Diet is a key, modifiable health determinant. UK children’s diets are high in saturated fat and sugar and low in fibre and fruit and vegetables. For example, only 8 % of UK 11–18-year-olds are meeting the ‘5-a-day’ guideline, with socio-economic differentials(1). The quality of diet in childhood has been shown to impact on future development, educational achievement, health and well-being outcomes and also influences adult diet and non-communicable diseases risk (e.g. diabetes, CVD) in later life(Reference Craigie, Lake and Kelly2). We need effective and sustainable ways of helping young people, particularly in areas of socio-economic disadvantage, access a better diet, as early modification in eating habits and behaviours will decrease risk of developing such conditions(Reference Bennett, Hall and Hu3).
Schools play a crucial role in improving children’s health and are an obvious setting for population-level public health interventions(Reference Marmot4). They provide easy, and almost universal, access to pupils of various ages from across the social spectrum, with children spending approximately 40 % of their time awake every week day at school. Food provided in schools could have a major influence on children’s diet quality and has the potential to reduce inequalities in dietary intake(Reference Moore, Murphy and Chaplin5,Reference Spence, Matthews and White6) . Promoting the health and nutrition of the school food system can be seen as an essential activity that supports the goals of education. There are differences in how schools arrange their food provision and what they serve, between schools and UK regions, and this is not well understood. A systematic review of interventions to prevent childhood obesity highlighted, however, that establishing school environments and cultural practices that support children eating healthier foods throughout the day could be an effective intervention strategy(Reference Bleich, Vercammen and Zatz7).
UK school food was deregulated in 1980, and, between 2000 and 2013, each nation re-introduced school food standards across primary and secondary schools. These standards varied in content and timetable for implementation, but are now compulsory (in all nations since 2013), except for English academies founded between 2010 and 2014. Evaluation and monitoring of standards, and the requirements for reporting of these, across the UK have varied in scope, detail and timing(Reference Adamson, Spence and Reed8). When standards have been implemented, evaluations conducted in England suggest that the quality and nutritional value of food provided have improved, both within and beyond the school setting, and children from all socio-economic groups have benefitted(Reference Spence, Delve and Stamp9-Reference Evans, Melia and Rippin11).
There has, to date, been no formalised research, practice or policy network bringing UK school food stakeholders together to understand and share best practice. There is much to learn regarding the landscape and initiatives regionally that could be applied UK-wide. This required learning has been brought into sharp focus recently with the closure of schools during the COVID-19 pandemic, when the government response in terms of replacement support for those eligible for free school meals, and the heterogeneity with which alternatives were implemented, received much attention(12).
It is critical to policy development that the value of investment, innovation and change in the school food system are measured and protected using planned, appropriate, robust and timely evaluations, working across government departments and between countries. Broader insight is needed to provide a foundation for future actions, in terms of activities ripe for innovation, intervention development/testing and effective routes to influence policy.
School food system research: the health-promoting schools ‘whole-school approach’
The health-promoting schools (HPS) approach is advocated internationally to support and foster positive health behaviours(Reference Langford, Bonell and Jones13,Reference Wang and Stewart14) .
Recognising that education and health are intrinsically linked, the WHO defines a HPS as ‘a school that is constantly strengthening its capacity as a healthy setting for living, learning and working’. The WHO’s HPS Framework(15) advocates a ‘whole-school approach’ to promoting health via: provisions and activites relating to health-promoting school policies; the school’s physical and social environment; the curriculum; family and community links and health services at the school(Reference Turunen, Sormunen and Jourdan16).
Recent reviews of the HPS approach have indicated not only some successes but also gaps in the evidence base(Reference Langford, Bonell and Komro17-Reference Keshavarz, Nutbeam and Rowling20). Notably, activities to engage families and communities are weak, implementation in low-income settings is largely absent, most studies have focused on primary school-age children rather than adolescents and few interventions examine impacts on educational outcomes alongside health indicators. Furthermore, in terms of the robustness of the evaluation approach, evidence on sustainability, cost-effectiveness and contextual factors influencing effectiveness and implementation are lacking(Reference Langford, Bonell and Komro17-Reference Keshavarz, Nutbeam and Rowling20).
Whilst sytematic review evidence has revealed some school-level factors that contribute to the successful operation of HPS (such as school leadership, support from parents, community support, culture and capactity)(Reference McIsaac, Hernandez and Kirk18,Reference Hung, Chiang and Dawson19) , information on the broader system-level elements that may impact local implementation barriers and support uptake of a HPS approach is limited(Reference McIsaac, Hernandez and Kirk18). Several barriers to developing sustainable and effective HPS are proposed(Reference Keshavarz, Nutbeam and Rowling20) including poor understanding of the complexity of schools and how they function as complex adaptive systems; lack of acknowledgement of the diversity between schools; inadequate shared information and experience about the HPS approach between schools and also between the education and health sectors and lack of effective interactions between schools and parents about health(Reference Keshavarz, Nutbeam and Rowling20).
An example of application of the HPS approach is the HEALTHY study(Reference Gillis, Mobley and Stadler21). It modified the total school food environment and observed positive changes in the nutritional quality of foods and beverages available in schools and modest improvements in fruit and water consumption(Reference Gillis, Mobley and Stadler21). Other components were physical education, behaviour change and social marketing. A systematic review of the impact of multi-strategy nutrition education programmes on the health and nutrition of adolescents(Reference Meiklejohn, Ryan and Palermo22) also highlighted the important role of schools, stating that such interventions can significantly impact on adolescent nutrition, when the nutrition education is theoretically based and facilitated by school staff in conjunction with parents and families, and includes changes to the school food environment.
These whole school nutrition interventions exist that may be relevant to the UK setting; however, an understanding of context is essential to inform implementation and testing of approaches that have been developed in other countries. As highlighted by Turunen(Reference Turunen, Sormunen and Jourdan16), the factors that influence implementation of HPS interventions are numerous, variable and contextually influenced. It is essential to understand the complexity of the school food system in the UK in order to tailor and embed interventions appropriately in different contexts according to local needs(Reference Hung, Chiang and Dawson19). There is also value in taking stock of current evidence and practice in order to develop a future research agenda that meets the needs of schools, pupils, parents and the wider community. Such an exercise has not been undertaken to date in the UK.
Themes relevant to school food research
A systems approach to school food, and considering schools as a complex adaptive system, may be pertinent to first understand their complexity and then allow the opportunities for innovation and intervention to be fully realised. However, even without such a methodology yet being applied, it is likely that the following themes will be relevant.
-
School food policies and standards: nutrient and food-based standards across the UK need to be scoped, as does the evidence on which these are based. The policies and standards range according to age, are in place for school meals, but also for packed lunches and broader food provision in schools, e.g. vending machines (including beverages), breakfast clubs, after school clubs, tuck shops and snack foods. Provision of free school meals and the extent to which these are taken up, and actually consumed, also needs to be explored. Such a scoping exercise will identify gaps and explore heterogeneity in how standards are implemented and monitored. A similar, although higher level, analysis was conducted in 2014 across Europe, but did not capture the UK in detail(23), whilst the previous UK-focused review is now outdated(Reference Adamson, Spence and Reed8). Opportunities to evaluate policy change need to be capitalised, e.g. introduction of universal infant free school meals and the role of advocacy considered.
-
School food procurement/provision: models of school food procurement/provision across the UK vary, with no consensus around what good practice is in terms of effectiveness, efficiency and sustainability. Metrics of good practice may include high uptake rates, increased diet quality, sustainability, reduced food miles, low levels of waste, both within the kitchen and plate waste in the canteen and cost efficiencies. Similarly, little is known about how savings, efficiencies and improvements in quality could impact in the long term on economic, educational and health outcomes. Increasing uptake of free school meals or improving meal quality with minimal financial impact on families could potentially reduce socio-economic inequalities.
-
The school food environment: long queuing times and concerns about hygiene and the quality of food offered are frequently mentioned barriers to school meal acceptability(Reference Payán, Sloane and Illum24). Modifiable factors within the school food environment need to be explored, including timing of school meals, food sourcing practices and dining environment, i.e. a welcoming social environment and a lack of queues. How the school leadership team can intervene to successfully achieve such culture change must be determined, as should how catering staff training might help encourage children to eat higher nutritional quality foods. The feedback received from pupils, teachers and other staff members is likely to be of key importance to the success and development of the school food system, and therefore a direct and interactive feedback mechanism which supports concrete actions should be considered.
-
School food system data collection: limited data on school food are routinely collected throughout the UK, but a thorough understanding of what is available, for example, from local authorities in terms of school meal uptake, adherence to standards, would help to plan research with routine outcome assessment and allow potential linkage, for example, to educational, welfare and health outcomes. Harmonisation of data collection methods across the UK, including consideration of the key timepoints for data collection to allow the monitoring of trends over time and the impact of policy changes, would aid this. The use of technology to improve data collection, for example, exploiting big data from cashless meal card food purchases, should be considered.
-
Interventions in school settings: much work is already being conducted in UK schools(Reference Nathan, Janssen and Sutherland25,Reference Langford, Jago and White26) , but a thorough scoping review of current interventions to gain consensus on those likely to be successful would enable these to be tested on a larger scale. These could include not only whole school approaches but also age-specific meal size guidance for catering staff, interventions changing menu cycling and number/type of options and utilising food choice architecture. Exploring how interventions could be implemented in practice, at scale and funding mechanisms will be important. Effects of such interventions on broader dietary change, for example, food intake at home, should also be examined. The theoretical basis (explicit or implicit) of existing or potential interventions needs to be explored, exploring the broad behaviour change routes that interventions may target, such as motivation, action, prompting or maintenance processes. Moreover, the specific ‘mechanisms of action’ within behaviour change processes will need to be identified (e.g. food literacy, confidence, knowledge and attitude for motivational processes, changing social norms and school food culture) and mapped onto the existing and potential tools and strategies for behaviour change to arrive at an adaptable theory-based toolkit with potential for cross-translation and testing in different school-based contexts.
The GENIUS school food network
The UKPRP-funded GENIUS network(27,28) will consider the food system across preschool, primary and secondary settings and include all school food provision, within canteens, vending machines, shops and home-prepared packed lunches, and also the school fringe environment. The overarching aim of this network is to build a community to work towards a more health-promoting food and nutrition system in UK schools. Specific objectives include the development of a network of academics and non-academics across the UK actively researching and influencing the school food system, the use of a range of methodologies, including systems mapping and network analysis, to understand the current UK school food landscape, including similarities and differences, areas of best practice, and, finally, the exploration of opportunities for population- and system-level interventions that will positively impact diet quality and inequalities.
The network brings together an interdisciplinary team, including nutrition, epidemiology, public health, systems science, sensory science, health economics, health informatics, health psychology, education, planning and policy, to comprehensively examine school food in its broadest and most complex sense. Inclusion of non-academic project partners from across the UK will prioritise stakeholder/user engagement and allow the co-development of research priorities. The work of the network is at an early stage but, given the likely themes listed above, and early discussion amongst network members, Figure 1 demonstrates the themes with some consideration of how they inter-relate and how they might be prioritised.
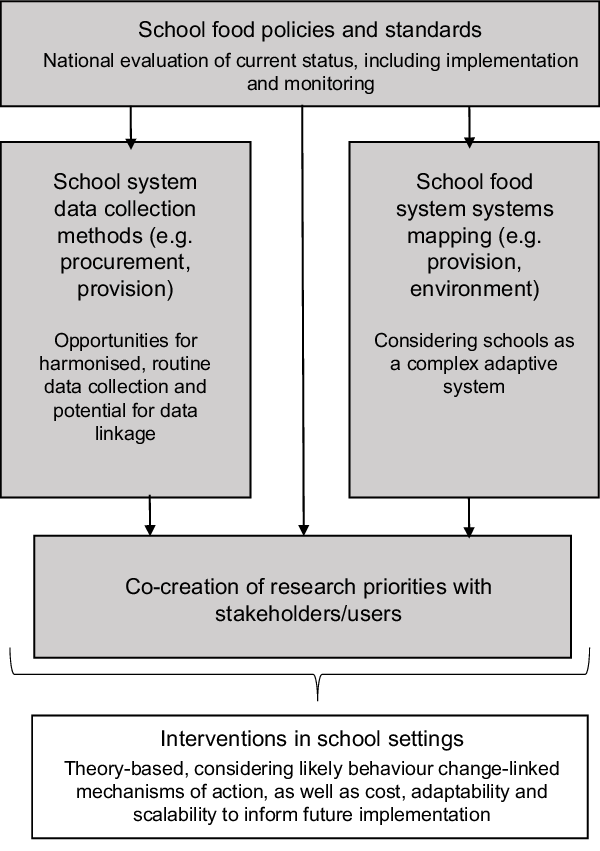
Fig. 1 Themes relevant to school food research. ![]() , Prioritised research themes and activities within the GENIUS network
, Prioritised research themes and activities within the GENIUS network
Conclusion
The GENIUS network will bring together a wide range of UK school food stakeholders to build a better understanding of the school food system, innovate, co-create and share best practice. Understanding the current food system and building network expertise will advance research to better inform policy and good practice around food in schools. The co-production of priorities for research and changes in practice will ensure that the activities of the network are relevant for beneficiaries (families with school-age children), stakeholders (teachers, principals, catering staff and policymakers) and are, thus, more likely to result in meaningful and sustained changes in policy and practice. The network ultimately aims to effect an improvement in school food quality, normalise evidence-based healthy food practices within school settings and change school food culture and practice, creating healthier school food environments which are accessible to all, reducing socio-economic diet-related inequalities, and, consequently, non-communicable diseases risk.
The GENIUS network consists of:
Jayne Woodside, Michelle McKinley, Ciaran O’Neill, Laura Dunne, Ruth Hunter, Queen’s University Belfast; Ashley Adamson, Suzanne Spence, Newcastle University; Laura Johnson, Angeliki Papadaki, University of Bristol; Stephanie Chambers, University of Glasgow; Charlotte Evans, Hannah Ensaff, University of Leeds; Julie Lovegrove, Lisa Methven, Jeremy Spencer, Kate Harvey, University of Reading; Annie Anderson, University of Dundee; Sinead Brophy, Swansea University; Kevin Morgan, Cardiff University; Stephan Dombrowski, University of New Brunswick.
Acknowledgements
Acknowledgements. The authors wish to acknowledge the administrative support provided by Ms Angela Mullan. Financial support. This work was supported by the Medical Research Council (grant number MR/S03756X/1). Conflict of interest. The authors declare no conflicts of interest. Authorship. J.V.W. is PI of the GENIUS network and produced the first draft of the commentary. A.A., S.S., T.B. and M.McK. provided feedback and revised this first draft. All authors approved the final version of the manuscript. Ethics of human subject participation. This commentary does not describe research involving human participants.






