men in the Middle East and North Africa increased from 7.1% in 2019 to 9.3% in 2021. But in the same period, women suffered more, and the unemployment rate increased from 17.4% to 19.7%. Also, the high unemployment rate is considered a risk factor for OCD (Mohammadi et al., Reference Mohammadi, Ghanizadeh, Rahgozar, Noorbala, Davidian, Afzali, Naghavi, Yazdi, Saberi, Mesgarpour, Akhondzadeh, Alaghebandrad and Tehranidoost2004). Therefore, the higher rate of unemployment among women may serve as a justification factor for them being a possible risk factor for OCD.
Also, the rate of domestic violence against women increased during the COVID-19 pandemic (Kourti et al., Reference Kourti, Stavridou, Panagouli, Psaltopoulou, Spiliopoulou, Tsolia, Sergentanis and Tsitsika2021; Women & Count, Reference Women and Count2021). According to a report by United Nations, violence against women has increased to unprecedented levels during the pandemic (Women & Count, Reference Women and Count2021). In a report, it is mentioned that trends regarding domestic violence are starting to emerge on a global scale, and various numbers from 25% to higher percentages have been mentioned regarding this increase (Boserup et al., Reference Boserup, Mckenney and Elkbuli2020). Also, domestic violence can act as a risk factor for OCD directly or indirectly through increasing anxiety (Ahmadzad-Asl et al., Reference Ahmadzad-Asl, Davoudi, Zarei, Mohammad-Sadeghi and Rasoulian2016; Moasheri et al., Reference Bibi Narjes, Gholamreza, Masoomeh, Faezeh and Vahideh2020). Therefore, in this situation, women can be considered as a risk factor for OCD.
One of the issues addressed in similar previous reviews has been the comparison of obsessive-compulsive symptoms among women and men. In the present article, it was not possible to compare the symptoms properly between men and women because none of our included studies were specifically designed to compare the symptoms of OCD between the two genders, but in this section, we present a number of symptoms that were specifically mentioned in our included studies.
A study conducted among the general population in the United States found that men are at more risk for contamination obsessions and contamination phobias in comparison with women (Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021). Another study conducted in Iran among students between the ages of 13 and 19 stated that the prevalence of OCD symptoms and severity of the following subscales of OCD (Checking, Washing, Strictness, Doubting subscales) was remarkably higher in females compared to males (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020). Another study was performed to assess prevalence and correlates of new-onset obsessive-compulsive symptoms among people with possible mental issues and found a high correlation between obsessions related to dirt, germs, and viruses, and male gender. It means that the male gender had a significant correlation with being worried about getting contaminated with dirt, germs, and viruses, compared to other respondents. On the other hand, this study stated that there is no significant correlation between gender as a variable and compulsive hand washing (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020) (Table 5).
Table 5. OCD symptoms

In another division, the study population of the studies was investigated. The studies we reviewed in this article selected their study population from different groups of the community. To reduce the risk bias resulting from heterogeneity in the studied populations, we split the studies into several demographical sub-population groups (including general population, students, medical students, non-medical students, university students, hospital staff, and obsessive-compulsive patients), and examined the mentioned relationship within these newly created categories.
Ten studies selected their target population from the general population (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021; Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021; Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021) (two of the articles in this section will be reviewed in the section related to hospital staff either since the studies examined both populations (Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021)), which five cases were conducted in the Middle East (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021), two cases in the US (Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021) and two cases in China (Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020). There was also a case in Europe (Portugal) (Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021). Two studies in China both found that gender was not a risk factor for OCD during the current pandemic (Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020). However, two studies conducted in the United States did not show such a correlation with each other that one of them stated that female gender was a risk factor (Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021) and the other identified male gender as a risk factor (Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021). Of the five studies conducted in the Middle East (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021), two were in Saudi Arabia (Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021), one of which identified male gender as a risk factor (AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021), but the other did not consider gender as a risk factor (Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021), which is also supported by another study in Iran (Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021). In contrast, two other studies in Lebanon (El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021) and Egypt (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021) identified female gender as a risk factor. The study conducted in Europe (Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021), like the Chinese studies (Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020), did not consider gender a risk factor. As is clear, studies conducted among the general population do not give us a definite conclusion, but overall, studies that considered gender as a non-risk factor weighed more. Two articles specifically examined this relationship among K-12 and under-19 years students (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021). Both of these studies, conducted in the United States (McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021) and Iran (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020), emphasised the role of the female gender in OCD during the COVID-19 pandemic. As it turns out, the role of the female gender in this section is clear. Two studies examined the status of OCD and its relationship to gender during the COVID-19 pandemic among medical students (Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021). Both studies conducted in this section did not consider gender as a risk factor at all, one of which selected its study population from all around the world (Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021), which adds to its credibility. Also, three studies examined this relationship among non-medical students (Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020; Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021), none of whom identified male gender as a risk factor. One in the UAE identified female gender as a risk factor (Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020), and two other studies in Europe did not consider gender a risk factor (Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021). One study also examined this relationship between students of a university in China, including both medical students and non-medical students, and identified the males aged < 26 as a risk factor; however, they declared that the rates of possible OCD were not remarkably different between males and females aged ≥ 26 years (Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020). In general, studies conducted among university students did not consider gender as a risk factor. Two studies examined this relationship among obsessive-compulsive patients (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021). None of the two studies which was conducted in Europe considered the male gender a risk factor (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021). As in the first section, which was done among the general population, the conflicting results of studies conducted among obsessive-compulsive patients do not lead us to a definite conclusion. Four studies also examined this relationship among hospital staff and health care workers (Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020; Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021). A study in Europe did not consider gender a risk factor (Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021), but two studies conducted in China yielded conflicting results, with one of them considering gender not as a risk factor (Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020), as in a European study, but the second study emphasised the role of female gender in OCD (Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020). Also, a study in Egypt that examined the mentioned relationship among the general population and health care workers also emphasised the role of the female gender (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021). In this section, we see that the role of the female gender is more obvious so that none of the four articles in this section introduced male gender as a risk factor, and two articles directly introduced female gender as a risk factor (Fig. 4).

Fig. 4 Results distribution (whether gender is a risk factor and if so which gender) in different demographical subgroups. *University Students consist of both medical and non-medical students. A study in this section identified the males aged <26 as a risk factor, however, they declared that the rates of possible OCD were not remarkably different between males and females aged ≥26 years (This study is considered in this figure).
If we examine the studies not according to the type of study population, but according to the country and region in which they were conducted, we may reduce the risk biases related to different regions and thus reach new conclusions. To reduce the risk bias due to differences in the geographical regions of the studies, we split the studies into several geographical sub-population groups (including North America, Eastern Asia (China), Middle East, Europe), and examined the mentioned relationship within these newly created categories.
In studies conducted in the United States (Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021) and Canada (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020), although they consider gender as a risk factor but we can’t point at a specific gender, with two studies emphasising the role of female gender (Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021) and two studies emphasising the role of male gender in OCD (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021). The study conducted in Canada, although in some sections introduced male gender as a risk factor (the obsessions related to dirt, germs, and viruses), but in some late items (compulsive hand washing) did not consider gender as a risk factor at all (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020). Studies in China (Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020; Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020), such as those in North America, do not provide clear results so that two of them did not consider gender as a risk factor (Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020), and from the other two studies, one emphasised the role of female gender (Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020) and the other emphasised the role of the male gender under 26 years old. They also declared that the rates of possible OCD were not remarkably different between males and females aged ≥ 26 years (Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020). But studies in Europe and the Middle East show clearer results, and the role of the female gender is more evident in these two regions. Of the eight studies conducted in the Middle East (Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020; Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), four directly emphasised the role of female gender in this regard (Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020; Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021), three did not consider gender as a risk factor (Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), and only one study identified male gender as a risk factor (AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021). The clarity of the role of female gender in this regard in the Middle East is intensified by the elimination of the results of Saudi Arabia (Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021) so that out of the remaining six studies (Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020; Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), four cases of the female gender are introduced as a risk factor (Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020; Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021). Two other studies still do not introduce the male gender as a risk factor (Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021). Noteworthy that in neither of the two studies conducted in Saudi Arabia, female gender was considered as a risk factor (Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021).
The studies conducted in Europe provide different results from the studies in the Middle East. Of the seven studies conducted in Europe (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020; Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021; Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021; Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021), none considered male gender as a risk factor, so that two of them directly emphasised the role of female gender (Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020; Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021) and the other five did not consider gender as a risk factor at all (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021; Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021) (Fig. 5).

Fig. 5 Results distribution (whether gender is a risk factor and if so which gender) in different geographical locations. * A study in this section (categorized in male results) although in some items introduced male gender as a risk factor (the obsessions related to dirt, germs, and viruses), but in some late items (compulsive hand washing) did not consider gender as a risk factor at all. ** A study in this section (categorized in male results) emphasized the role of the male gender under 26 years old. But they also declared that the rates of possible OCD were not remarkably different between males and females aged ≥26 years.
Considering the set of these explanations, in the following groups, the female gender may have acted as a risk factor: students (under 18 years old), hospital staff and studies performed in the Middle East. In none of the categories, male gender was clearly identified as a risk factor regarding OCD. And finally, in the following groups, gender was not identified as a risk factor: medical students, university students, and possibly the general population. Table 6 shows major results of each population and whether in each of the groups surveyed in this systematic review, gender was a risk factor, and if so, which gender.
Table 6. The major results of each population whether gender was a risk factor or not, and if so, which gender
* University students consist of both medical and non-medical students.
Different hypotheses can be proposed for the obtained results. One of the conclusions made is the possibility of the female gender being a risk factor for OCD in the Middle East. In a study by Mohammadi et al, it was reported that the occupational variables of ‘business’ and ‘housewife’ decreased and increased the probability of OCD, respectively (Mohammadi et al., Reference Mohammadi, Ghanizadeh, Rahgozar, Noorbala, Davidian, Afzali, Naghavi, Yazdi, Saberi, Mesgarpour, Akhondzadeh, Alaghebandrad and Tehranidoost2004). On the other hand, according to World Bank reports, the unemployment rate of men in the Middle East and North Africa in 2018 was 7.8%. This is while the unemployment rate of women was 17.8% in the same year. Also, from 2010 to 2018, the highest unemployment rate for men was 8.2%, while the lowest unemployment rate for women was 17.1%. Since the COVID-19 pandemic started in 2019, many jobs in society were damaged. In this situation, the unemployment rate of men increased from 7.1% in 2019 to 9.3% in 2021. But in the same period, women suffered more, and the unemployment rate increased from 17.4% to 19.7%. In addition, the global unemployment rate for women in 2018 was 5.6%, and this number increased from 5.5% to 6.4% between 2019 and 2021. Therefore, we see that in the Middle East, women suffer from a higher unemployment rate and are more affected during the pandemic. Taking into account that being unemployed is considered a risk factor for OCD, therefore, the possibility of women being a risk factor in the Middle East can be justified in this way. In addition, a study by Williams et al demonstrates that lower levels of education and fewer years of educational attainment were associated with more compulsive symptoms (Williams et al., Reference Williams, Taylor, Himle and Chatters2017). The literacy rate for men in the Middle East and North Africa in 2020 was 86%, while it was 73% for women. In the meantime, the literacy rate in the world was 90% for men and 83% for women. Therefore, a greater difference in the literacy rate of women in the Middle East and the world is visible, and this point may serve as another justifying factor for women being a risk factor for OCD in the Middle East.
The possible causes cited for the Middle Eastern results have worked in the opposite way in Europe. As mentioned, it was concluded that in Europe, gender did not act as a risk factor. The unemployment rate for men in 2018 was 7%, and in the same year for women, it was 7.6%. Also, from 2019 to 2021, the unemployment rate for men increased from 6.4% to 6.7% and for women from 7% to 7.5%. Therefore, in Europe, the unemployment rate between men and women is close to each other, and there is no significant difference (similar to what was reported in the Middle East) between the two genders during the pandemic. On the other hand, the literacy status of society in Europe is generally better. In 2016, in Central Europe and Balkan, the literacy rate for both men and women was 99%. In this way, the two factors of ‘high unemployment rate’ and ‘high illiteracy rate’, which act as risk factors for OCD, are weak in Europe.
One of the other conclusions made is the possibility of the female gender being a risk factor for OCD among under 18 years old students. We know that one of the effects of the pandemic was the imposition of distance learning on students. In many countries, in order to protect the lives of students and prevent the cycle of virus transmission, regular school education was replaced by distance education. Radwan et al studied the perceived stress level in distance learning students during the COVID-19 period and found that female students had remarkably higher perceived stress levels compared to male students. They also had a greater chance of having moderate stress compared to males (Radwan et al., Reference Radwan, Radwan, Radwan and Pandey2021). On the other hand, stress is an important factor affecting OCD and may act as both a triggering and aggravating factor (Raposo-Lima & Morgado, Reference Raposo-Lima and Morgado2020). Stress also leads to neuronal atrophy in frontal cortices, the caudate part of the dorsomedial striatum, and the hippocampus parallel with hypertrophy in the putamen part of the dorsolateral striatum and amygdala. These neurobiological changes are consistent with the neurological abnormalities reported in OCD (Adams et al., Reference Adams, Kelmendi, Brake, Gruner, Badour and Pittenger2018). Therefore, one of the possible hypotheses of this section can be the effect of distance learning and the greater stress caused by it in females, making this gender a possible risk factor for OCD during the pandemic.
In fact, one of the critical effects of the COVID-19 pandemic was the imposition of increasing stress on society (Couarraze et al., Reference Couarraze, Delamarre, Marhar, Quach, Jiao, Dorlhiac, Saadaoui, Liu, A., Dubuis, Antunes, Andant, Pereira, Ugbolue, Baker, Clinchamps and Dutheil2021; Durbas et al., Reference Durbas, Karaman, Solman, Kaygisiz and Ersoy2021), considering that stress is viewed as a risk factor for OCD (Adams et al., Reference Adams, Kelmendi, Brake, Gruner, Badour and Pittenger2018; Raposo-Lima & Morgado, Reference Raposo-Lima and Morgado2020), the way both genders face this increasing stress in different groups of society or geographical regions can justify some of the results obtained.
Regarding the hospital staff, the role of the female gender as a risk factor for OCD is also remarkable. One of the effects of the pandemic was the heavy workload imposed on hospital staff and the healthcare workers were on the front line during this crisis. A study by Couarraze et al. demonstrates that healthcare workers experienced a major stressful event and the highest levels of stress were recorded. They also declared that females had systematically higher levels of work-related stress than males (Couarraze et al., Reference Couarraze, Delamarre, Marhar, Quach, Jiao, Dorlhiac, Saadaoui, Liu, A., Dubuis, Antunes, Andant, Pereira, Ugbolue, Baker, Clinchamps and Dutheil2021). As mentioned, stress may both trigger and aggravate OCD (Adams et al., Reference Adams, Kelmendi, Brake, Gruner, Badour and Pittenger2018; Raposo-Lima & Morgado, Reference Raposo-Lima and Morgado2020). Therefore, considering that more stress has been imposed on the female hospital staff, the mentioned relationship can be justified in this way.
Another finding was that most likely, gender did not act as a risk factor for OCD among university students (both medical and non-medical students). As we mentioned, stress is considered a risk factor for OCD (Adams et al., Reference Adams, Kelmendi, Brake, Gruner, Badour and Pittenger2018; Raposo-Lima & Morgado, Reference Raposo-Lima and Morgado2020), and therefore, any gender that has suffered more stress during the pandemic, may face greater challenges regarding OCD. Unlike the students (under 18 years old) and hospital staff in which the female gender probably suffered more stress, no gender seems to be more stressed among university students. A study by Chu et al investigated the potential impact of online learning during the pandemic on the mental health status of university students by assessing the differences in psychological distress and student life stress. They reported that gender did not affect the psychological distress nor the subdomains of student life stress and overall life stress (Chu & Li, Reference Chu and Li2022). Therefore, when the two genders did not differ significantly in terms of stress among university students, perhaps, for this reason, gender did not emerge as a risk factor for OCD in this sample group.
The cases that were raised only examine a number of possible hypotheses and there are definitely several factors that have affected these relationships and results, which can be the subject of future studies.
Articles can be reviewed based on another category. If we divide the articles into three sections, so that the first section (nine articles) refers to articles that consider the female gender as a risk factor for OCD (Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020; Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El J uan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020; Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020; Othman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021; Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021), the second section (11 articles) refers to articles that did not consider gender as a risk factor at all (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021; Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021; Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), and the third section (4 articles) including the articles that considered male gender as a risk factor (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021), we can make the following comparisons (needs to be mentioned that there are two articles in the third section that in a number of cases have stated that neither male nor female gender was risk factors, but because in a number of items male gender was expressed as a risk factor, we brought in this section and in previous sections of the discussion, we discussed these articles in detail (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020):
In the first section, four studies were established in the Middle East (Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020; Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021), two in Northern America (Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021), two in Europe (Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020; Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021), and one in Eastern Asia (China) (Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020). Although these studies were established in four different continents, the fact that nearly half (four articles) of these studies were established in the middle east, cannot be ignored, and it may negatively affect the generality of the results of this section. Also, five studies in the second section were established in Europe, which is a remarkably high percentage (50.0%) for a specific region (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021; Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021) (Fig. 6).

Fig. 6 Geographical distribution of studies based on their results (whether gender is a risk factor and if so which gender). *A study from all over the world stated that OCD was gender-independent during the COVID-19 pandemic; however, the purpose of this chart is to compare different geographical areas based on the obtained results, so the mentioned study is not included in this figure.
The most popular methods used to assess the status of OCD are the Yale-Brown obsessive-compulsive scale (Y-BOCS) (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El J i et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Othman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021) and the OCI-R (Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021; Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021), each of which was used by seven articles. Also, one of the studies in the first section did not use any known validated measurement tool for assessing OCD status (McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021).
Unlike the first section, in which the studies mainly used the Y-BOCS to determine the state of OCD (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El J uan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020; Othman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021), the studies in the second (Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021; Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021) and third sections (AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021) mainly used obsessive-compulsive inventory-revised (OCI-R). Noteworthy that none of the articles in the first section used OCI-R.
Considering that studies mainly used two different instruments, the difference in the methods for examining OCD may have acted as a risk bias and caused imprecise in the reported results. A study by Sulkowski et al compared the clinician ratings on the Y-BOCS-SC for 112 OCD patients with their self-report ratings on the OCI-R. They reported good internal consistency reliabilities (alphas) for the six OCI-R symptom scales. In the Y-BOCS-SC, three of five scales had good reliabilities (alphas > .80); however, alphas for two other scales (symmetry/ordering and sexual/religious symptom scales) were inadequate. The total scores of the two instruments were highly correlated with their corresponding ‘checking’ scales, but no individual symptom scale was identified as an indicator of the overall presence of OCD symptoms. Comparing the two OCD measurement instruments, scales assessing symmetry/ordering, washing/contamination, and hoarding correlated well. However, regarding the other scales, lower correlations were monitored which indicates differences in symptom coverage by the two instruments. In addition, they compared Y-BOCS-SC and OCI-R scores to OCD symptom severity measures and self-report measures of depression (BDI-II) and anxiety (STAI-T). Most of the Y-BOCS-SC and OCI-R symptom scales had low correlations with the BDI-II and STAI-T; however, obsessing scale of OCI-R was well correlated with the STAI-T. Unfortunately, the comparison of these two methods and their correlation has been neglected and further studies are needed to provide a better view (Sulkowski et al., Reference Sulkowski, Storch, Geffken, Ricketts, Murphy and Goodman2008).
In total, 10 studies reported that they used the Chi-square test to assess the correlation between demographic factors and OCD symptom severity (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021). In general, this test was the most popular test used by studies to assess the mentioned correlation. Especially in the studies related to the second (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021) and third sections (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021). One of the studies in the first section did not clarify what tool they did use to assess the mentioned correlation (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020).
Regarding the study population, the second and third sections have the most credibility in this area, because half of the studies conducted in these sections selected their study population from the general population (AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021). In the second section, out of 10, five studies selected their sample from the general population (Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021; Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021), and in the third section, two (AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021) out of four. The first section has a weaker condition in this area so that out of nine studies, only three studies selected their sample from the general population (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021), which is one of the weaknesses of this section. Articles that did not select their sample from the general population, naturally, used a more limited group. Thus, reduces the generalizability of these studies. Also, in some studies, the included population was purely hospital staff (Doctors and Nurses) (Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020), and Physicians (Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021) which according to several studies they may be at more risk than the general population and may have affected the results and acted as a risk bias (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Lamiani et al., Reference Lamiani, Borghi, Poli, Razzini, Colosio and Vegni2021).
In several studies, the recruited population was larger than the calculated population, thus increasing the reliability of these studies (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021). Also, in a number of studies, the recruited population was proportional to the calculated population (Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021), and a number of studies did not provide information about the sample size calculation.
Three studies indicated that they used the snowball method to recruit their needed population and therefore it was not possible for them to determine how many subjects received the questionnaire and refused to answer them (Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021).
In nearly all studies, the number of female participants was more than males, and this inequality was significant in 17 articles (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020; Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020; Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021; Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021; Moreira et al., Reference Silva Moreira, Ferreira, Couto, Machado-Sousa, Fernandez, Raposo-Lima, Sousa, Pico-Perez and Morgado2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021) including three articles that considered male gender as a risk factor (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021). All four studies in the third section had more female participants than males (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021). This inequality may have acted as a risk bias and needs to be considered. However, in two studies, the rate of male participants was higher (Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020; Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021) and in one of them which considered female gender as a risk factor, the difference was remarkable with nearly two-thirds of the participants being male (Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020).
The smallest size of the study population belonged to a study in the second section with 30 people participating (which reduces the validity of the study) (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020), and the biggest one belonged to a cohort study in the third section with more than 13 000 people participating in its first survey (Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020). It is worth mentioning that all four studies in the third section were among the studies with the most participants (with a participation rate of more than 2000), which adds to the credibility of this section (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021). The study population range of studies in the first section varies from 150 (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020) to 2182 (Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020), in the second section 30 (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020) to 2900 (Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021), and in the third section 2117 (Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021) to 13 478 (in one of the study’s surveys) (Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020).
The age range of study participants varies and should be considered. In two studies belonging to the first section, the age range of the participants was generally under 18 years old (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021), and in six cases, it was generally above 18 years old (Abuhmaidan & Al-Majali, Reference Abuhmaidan and Al-Majali2020; Juan et al., Reference Juan, Yuanyuan, Qiuxiang, Cong, Xiaofeng, Yundong, Jing, Peifeng, Yan, Xiaojiao and Yujie2020; Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020; Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021). In two of our articles, they did not mention the age range of participants, but the mean age was 31.32 ± 11.11 (El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021) and 39.66 years (Højgaard et al., Reference Højgaard, Duholm, Nissen, Jensen and Thomsen2021), respectively. About the age range of study participants in the second section, most studies in this section have studied the young population so that either the mean age is less than 30 or the main population of the study is under 30 years (Munk et al., Reference Munk, Schmidt, Alexander, Henkel and Hennig2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Aftab et al., Reference Aftab, Abadi, Nahar, Ahmed, Mahmood, Madaan and Ahmad2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021; Taher et al., Reference Taher, Al-Fadhul, Abutiheen, Ghazi and Abood2021). One of the studies in this section did not mention the age range or mean age of the participants, but according to the information given about the educational status of the participants, it seems that the subjects were over 18 years old (Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021). And finally, all four studies in the third section were performed generally among individuals with more than 18 years. By noting this fact, of course, some factors that are related to age are also different. For example, given that the participants in several studies were under the age of 18 (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021), the marriage and employment rates are very low. Moreover, marital status, the rate of employment, and history of mental illnesses may also have played a role and affected the obtained results and should be checked to see if they are risk bias.
The highest score in our qualitative analysis of cross-sectional studies (Newcastle−Ottawa quality assessment scale) was 9 points which were awarded to one of the articles in the second section (Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021). Proper comparability is one of the strengths of this study and it was the only one that provided information on non-respondents. Also, several studies in this analysis have received 8 points (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; Alateeq et al., Reference Alateeq, Almughera, Almughera, Alfedeah, Nasser and Alaraj2021; AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021; El Z hang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020; Zheng et al., Reference Zheng, Xiao, Xie, Wang and Wang2020; Othman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021), which can be attributed to good comparability.
The lowest score in this evaluation was 5 points, due to the weakness in the selection of the study and is placed in the first section. This study also had the lowest number of participants with 30 people among all studies (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020). There were also three cohort studies, all of which scored 6 points in our qualitative analysis. It should be noted that there was only one cohort article in each section (Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021). The highest score obtained by cross-sectional studies in the first and second sections was 8 (Ahmed et al., Reference Ahmed, Ramadan, Refay and Khashbah2021; El O thman et al., Reference El Othman, Touma, El Othman, Haddad, Hallit, Obeid, Salameh and Hallit2021; Fontenelle et al., Reference Fontenelle, Albertella, Brierley, Thompson, Destrée, Chamberlain and Yücel2021), and 9 (Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021) points respectively. And the lowest scores were 5 (Darvishi et al., Reference Darvishi, Golestan, Demehri and Jamalnia2020), and 6 (Davide et al., Reference Davide, Andrea, Martina, Andrea, Davide and Mario2020; Dehkordi et al., Reference Dehkordi, Gholamzad, Myrfendereski, Dehkordi and Ghaderi2021; McKune et al., Reference Mckune, Acosta, Diaz, Brittain, Beaulieu, Maurelli and Nelson2021) points, respectively. Noteworthy that all four cross-sectional articles in the third section, scored well on the Newcastle−Ottawa scale. Two cross-sectional studies received 7 points (Abba-Aji et al., Reference Abba-Aji, Li, Hrabok, Shalaby, Gusnowski, Vuong, Surood, Nkire, Li, Greenshaw and Agyapong2020; Samuels et al., Reference Samuels, Holingue, Nestadt, Bienvenu, Phan and Nestadt2021) and the other scored 8 points (AlHusseini et al., Reference AlHusseini, Sajid, Altayeb, Alyousof, Alsheikh, Alqahtani and Alsomali2021). The results of the qualitative analysis were similar in the three sections and there was no significant difference.
As mentioned, 21 of the 24 articles included in the study used a cross-sectional method to conduct their study, which is not a very appropriate method due to its nature. In addition, three studies used the cohort study method to perform their study, which is a more appropriate method for examining the relationship between gender and OCD during the COVID-19 pandemic, and therefore these studies are more valid (Ji et al., Reference Ji, Wei, Yue, Li, Shi, Ma, He, Zhou, Zhao, Lou, Cheng, Yang and Hu2020; Mazza et al., Reference Mazza, Lorenzo, Conte, Poletti, Vai, Bollettini, Melloni, E.M., Furlan, Ciceri, Rovere-Querini and Benedetti2020; Meda et al., Reference Meda, Pardini, Slongo, Bodini, Zordan, Rigobello, Visioli and Novara2021). However, since these three studies were divided into three sections, and each had only one cohort study, and all these studies also scored the same in our qualitative analysis (6 points), so this issue cannot be used to prioritise one section over another.
It is worth mentioning that none of our cross-sectional studies have compared the respondents and non-respondents properly and therefore all but one (Ferreira et al., Reference Ferreira, Sousa, Moreira, Sousa, Picó-Pérez and Morgado2021) missed a point in the selection part of the Newcastle−Ottawa quality assessment scale. Also, most of the studies used the self-report method to present their outcomes and consequently they lost another point in this mentioned assessment.
Limitation
There were several limitations in this review including the limitation of studies, variation in data collection, and methods of assessing the correlation between demographical variables and OCD symptom severity and studied population.
As mentioned in the discussion, in pre-pandemic articles, the symptoms of OCD were widely compared between men and women, but in the current study, our references never accurately compared the symptoms of men and women, and only had a general comparison. Therefore, it was not possible for us to accurately compare the symptoms of obsessions and compulsions between men and women during the COVID-19 pandemic.
Also, the databases used in this systematic review were limited to three databases: PubMed, Scopus, and Web of Science. To reduce the potential risk of bias due to the limited number of databases, we reviewed references of our included articles to retrieve potential missing studies. But due to the novelty of the subject, the number of duplicate articles is high, and we could not find new studies through this way. However, we recommend future studies consider more databases for their research after conducting studies that specifically examine the signs and symptoms of OCD in men and women. It also needs to be mentioned that the search was conducted only on articles in English and some studies online were demonstrated.
Also, regarding the meta-analysis conducted in this study, we encountered serious limitations. The primary goal of this study was to conduct a meta-analysis for each of the classifications based on the objectives of the studies (prevalence), geographical regions, and the sample groups of the studies. However, due to the limitations mentioned below, conducting the meta-analysis was limited only to studies that investigated the prevalence of OCD during the COVID-19 pandemic.
The 24 studies that were reviewed in this study had many heterogeneities, so it was impossible to perform a general meta-analysis. In order to reduce heterogeneity, studies were divided into several groups. The first division was based on the objectives of the studies, where the studies that investigated the prevalence of OCD were placed in one group. The second division was based on geographical regions and the third division was based on the study sample group. One of the limitations that we encountered in the second and third classifications was the different objectives of the studies conducted in each of the geographical regions or sample groups. For example, the studies that were conducted in the Middle East or Europe or among the general population dealt with different aspects of OCD, and it was not possible to design a specific research question. Also, studies used different and various methods to assess OCD status, and therefore it was not possible to unify their methods. Also, one of the most important limitations that we encountered in all the classifications was that none of the studies were specifically designed with the aim of examining the differences between the two genders in relation to OCD during the COVID-19 pandemic. This point greatly limited the possibility of expanding the meta-analysis. For example, in the section related to the prevalence of OCD, it was not possible to examine any side factors, because the studies never differentiated between the two genders in presenting their information, and for example, when presenting information related to the occupational status of their sample, they limited themselves to providing information on the main sample group.
Another serious limitation was the small number of studies after dividing them into different subgroups. For example, there were only two studies in the subgroup related to under 18 years old students, and performing a meta-analysis under these conditions would damage its validity. Therefore, the meta-analysis was limited to examining different aspects of the prevalence of OCD during the COVID-19 pandemic.
Regarding the meta-analysis conducted to investigate the prevalence of OCD, there were limitations that caused the heterogeneity of the analysis to be 99.07%. The first limitation was the small number of studies that investigated this relationship. The prevalence of OCD during the COVID-19 pandemic was examined by seven studies, and only five of them differentiated the prevalence of OCD between the two genders. The next limitation was the difference in the method used to investigate OCD status, which studies used different methods (5 methods in 7 studies). Another limitation was the difference in the sample groups of the studies, for example, the study group was selected from students (under 18 years old), university students, and the general population. Future studies can help the progress of this field by considering and overcoming the limitations raised in this systematic review.
Conclusion
This systematic review, as the first one to investigate the gender differences in OCD during the Covid-19 pandemic, found that seemingly the female gender has been more vulnerable to OCD during the pandemic. The meta-analysis results revealed a 41.2% overall prevalence of OCD during the COVID-19 pandemic and 47.1% and 39.1% OCD prevalence for female and male genders, respectively. Although the prevalence of OCD was higher in females compared to males, this difference was not statistically significant. In the students (under 18 years old), and hospital staff, the female gender may have acted as a risk factor. However, in the following demographic subgroups, gender was not identified as a risk factor: medical students, university students, and possibly the general population. In none of the categories, the male gender was clearly identified as a risk factor regarding OCD. When it comes to geographical regions, studies conducted in the Middle East show a more significant role for the female gender regarding OCD. However, in European studies, the relationship was more gender independent. Generally, studies considered OCD to be gender-dependent, overcome those declared gender-independent in this systematic review. Further studies must be performed considering the risk biases mentioned in this study especially those that compare the symptoms of OCD in men and women.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/neu.2023.15
Acknowledgements
We want to sympathise with the victims of the recent earthquake that occurred in the city of Khoy (Xoy) in the West Azerbaijan province of Iran on 28 January 2023. We also want to express our sympathies to the victims of the massive earthquake that occurred in Türkiye and Syria affecting more than 20 million people on 6 February 2023. We dedicate our work to all those who suffered from these earthquakes, and our hearts remain with the victims of these tragic incidents. YOU ARE NOT ALONE!
We also want to draw attention to Lake Urmia located in north-western Iran, West and East Azerbaijan provinces, which suffers from severe environmental conditions and is on the verge of drying up, thus endangering the lives of tens of millions of people living in the area, and affecting at least five countries (Iran, Iraq, Azerbaijan, Armenia, and Türkiye). We need all the help we can get to prevent a large-scale environmental disaster.
Author contributions
EJ, study conception, data gathering, article writing (abstract, method, results, discussion, limitation, conclusion, table 1,2,3,4,5,6, figure 1,2,3,4), and article editing.
AA, data gathering, article writing (introduction, results, table 2,3,4).
MR, data gathering, article writing (method), article editing.
RB, data gathering, article writing, meta-analysis.
Financial support
None.
Conflict of interest
None.
Competing interests
The authors declare that they have no competing interests.
Availability of data and material
All data used for this study are gathered and illustrated in the file.















