People with a mental disorder face markedly higher mortality rates compared with the general population,Reference Walker, McGee and Druss1 resulting in an average reduced life expectancy of 7.1 years for women and 10.1 years for men.Reference Plana-Ripoll, Pedersen, Agerbo, Holtz, Erlangsen and Canudas-Romo2 People with a mental disorder are also considerably more likely to have diminished social connections,Reference Richter and Hoffmann3 which has likewise been established as a key determinant of mortality.Reference Wang, Gao, Han, Yu, Long and Jiang4,Reference Holt-Lunstad, Smith and Layton5 Additionally, a reciprocal relation has been documented, where people with a mental disorder are prone to become more socially disconnected,Reference Wang, Chung, Wang, Yu and Kenardy6 while people with diminished social connections are also more likely to develop a mental disorder.Reference Mann, Wang, Pearce, Ma, Schlief and Lloyd-Evans7 Previous studies have shown that people with both a mental disorder and diminished social connections are at increased risk of adverse outcomes in terms of symptom severity, recovery and social functioning.Reference Wang, Mann, Lloyd-Evans, Ma and Johnson8 Although some prior studies have also investigated diminished social connections as a determinant of mortality in the context of mental disorders, these findings have been inconclusive and inconsistent.Reference Otsuka, Sugawara, Matsuyama and Tsuji9–Reference Finlay, Oliva, Timko, Moos and Cronkite15 Understanding the interplay of these risk factors could be of importance to identify groups at high risk of premature death, which can inform targeted prevention efforts and help to shed light on the underlying causal factors in the observed life expectancy gap.
The majority of prior studies have focused on individuals with depression and are limited by small study populations (<4000 individuals)Reference Otsuka, Sugawara, Matsuyama and Tsuji9–Reference Finlay, Oliva, Timko, Moos and Cronkite15 (for a full overview of previous studies see Supplementary T1 available at https://doi.org/10.1192/bjp.2024.68). To further investigate interaction between mental disorders and diminished social connections on mortality, comprehensive studies based on larger samples are needed. In addition, several studies have reported results according to sex,Reference Otsuka, Sugawara, Matsuyama and Tsuji9,Reference Holwerda, van Tilburg, Deeg, Schutter, Van and Dekker12 ageReference Otsuka, Sugawara, Matsuyama and Tsuji9 or characteristics of the mental disorder.Reference Holwerda, van Tilburg, Deeg, Schutter, Van and Dekker12 Exploration of results for subgroups is relevant to clarify whether specific risk factors are of greater importance in certain demographic or clinical groups. Therefore, we aimed to examine whether mental disorders interact with three distinct aspects of diminished social connections (loneliness, social isolation and low social support) on mortality, while taking into account sex, age and a range of characteristics of the mental disorder.
Method
Study design and population
We designed a cohort study of participants in the Danish National Health Survey, linking self-reported information on social connections with national register data on mental disorders and mortality. The Danish National Health Survey is a population-based survey conducted every fourth year.Reference Christensen, Lau, Kristensen, Johnsen, Wingstrand and Friis16 The survey is based on five stratified random samples from the Danish administrative regions and one national random sample, drawn from individuals aged ≥16 years in the Danish Civil Registration System.Reference Pedersen17 Based on the availability of self-reported data on social connections, we included 162 604 survey participants from four regional samples in 2017 and one regional sample in 2013. Survey invitations were sent via the regular postal service (2013, 2017) and a secure electronic mail service (2017), and it was possible to participate either by paper or online (i.e. mixed-mode approach) in both years.Reference Christensen, Lau, Kristensen, Johnsen, Wingstrand and Friis16 The overall response rate was 57.5%. To account for non-response and selection probabilities, we applied inverse probability weights constructed by Statistics Denmark based on information from the national registers using a model-based calibration approach.Reference Christensen, Lau, Kristensen, Johnsen, Wingstrand and Friis16 These weights have been shown to account well for the underrepresentation of individuals with a mental disorder in the Danish National Health Survey.Reference Momen, Lasgaard, Weye, Edwards, McGrath and Plana-Ripoll18 Owing to the population-based sample, 3426 (2.1%) of the responses came from individuals who participated in both 2013 and 2017. To maintain the sample used for weighting, both responses from repeated participants were included with time-specific exposure and covariate information. The survey data were linked with register data using unique personal identification numbers from the Danish Civil Registration System.Reference Pedersen17 Only 107 individuals (0.07%) were excluded owing to no register linkage at the time of the survey. The remaining individuals (N = 162 497) were followed from the date of survey participation until death, emigration or end of data availability (31 December 2021), whichever came first. A flowchart illustrating the definition of the cohort is presented in Supplementary F1.
The study was registered with the Danish Data Protection Agency at Aarhus University (file no. 2016-051-000001-2587) and approved by Statistics Denmark and the Danish Health Data Authority. All survey participants were informed that participation was voluntary and that their survey data could be linked to registers for research purposes. The respondents’ full or partial completion of the survey constituted implied consent. No further ethical approval is required for registry-based research in Denmark. Data were accessed and analysed in a pseudo-anonymous form on secure servers located at Statistics Denmark.
Measures
Social connections
Loneliness, social isolation and low social support were assessed in the Danish National Health Survey. Loneliness is commonly defined as an undesirable emotional state resulting from a perceived lack of social contactReference Peplau, Perlman, Peplau and Perlman19 and was assessed with the Danish version of the Three-Item Loneliness Scale.Reference Hughes, Waite, Hawkley and Cacioppo20,Reference Lasgaard21 In 2013, one of the three items was phrased slightly differently, but the scale has demonstrated good internal consistency at both time points.Reference Laustsen, Christiansen, Maindal, Plana-Ripoll and Lasgaard22 We classified individuals scoring 7 or higher as experiencing loneliness, corresponding to the most conservative dichotomisation of severe loneliness applied in the literature.Reference Nielsen, Friderichsen and Rayce23 Social isolation refers to the objective state of having limited social contactReference de Gierveld, van Tilburg, Dykstra, Vangelisti and Perlman24 and was assessed through quantification of different areas of social contact inspired by the Berkman-Syme Social Network Index.Reference Berkman and Syme25 Specifically, we measured social isolation using an index based on four indicators of social contact: (a) living alone (yes = 1, no = 0), (b) not employed and not enrolled in education (yes = 1, no = 0), (c) less than monthly contact with friends (yes = 1, no = 0) and (d) less than monthly contact with family outside of the household (yes = 1, no = 0). We classified individuals with a score of 3 or 4 as socially isolated. Social support comprises multiple dimensions; we focused specifically on perceived emotional support.Reference Sheldon, Lynn and Gottlieb Benjamin26 Inspired by the MOS Social Support Instrument,Reference Sherbourne and Stewart27 social support was assessed with the single-item ‘Do you have someone to talk to if you have problems or need for support?’, and the four response options ‘Yes, always’, ‘Yes, mostly’, ‘Yes, sometimes’ and ‘No, never or almost never’. The two last-mentioned response options were classified as low social support.
Mental disorders
Information on mental disorders in the 18 years preceding survey participation was obtained from the Danish Psychiatric Central Research Register, which since 1 January 1995 contains diagnostic data on emergency room contacts, out-patient visits and admissions to psychiatric hospital services in Denmark.Reference Mors, Perto and Mortensen28 Diagnoses were based on the International Classification of Diseases, 10th revision (ICD-10). We excluded organic disorders (ICD-10: F00–F09) and intellectual disabilities (ICD-10: F70–F79) owing to concerns regarding response validity and response ratesReference Momen, Lasgaard, Weye, Edwards, McGrath and Plana-Ripoll18 but included all other psychiatric diagnoses (ICD-10: F10–69 and F80–99). We additionally included information on the diagnostic category of the initial diagnosis as specified in SA1, the primary type of contact with psychiatric hospital services (determined based on the greatest number of contacts as emergency room patient, in-patient and/or out-patient), the number of contacts with psychiatric hospital services and the time since the most recent contact with psychiatric hospital services.
Mortality
All-cause mortality was estimated using the date of death from the Danish Civil Registration System.Reference Pedersen17 Additionally, the cause of death was obtained from the Danish Register of Causes of Death and categorised in external causes (suicides, homicides and accidents) and natural causes (all other causes) with data available until 31 December 2020 (see Supplementary A1).
Covariates
Demographic characteristics included age, sex (administrative legal sex classified as female or male in the registers; information on gender was not available), country of birth (Denmark and Greenland versus abroad) and linkage to legal parents, all obtained from the Danish Civil Registration System. Somatic morbidity was assessed with the Nordic Multimorbidity Index,Reference Kristensen, Lund, Jensen, Broe, Rotbain and Damkier29 using data from the Danish National Patient Register and the Danish National Prescription Registry. The highest level of completed education was obtained from the Population Education Register and classified into three groups. Annual disposable equivalised household income and equivalised household wealth were obtained from the Income Statistics Register and adjusted for inflation. For individuals aged <30 years, their parents’ highest educational level and an average of their parents’ values for income and wealth were used as proxies. Since the survey data could not address the onset of diminished social connections, we assessed somatic morbidity, educational level, income and wealth before the date of the first registered diagnosis of a mental disorder, hereafter referred to as the index date. To ensure consistency, we replicated this adjustment procedure among individuals without a mental disorder via the assignment of pseudo-index dates in age- and sex-specific groups. Details can be found in Supplementary A1.
Statistical analysis
We performed multiple imputation of missing survey and register data to avoid introducing selection bias through the exclusion of 25 698 individuals (15.8% of the cohort) with partly missing data (Supplementary A2).
All estimates are calculated with inverse probability weights and multiple imputed data. For each aspect of diminished social connections, a Poisson regression model with linearised variance estimation and 95% CIs was applied to estimate the independent and joint association with mortality rates for mental disorders and diminished social connections. We applied two adjustment models: in model 1, we adjusted for age, sex and year of survey participation, and in model 2, we further adjusted for country of birth, somatic morbidity, educational level, income and wealth (Supplementary A3).
The data were analysed based on the concept of additive interaction since this is considered relevant for healthcare prioritisation.Reference Lash, VanderWeele, Haneuse and Rothman30 We estimated the interaction contrast as a measure of the mortality rate beyond or below that expected based on additivity of independent associations with mortality.Reference Lash, VanderWeele, Haneuse and Rothman30 To ease comparison of interaction contrasts for the different aspects of diminished social connections, we applied marginal standardisation to individuals with a mental disorder and at least one of loneliness, social isolation and low social support. If excess mortality was present (i.e. synergistic interactions), we additionally estimated the attributable proportion of joint effects as a measure of the proportion of the joint association with the mortality rate that can be attributed to an interaction.Reference Lash, VanderWeele, Haneuse and Rothman30 Details can be found in Supplementary A3.
These analyses were repeated for specific subgroups defined by sex (women, men), age (16–55, 55–75 and >75 years), diagnostic category of the initial diagnosis, primary type of contact with psychiatric hospital services (in-patient, out-patient, emergency room patient), number of contacts with psychiatric hospital services (1–2, >2) and time since the last contact with psychiatric hospital services (<5, 5–18 years). Because of a low number of cases for some types of mental disorders, we computed estimates for only three diagnostic categories (substance use disorders [ICD-10: F10–9], mood disorders [ICD-10: F30–9] and anxiety or neurotic disorders [ICD-10: F40–8]).
As a sensitivity analysis, we investigated whether similar results were obtained using alternative operationalisations of mental disorders (self-reported information, redeemed prescriptions of psychopharmaceuticals and consultation with a private practise psychiatrist [Supplementary A1]). To examine the dichotomisation of loneliness, social isolation and low social support, we additionally estimated the association with mortality rates for specific scores/responses. Furthermore, we repeated the main analysis with alternative modelling assumptions (cluster-robust standard errors to account for correlation between observations from repeated participants, added covariate adjustment and a complete case analysis).
Statistical analyses were conducted in Stata version 17.0 on a Windows Server 19 operating system using the svy and mi suite of commands. A preregistered analysis plan and the code used for data management and statistical analysis are available at Open Science Framework (https://osf.io/aqx4s).
Results
In the total sample (N = 162 497), the mean age at survey participation was 48.3 years (s.d. 19.1), 87 627 (50.6%) were women, 10 347 (7.7%) had a pre-existing diagnosis of a mental disorder from in-patient or out-patient psychiatric hospital services, and the number of individuals classified as lonely, socially isolated and with low social support, respectively, was 9829 (7.6%), 4720 (3.5%) and 21 370 (14.9%). Descriptive characteristics stratified by mental disorders and social connections are presented in Table 1. Among individuals with a mental disorder, 3869 (40.6%) experienced loneliness, social isolation and/or low social support, whereas this was the case for 24 414 (18.3%) of the individuals without a mental disorder. Individuals with a mental disorder were also more prone to experiencing co-occurring loneliness, social isolation and low social support compared with individuals without a mental disorder (Supplementary F2).
Table 1 Descriptive statistics stratified by mental disorders and social connections
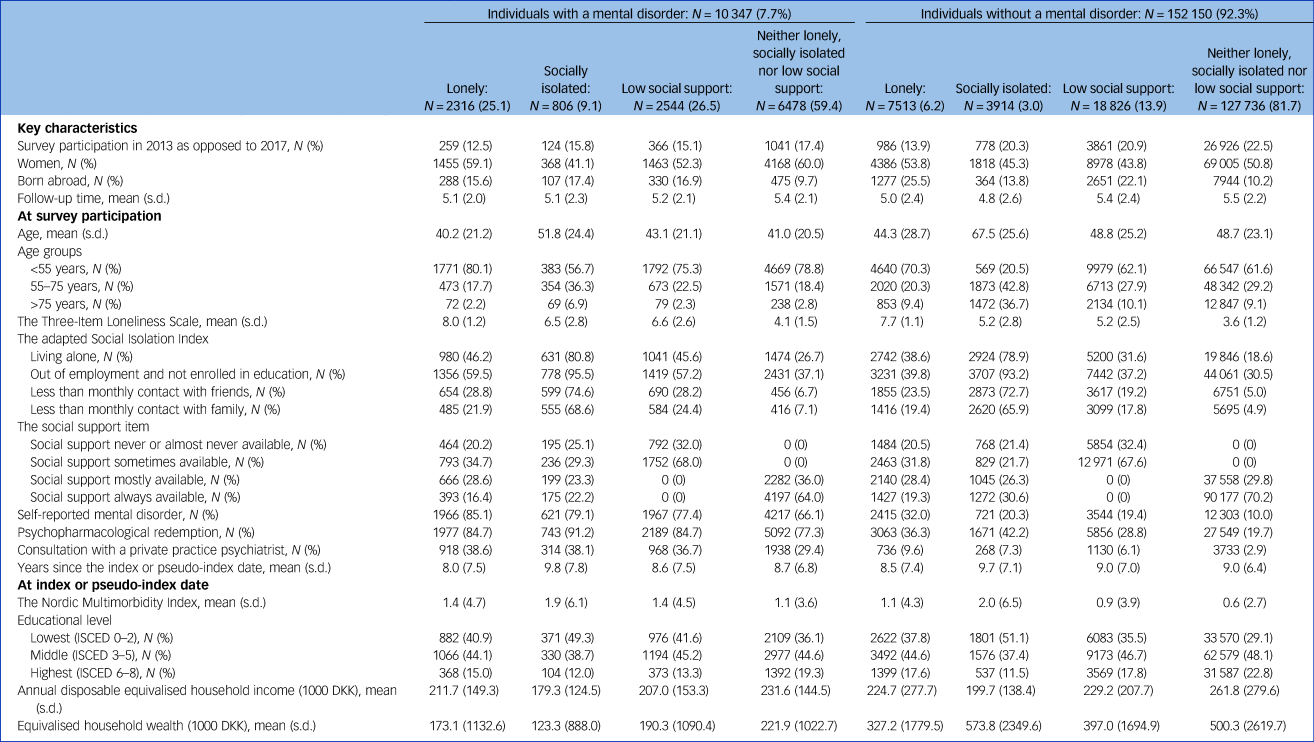
Missing data were imputed using multiple imputation by chained equations. Absolute numbers are unweighted, whereas percentages, means, and s.d.s are weighted based on register data to represent the population of the included regions in 2013 and 2017.
The cohort was followed for a mean period of 5.5 years with a total of 886 614 person-years at risk. During follow-up, 9047 deaths occurred. Table 2 displays the estimated associations with mortality rates for mental disorders and diminished social connections. After all adjustments, the joint associations of mental disorders and loneliness, social isolation and low social support, respectively, with mortality rates were 2.51 (95% CI: 1.99–3.03), 2.53 (95% CI: 2.00–3.06) and 2.23 (95% CI: 1.79–2.67). An interaction between mental disorders and loneliness, social isolation and low social support, respectively, accounted for 19% (95% CI: −14 to 52%), 16% (95% CI: −18 to 49%) and 34% (95% CI: 4–64%) of the excess mortality in these groups.
Table 2 Independent and joint associations of mental disorders and social connections with mortality
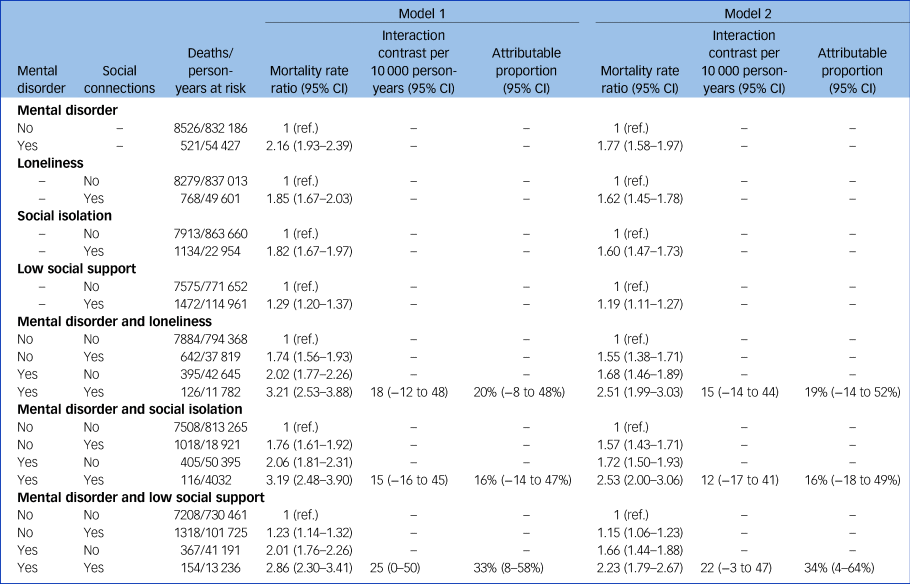
Missing data were imputed using multiple imputation by chained equations, and the results are weighted based on register data to represent the population of the included regions in 2013 and 2017. Interaction contrasts are calculated using marginal standardisation to individuals with at least one of loneliness, social isolation and low social support. Model 1 is adjusted for age, sex and year of survey participation, and model 2 is further adjusted for country of birth, somatic morbidity, educational level, income and wealth.
As shown in Fig. 1, synergistic interactions were found for men, but not for women, in fully adjusted subgroup analyses. Specifically, among men, an interaction between mental disorders and loneliness, social isolation and low social support, respectively, accounted for 47% (95% CI: 21–74%), 24% (95% CI: −15 to 63%) and 61% (95% CI: 35–86%) of the excess mortality in these groups. In other words, 47, 24 and 61% of the excess mortality among men with both a mental disorder and loneliness, social isolation and low social support, respectively, could not be explained by these factors independently. This corresponded to 61 (95% CI: 6–115), 24 (95% CI: −22 to 69) and 59 (95% CI: 16–101) deaths per 10 000 person-years among men with both a mental disorder and diminished social connections. Among women, no excess mortality could be attributed to interaction. Concerning the other subgroup analyses, mixed results were found for the different aspects of diminished social connections according to age, diagnostic category (substance use disorders, mood disorders and anxiety or neurotic disorders), primary type of contact, number of contacts and time since the most recent contact with psychiatric hospital services (Supplementary F3). As a result of sample size limitations, no formal subgroup analysis was done for the cause of death; however, 2508 (63.6%) and 101 (2.3%) deaths could be attributed to respectively natural and external causes among women, whereas this was the case for 3239 (63.8%) and 150 (3.6%) deaths among men.
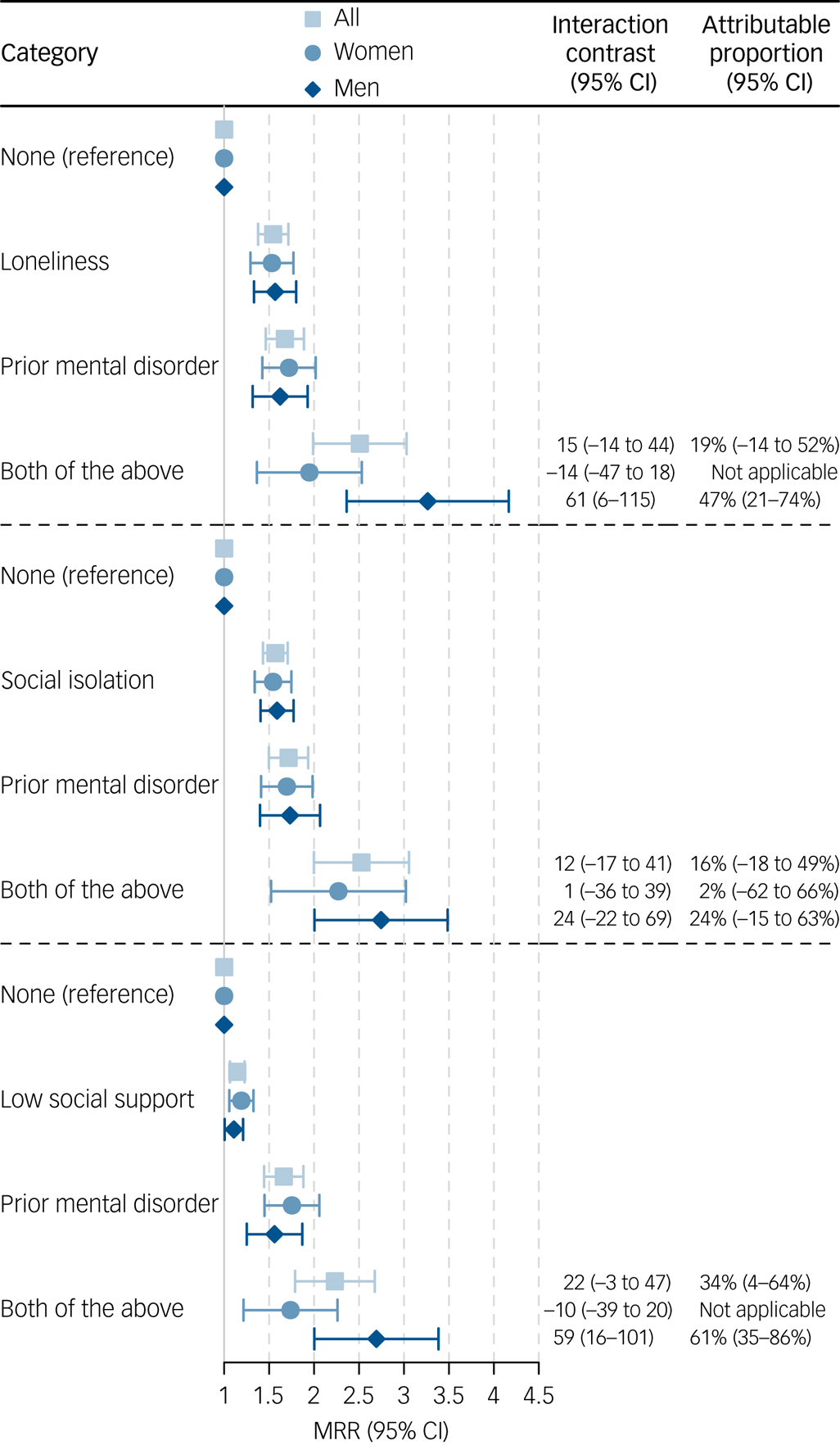
Fig. 1 Independent and joint associations of mental disorders and social connections with mortality among women and men. MRR: mortality rate ratio. Missing data were imputed using multiple imputation by chained equations, and the results are weighted based on register data to represent the population of the included regions in 2013 and 2017. The attributable proportion was calculated if a synergistic interaction was found. Interaction contrasts are calculated using marginal standardisation to individuals with at least one of loneliness, social isolation and low social support. The models are adjusted for age, sex year of survey participation, country of birth, somatic morbidity, educational level, income and wealth (model 2). Estimates can be found in ST2.
The results were robust to the application of alternative operationalisations of mental disorders, as we found varying associations with mortality but comparable attributable proportions for interaction (Supplementary F4). Additionally, we found a dose-response-like association with mortality for specific scores of loneliness and social isolation and a threshold-like association with mortality for specific responses on the social support item (Supplementary F5). Similar results for the interactions were also obtained in an analysis with cluster-robust standard errors, after additional covariate adjustment and in a complete case analysis (Supplementary F6).
Discussion
In this analysis of data from the Danish National Health Survey linked with national registers, we found a substantially higher mortality rate than expected among men with both a mental disorder and diminished social connections, whereas among women no excess mortality could be attributed to an interaction between them. In contrast, no clear trend was found for an interaction between mental disorders and diminished social connections according to age and a range of characteristics of the mental disorder. Importantly, our results were not attributable to the operationalisation of mental disorders, the scale thresholds used or the adjustment procedure, as similar results were found in sensitivity analyses.
Compared with a previous study of mental disorders applying Danish register data,Reference Plana-Ripoll, Pedersen, Agerbo, Holtz, Erlangsen and Canudas-Romo2 we obtained a slightly lower estimate of the association between mental disorders and mortality. This difference might be explained by our exclusion of organic mental disorders and intellectual disabilities, since the association with mortality for these diagnostic categories is stronger than that of all mental disorders combined.Reference Plana-Ripoll, Pedersen, Agerbo, Holtz, Erlangsen and Canudas-Romo2 When compared with previous reviews on loneliness, social isolation and low social support,Reference Wang, Gao, Han, Yu, Long and Jiang4,Reference Holt-Lunstad, Smith and Layton5 we found a considerably stronger association with mortality for loneliness and social isolation, but a similar association with mortality for low social support. These discrepancies could be as a result of our application of relatively conservative thresholds for loneliness and social isolation which classified 7.6% of the cohort as lonely and 3.5% as socially isolated.
In the total sample, our findings indicated that some excess mortality was attributable to an interaction, which is in line with previous studies on lonelinessReference Stek, Vinkers, Gussekloo, Beekman, van der Mast and Westendorp11,Reference Holwerda, van Tilburg, Deeg, Schutter, Van and Dekker12 and low social support.Reference Otsuka, Sugawara, Matsuyama and Tsuji9 In contrast, a recent study did not find any association between loneliness and mortality among patients attending mental healthcare services, yet this study assessed loneliness using healthcare records rather than a validated measure.Reference Parmar, Ma, Attygalle, Mueller, Stubbs and Stewart13 A prior study on social isolation and depression likewise reported no significant interaction,Reference Fuhrer, Dufouil, Antonucci, Shipley, Helmer and Dartigues14 a finding which is in line with our subgroup analysis restricted to individuals with mood disorders. However, comparisons across studies are complicated by differences in the operationalisations of loneliness, social isolation and social support (see Supplementary T1).
In the subgroup analyses, we found that men, but not women, with both a mental disorder and diminished social connections have elevated mortality rates compared with what was expected. This finding is consistent with a previous study where a stronger association with all-cause mortality was found among men compared with women with both severe depression and loneliness.Reference Holwerda, van Tilburg, Deeg, Schutter, Van and Dekker12 However, another study found a similar association with death from suicide among men and women with symptoms of a mood or anxiety disorder and low social support.Reference Otsuka, Sugawara, Matsuyama and Tsuji9
Strengths and limitations
A key strength of our study is the availability of a large population-based sample with the imputation of partly missing data and no loss to follow-up. While programming constraints hindered the correction of standard errors to account for correlation between observations from repeated participants, a sensitivity analysis showed close to equal results after the estimation of cluster-robust standard errors in the total sample. Another strength of our study is the linkage of rich survey data with high-quality national register data. The study benefited from a validated measure of lonelinessReference Lasgaard21 and an index for social isolation which has its roots in the well-known Berkman–Syme Social Network Index.Reference Berkman and Syme25 Additionally, we used register-based data on hospital-diagnosed mental disorders to circumvent recall bias. The validity of hospital-diagnosed mental disorders has been confirmed for some diagnoses,Reference Mors, Perto and Mortensen28 although the reliability may vary depending on the specific hospital setting. Not least, the estimation of deviations from additive interaction allowed us to compare mortality rates across subgroups on the absolute scale which holds relevance for healthcare prioritisation.Reference Lash, VanderWeele, Haneuse and Rothman30
However, we are confined to the limitations of survey data, and with a response rate of 57.5%, selection biases could have weakened the representativeness of the cohort. However, the applied inverse probability weights have been shown to mitigate bias caused by differential selection based on mental disorder diagnoses.Reference Momen, Lasgaard, Weye, Edwards, McGrath and Plana-Ripoll18 Additionally, individuals with a fatal outcome shortly after the onset of a mental disorder will be considerably underrepresented in our study design (cf. Neyman bias), which may have led to an underestimation of the association between mental disorders and mortality. In contrast to the Berkman–Syme Social Network Index,Reference Berkman and Syme25 the applied social isolation index did not include associational activities and voluntary work, limiting the accuracy in identifying social isolation. However, no consensus exists on the operationalisation of social isolation.Reference Prohaska, Burholt, Burns, Golden, Hawkley and Lawlor31 Likewise, the applied measure of social support has not been validated and was limited to capturing perceived emotional support.Reference Sheldon, Lynn and Gottlieb Benjamin26 Furthermore, our analysis based on diagnoses from psychiatric hospital services did not capture individuals who sought treatment from general practitioners or private practice psychiatrists as they do not report diagnoses to the applied register, nor did it capture individuals who did not seek help. Thus, differences in help-seeking behaviour could have affected the results. Additionally, the registers do not provide information on remission, and individuals could have recovered since receiving a diagnosis of a mental disorder.
Implications
Importantly, our data enable us to infer neither causality nor the temporal order of mental disorders and diminished social connections. We have, however, addressed whether individuals with a mental disorder and diminished social connections in co-existence have an elevated mortality rate. Our results regarding sex differences raise several hypotheses. First, the results could be due to a greater prevalence or progression of disease with impact on mortality. This scenario could be the case if socially disconnected men with mental disorders are especially likely to take up a range of health behaviours that increase the risk or progression of disease. A second explanation would be a greater case fatality rate as a result of suboptimal treatment outcomes. This explanation could apply if socially disconnected men with mental disorders are less likely to recognise symptoms, adhere to treatment or have difficulties navigating the healthcare system to achieve optimal treatment. A third explanation could be a greater number of deaths because of external causes of death (e.g. suicides and accidents), given that social connections affect men's ability to cope with mental disorders. These hypotheses have, however, not been tested, and further studies are therefore needed to investigate specific causes of death and elucidate the potential behavioural, psychological or physiological mechanisms driving our findings.Reference Berkman, Glass, Brissette and Seeman32 Furthermore, health literacy, disease burden or co-occurrence of different aspects of social connectedness could also play a role as confounding factors. Irrespective of the underlying mechanisms, these findings suggest that men with a mental disorder and diminished social connections in co-existence constitute a vulnerable group. Thus, these sex differences could have direct implications for clinical practice when feasible to tailor services and interventions to address the needs of particularly vulnerable population groups. However, further studies are needed to confirm and explore these findings.
In conclusion, our findings suggest sex differences in the extent to which the strain of a mental disorder in combination with diminished social connections translates into increased all-cause mortality. The mortality rate among men, but not women, with a co-occurring mental disorder and diminished social connections was substantially elevated compared with what was expected. Awareness of elevated mortality rates among socially disconnected men with mental disorders could be of importance to qualify and guide prevention efforts in psychiatric services. Further studies are needed to investigate how our findings apply to specific causes of death and explore potential mechanisms behind these sex differences.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2024.68
Data availability
Data presented in this study were obtained from Danish registries and regions participating in the Danish National Health Survey. Owing to data protection rules, we are not allowed to share individual-level data. Other researchers who fulfil the requirements set by the data providers may gain access to the data through Statistics Denmark, the Danish Health Data Authority and/or the Danish regions (Central Denmark Region, North Denmark Region, Region Zealand and Capital Region of Denmark).
Author contributions
L.M.L., M.L., L.E., S.D.Ø., J.L.G., D.C. and O.P.-R. participated in designing the study and preregistered the protocol. L.L., M.L., M.S.G. and O.P.-R. contributed to acquisition of data for the work. With help from O.P.-R., L.E. and M.L., LM.L. conducted data curation and analysis. D.C. accessed and verified the data curation and analysis. All authors contributed to the interpretation of the results. L.M.L. wrote the first draft of the paper, which was subsequently revised for important intellectual content by the remaining authors. All authors contributed to the interpretation of the results and approved the final manuscript prior to submission.
Transparency declaration
L.M.L. and O.P.-R. had full access to the data and had the final responsibility for the decision to submit for publication. L.M.L. and O.P.-R. affirm that the manuscript is an honest, accurate and transparent account of the conducted study. A preregistered analysis plan is available at Open Science Framework (https://osf.io/aqx4s).
Analytic code availability
All statistical code from the main analysis is available at Open Science Framework (https://osf.io/aqx4s).
Funding
This work was supported by the Graduate School of Health at Aarhus University (PhD fellowship to L.M.L.), the American-Scandinavian Foundation (travel grant to L.M.L.), the William Demant Foundation (travel grant to L.M.L.) and the Lundbeck Foundation (Fellowship R345-2020-1588 to O.P.-R.). O.P.-R. also received funding from Independent Research Fund Denmark (grants 1030-00085B and 2066-00009B). S.D.Ø. also received funding from the Novo Nordisk Foundation (grant number: NNF20SA0062874), the Lundbeck Foundation (grant numbers: R358-2020-2341 and R344-2020-1073), the Danish Cancer Society (grant number: R283-A16461), the Central Denmark Region Fund for Strengthening of Health Science (grant number: 1-36-72-4-20), the Danish Agency for Digitization Investment Fund for New Technologies (grant number 2020-6720) and Independent Research Fund Denmark (grant numbers: 7016-00048B and 2096-00055A). The Central Denmark Region Health Survey was conducted and funded by the Central Denmark Region. The North Denmark Region Health Survey was conducted and funded by the North Denmark Region. The Danish Capital Region Health Survey was conducted and funded by the Capital Region. The Region Zealand Health Survey was conducted and funded by Region Zealand. The funding sources had no role in the design and conduct of the study; the collection, management, analysis and interpretation of the data; the preparation, review or approval of the manuscript; and the decision to submit the manuscript for publication.
Declaration of interest
S.D.Ø. received the 2020 Lundbeck Foundation Young Investigator Prize. S.D.Ø. owns and has owned units of mutual funds with stock tickers DKIGI, IAIMWC, SPIC25KL and WEKAFKI, and has owned units of exchange traded funds with stock tickers BATE, TRET, QDV5, QDVH, QDVE, SADM, IQQH, USPY, EXH2, 2B76 and EUNL. L.M.L. owns/has owned units of mutual funds with stock tickers DKIFJIX and units of exchange-traded funds with stock tickers JOBNDX, SOLAR B, PAAL B, NHY, NPAPER and RROS. The remaining authors declare no competing interests.






eLetters
No eLetters have been published for this article.