Introduction
The Centre for Anxiety Disorders and Trauma (CADAT) is a national specialist out-patient service that treats patients with anxiety disorders in the UK. Evidence suggests that integrative and collaborative care, including videoconferencing therapy, may effectively treat anxiety disorders (Muntingh et al., Reference Muntingh, van der Feltz-Cornelis, van Marwijk, Spinhoven and van Balkom2017). Despite this knowledge, videoconferencing was not offered routinely at CADAT due to an assumption that online sessions were less effective than face-to-face sessions, more difficult to engage patients in active work, and less acceptable to patients. As a result, almost all patients were required to attend CADAT regardless of distance from the clinic.
In the UK, since the nationwide introduction of a lock-down system due to COVID-19, there has been a decline in mental health (Daly et al., Reference Daly, Sutin and Robinson2020). COVID-19 has exacerbated difficulties for people with a range of mental health disorders, including those with anxiety disorders (Shevlin et al., Reference Shevlin, McBride, Murphy, Miller, Hartman, Levita, Mason, Martinez, McKay, Stocks, Bennett, Hyland, Karatzias and Bentall2020). Mental health services have been obligated to shift from in-person therapy to alternative mediums for treating anxiety disorders, such as videoconferencing, telephone, or resorting to temporary pausing of services altogether due to COVID-19 (Jassi et al., Reference Jassi, Shahriyarmolki, Taylor, Peile, Challacombe, Clark and Veale2020; Murphy et al., Reference Murphy, Calugi, Cooper and Dalle Grave2020). To better inform clinical practices and protocols, clinicians and researchers need to consider further the clinical implications of cognitive behavioural therapy (CBT) videoconferencing for people with anxiety disorders.
The effectiveness of CBT videoconferencing
CADAT offers CBT, a National Institute for Health and Care Excellence (NICE) recommended effective intervention to treat anxiety disorders (NICE, 2014). Several studies have also demonstrated that CBT videoconferencing successfully reduces psychological symptoms and is highly acceptable as a treatment (see Berryhill et al., Reference Berryhill, Halli-Tierney, Culmer, Williams, Betancourt, King and Ruggles2018). Findings from randomised controlled studies (RCTs) are also promising, demonstrating that CBT videoconferencing is equally effective as in-person treatment for mood and anxiety disorders (Stubbings et al., Reference Stubbings, Rees, Roberts and Kane2013). Another systematic review of videoconferencing therapies and anxiety disorders showed further evidence for the effectiveness of CBT videoconferencing; however, more controlled studies were required, particularly for general anxiety disorder (GAD) (Rees and Maclaine, Reference Rees and Maclaine2015). In summary, the literature highlights strong evidence for the effectiveness of CBT videoconferencing in anxiety disorders.
Patient and therapist aualitative experiences of CBT videoconferencing
Few studies document qualitative experiences of CBT videoconferencing. Specifically, limited studies report both therapist and client experiences or specific mechanisms of change in CBT videoconferencing. Of the few, some qualitative studies explore therapist experiences of CBT videoconferencing and emphasise associations between usage, increased positive attitudes, and previous online experiences. Initially, therapists often met technical difficulties and implementation issues but became more comfortable implementing CBT videoconferencing as they continued to use it (Khatri et al., Reference Khatri, Marziali, Tchernikov and Shepherd2014). Therapists’ views on videoconferencing also tended to increase positively with usage, and those with more online experience tended to report fewer technical and relational challenges (Connolly et al., Reference Connolly, Miller, Lindsay and Bauer2020).
Moreover, therapists who had previous online experience reported that patients were more likely to report positive experiences (Békés and Aafjes vanDoorn, Reference Békés and Aafjes vanDoorn2020). Other therapists have reported self-doubt about the therapeutic alliance and anxiety regarding therapeutic interaction while using CBT videoconferencing, although objective patient measures depicted working alliance and rapport remained intact (Aafjes-van Doorn et al., Reference Aafjes-van Doorn, Békés and Prout2020). Despite reporting self-doubt, most therapists still had a positive attitude towards videoconferencing.
Patient qualitative experiences of CBT videoconferencing are limited to post-traumatic stress disorder (PTSD) and obsessive compulsive disorder (OCD). In patients with OCD, videoconferencing was highly acceptable, with high treatment satisfaction and good therapeutic rapport (Himle et al., Reference Himle, Fischer, Muroff, Van Etten, Lokers, Abelson and Hanna2006). Furthermore, high ‘telepresence’ was also reported at pre- and post-treatment. ‘Telepresence’ refers to the felt sense of being in the room with the therapist and not in a remote space (Bouchard et al., Reference Bouchard, Paquin, Payeur, Allard, Rivard, Fournier, Renaud and Lapierre2004). Patients with PTSD described similar reports of remote therapy feeling indistinguishable from being in the room with the therapist, suggesting evidence of telepresence (Ashwick et al., Reference Ashwick, Turgoose and Murphy2019).
These studies provide some insight into patients’ experiences of CBT videoconferencing. However, studies depicting both patients’ and therapists’ qualitative experiences of CBT videoconferencing are limited. The UK government imposed COVID-19 restrictions on mental health services resulting in guidelines for adapting psychological therapies such as CBT for videoconferencing (British Psychological Society, 2020). Investigating both therapists’ and patients’ perspectives may provide a more collective and holistic approach and further inform service protocols. This study aims to explore patients’ and therapists’ experiences of CBT videoconferencing. The results of this study can help develop service policies to guide the use of videoconferencing therapy after the pandemic has ceased.
Method
Participants and experiences of CBT videoconferencing survey
Patients (n = 19) and therapists (n = 18) were recruited from CADAT at the South London and Maudsley NHS Foundation Trust (SLAM). The recruitment process was purposeful as CADAT patients and therapists were deemed able to provide in-depth information for the purposes of the study (Neergaard et al., Reference Neergaard, Olesen, Andersen and Sondergaard2009). All patients who gave consent to be contacted for research and received individual CBT videoconferencing at any stage in their treatment were sent the survey. All therapists that provided CBT videoconferencing were also sent a survey. Fifty-four (45.4%) patients completed the survey (female, n = 29; male, n = 15; genderqueer, n = 1).Footnote 1 The age range was from 21 to 62 years (mean = 34.32, SD = 10.29). Patients had the following diagnoses: OCD (n = 14, 26%), social anxiety disorder (SAD; n = 3), GAD (n = 6), body dysmorphic disorder (BDD; n = 1); emetophobia (n = 1); agoraphobia (n = 2); misophonia (n = 3); health anxiety (n = 3), depersonalisation (n = 2) and PTSD (n = 2).Footnote 2 Fifteen therapists (83.3%) completed the survey (female, n = 7; male, n = 5). The therapists’ mean age was 41 years (SD = 5.17), and their roles were clinical psychologists (n = 7), counselling psychologists/CBT therapists (n = 4), and trainee clinical psychologist (n = 1).Footnote 3
Procedure and materials
Patients and therapists were sent an email invitation that included the project URLs. When patients and therapists clicked on the project URL, a study information page was provided. The study information page clearly stated that as personal identifiers were not required to complete the questionnaires, the research team had no means to trace participants to the completed surveys once conducted. Therefore, the researchers could not withdraw their data. The next page included demographic questions that captured information to characterise the patient and therapist sample (see Supplementary material, sections 1 and 2). A follow-up call, email,or text was sent to therapists and patients 2 weeks after the initial invitation to increase response rates. Patients and therapists were recruited for the survey over 4 weeks (from 30 June 2020 to 30 July 2020).
Patient survey
The patient survey contains nine items (see Supplementary material, section 3). The first two questions were open-ended questions that captured experiences of videoconferencing. The third, an open-ended question, asked how patients’ attitudes towards therapy via videoconferencing had changed due to the COVID-19 restrictions. The fourth question also enquired about attitude change using a 0–100 response scale (0 = negatively changed, 50 = no change and 100 = positively changed). The next two questions asked about specific active CBT techniques. Finally, questions 7, 8 and 9 captured patient satisfaction, service recommendations, and suggestions for improvement. The survey took approximately 10 minutes to complete.
Therapist survey
The online survey about therapists’ experiences of delivering CBT videoconferencing contains 21 items (see Supplementary material, section 4). Questions 1 to 3 asked how many patients therapists had treated and assessed online and which type of media platform was used. The next six open-ended questions asked about therapists’ experiences of using specific CBT techniques, the involvement of family members in sessions and technological issues. Questions 10 to 12 asked about how sessions were recorded and the number of patients that declined CBT videoconferencing sessions and assessments. The next five questions were open-ended questions asking about the reasons for declining, the advantages and disadvantages of CBT videoconferencing, treating different anxiety disorders, and how COVID-19 restrictions have changed their attitude. As asked in the patient survey, question 18 captured the extent to which therapist attitude has changed towards CBT videoconferencing due to the COVID-19 restrictions, with a 0–100 response scale (where 0 = negatively changed, 50 = no change and 100 = positively changed). The last three open-ended questions asked about adaptions made to treatment due to its remote delivery, helpful ways of sharing treatment material, and whether they had any other experiences that they felt would be useful to share. The survey took approximately 15–20 minutes to complete.
Analysis
Qualitative content analysis was used to explore the patients’ and therapists’ responses (Krippendorff, Reference Krippendorff2018). The process involved establishing meaning units, codes, categories and themes, and identifying their frequency (Marks and Yardley, Reference Marks and Yardley2011). Content analysis is useful in analysing a person’s experiences, reflections and attitudes (Downe-Wamboldt, Reference Downe-Wamboldt1992). The study adopted an inductive approach while using both manifest and latent analysis. Manifest analysis refers to researchers reviewing information that is easily observable or ‘staying close to the text’, and latent analysis is defined as when researchers go beyond the text and focus on the implied meaning of the text (Graneheim and Lundman, Reference Graneheim and Lundman2004). The study was performed in three steps: preparation, organisation and reporting (Elo and Kyngäs, Reference Elo and Kyngäs2008). During the preparation step, researchers immersed themselves in the data to obtain a sense of the whole texts, selecting units of analysis. Next, organisation involved dividing the text into meaning units, for example words, sentences and paragraphs. Then meaning units were coded inductively, grouped to create categories and themes, and general descriptions of codes recorded at the manifest level (Krippendorff, Reference Krippendorff2018). Codes that deviated from the aim were excluded, for example comments on other psychological models and comments about the NHS in general. Two researchers (an assistant psychologist and a trainee clinical psychologist) performed the preparation and organisation step independently and then discussed their results with a third researcher (a clinical psychologist) to obtain consensus. This method of triangulation is often used to maintain validity (Graneheim and Lundman, Reference Graneheim and Lundman2004; Rolfe, Reference Rolfe2006). Finally, researchers described the analysis process in the reporting step and reflected on the categories to produce themes at a latent interpretative level (Graneheim and Lundman, Reference Graneheim and Lundman2004).
Results
Patient frequency scores from patient survey
Table 1 presents frequencies of patient-reported CBT components and patient stage of therapy. Half of the patients were towards the end of their therapy (50.0%), the majority of patients had set or reviewed homework (76.1%) and less than half conducted BEs and completed formulation (47.8%). The mean score of the degree to which COVID-19 affected patients’ attitudes towards CBT videoconferencing (where 100 = positive and 0 = negative) was 63.30 (SD = 21.78). Figure 1 presents patient satisfaction scores. Overall, 47.27% (n = 26) of patients were extremely satisfied, 30.91% (n = 17) somewhat satisfied, 5.45% (n = 3) neither dissatisfied nor satisfied, 7.27% (n = 4) somewhat dissatisfied, and 9.09% (n = 5) extremely dissatisfied with CBT videoconferencing. Sixty-one per cent of patients (n = 27) were extremely likely and 34.1% (n = 15) likely to recommend the service at CADAT to their friends and family. Five per cent (n = 2) were unlikely or extremely unlikely to recommend CBT videoconferencing due to the format.
Table 1. Frequencies of CBT components and stage of therapy (patients)

* Missing information (n=8).
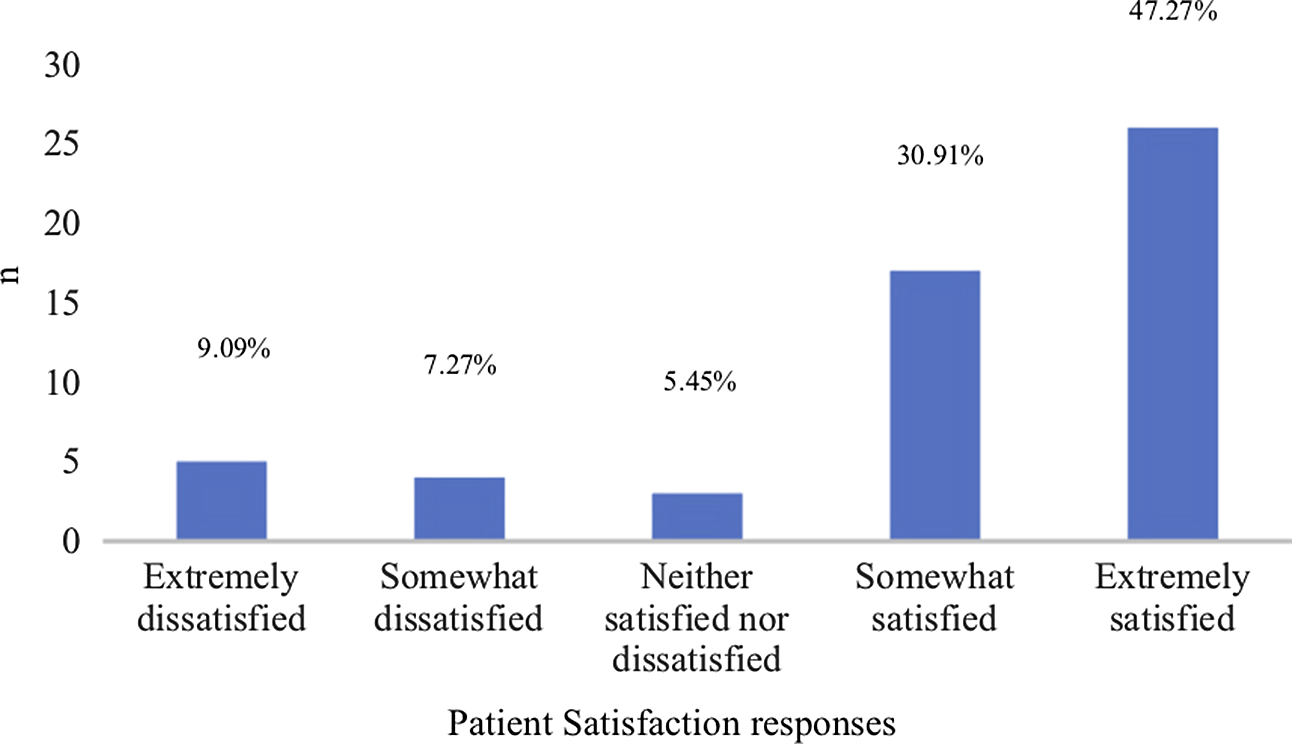
Figure 1. Patient satisfaction responses.
Therapist frequency scores from therapist survey
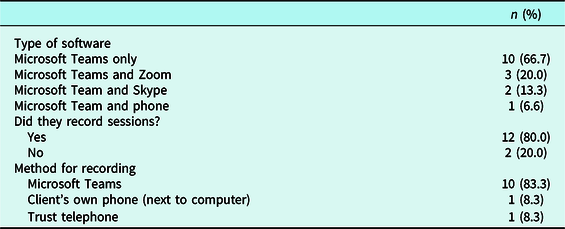
Table 2 presents frequencies regarding the type of software used for videoconferencing and how the sessions were recorded. The mean score of the degree to which COVID-19 affected therapists’ attitude towards CBT videoconferencing (where 100 = positive and 0 = negative) was 72.67 (SD = 15.43). The mean number of patients therapists saw using videoconferencing was 9.67 (SD = 6.24). The mean number of patients assessed was 4.8 (SD = 5.25). The mean number of clients that declined CBT videoconferencing was 2.67 (SD = 3.87) and .67 (SD = 0.976) that declined assessment.
Table 2. Frequencies of the type of software and what method (therapists)
Qualitative content analysis of patient and therapist survey
The results of the content analysis from the surveys revealed four themes. All codes and quotes can be found in supplementary material, section 5.
Theme 1: Behavioural experiments work well if the problem lends itself to CBT videoconferencing
Theme 1 contains two categories: positive behavioural experiment (BE) experiences and COVID-19 restrictions may confound BEs.
Category: Positive behavioural experiment (BE) experiences
This category contains two subcategories: patients’ and therapists’ experiences, and home environment is ideal.
Subcategory: Patients’ and therapists positive experiences
Many patients reported that BEs were helpful, practical, flexible and implementable; BEs could be done in the home and outside. The majority of therapists also encountered encouraging experiences of BEs; for example, three therapists commented on BEs working well with BDD, SAD and hoarding; seven therapists reported BEs working well for OCD; and two therapists for emetophobia. One therapist also reported that BEs were successful if they were amenable to the virtual medium. For instance, in CBT treatment for SAD, stooge experiments are typically conducted and involve volunteers who participate in a social experiment with the person with SAD (Wells et al., Reference Wells, Clark, Salkovskis, Ludgate, Hackmann and Gelder2016). It was easier to record such experiments and provide video patient feedback when conducted via videoconferencing.
Subcategory: The home environment is ideal
Almost half of the therapists reported that the home environment contributed to successful BE experiences and brought many opportunities to test cognitions in BEs. In addition, the home environment allowed therapists to see their patients in their own space and support them whilst doing experiments in real-time. This resulted in a better generalisation of the key learnings from experiments.
Category: COVID-19 restrictions may confound BEs
It was clear from the findings that both patients and therapists reported that COVID-19 restrictions may have confounded some BEs. For example, one patient with SAD reported that although BEs were successful through videoconferencing, previous BEs held in person were deemed more challenging and potentially more rewarding. Furthermore, another patient with SAD commented that testing their safety-seeking behaviours (SSBs) in BEs in person would have been more effective, as being with people would have been more realistic. Similarly, one therapist reported that the absence of being in the room might create barriers in noticing patients’ potential SSBs. Four therapists also reported that lockdown confounded BEs and that anti-OCD experiments, which directly challenge the problematic OCD thoughts and behaviours, were difficult to conduct.
Exposure-based tasks are integral techniques in CBT for the treatment of anxiety disorders. It involves experiencing stimuli specific to the patient’s psychological concerns to modify their problematic thoughts and acquire new learning (Kaczkurkin and Foa, Reference Kaczkurkin and Foa2015). Three therapists reported that specific elements of exposure-based experiments were difficult to set up whilst using videoconferencing due to COVID-19. Under half of the therapists further said some exposure-based experiments were difficult to complete for specific disorders such as emetophobia, OCD, SAD and panic disorder. Some therapists who worked with patients with SAD described that exposure-based experiments were harder to do, given that virtual stooges do not necessarily reflect real-life social interaction. Two patients explained that attending in-person sessions was an exposure-based experiment and that attending videoconferencing sessions lost the opportunity to do exposure experiments.
Theme 2: Overall practicalities, but some home environment implications
This theme has two categories: practical elements and home environment issues.
Category: Practical elements
Several subcategories fall under practical elements: opportunity to access treatment during the pandemic, helpful elements, and unhelpful elements.
Subcategory: Opportunity to access treatment during the pandemic
Just over a third of patients described being able to start or continue CBT during the pandemic as an advantage, thus illustrating a method that allowed them to address their mental health difficulties without disruption. In addition, for some patients, being able to have contact or continue to have contact with their therapist meant one less worry, particularly in difficult circumstances where most public services had stopped due to COVID-19.
Subcategory: Helpful elements
The majority of patients and therapists reported practical advantages to CBT videoconferencing. Twelve patients found that Microsoft Teams made it easier to show and share documents and make notes simultaneously. Nine therapists also shared this opinion. Of these nine, five also described the ease of sharing electronic documents and therapy material through email as an advantage of videoconferencing therapy. CBT videoconferencing created a sense of increased flexibility, which was common among therapists. Therapists reported that it made it easier to fit around their schedule. CBT videoconferencing also allowed more opportunities to conduct exposure/experiments around home-based problems.
Eight patients reported this same ease of sharing information for formulation. CBT formulation involves a collaborative exploration and understanding of the patient’s mental health difficulties between patient and therapist (Fenn and Byrne, Reference Fenn and Byrne2013). Formulation essentially hypothesises a ‘road map’ of the patient’s cognitions, behaviours and emotions. It is typically visibly drawn on a whiteboard, handwritten on paper or typed up in a Word document. Two therapists similarly reported that formulation worked well and aided collaboration through screen-share and whiteboard options.
Over a fifth of patients reported that they did not have to travel. It was apparent that some patients found videoconferencing very convenient by saving commuting time, freeing up time, or conveniently fitting around their schedule, particularly those who lived at some distance from CADAT and saved on travel costs. Furthermore, six patients explained that not travelling meant less anxiety, as many felt anxious about taking public transport. Almost half of the therapists also reported not having to travel due to videoconferencing therapy meant saving on time.
Subcategory: Unhelpful elements
Conversely, four patients explained elements of formulation that were not as practical through CBT videoconferencing. For example, handwritten formulation was more difficult to carry out, and that not using a whiteboard meant missing out on a collaborative experience between patient and therapist. In addition, three patients reported that videoconferencing medium itself was far from ideal as it appeared to make the sessions seem slower and less productive. Four therapists also said comparable undesirable formulation experiences; the process took longer than usual, and formulating online was harder and less collaborative.
Category: Home environment
This category has four subcategories; the comfort of own home, home environment issues, privacy issues and technical issues.
Subcategory: Comfort of own home
Eight patients described having CBT videoconferencing in the comfort of one’s own home as positive. Speaking about difficulties at home seemed less embarrassing and felt more private. The responses also illustrated that the home environment brought comfort and a sense that therapy was less invasive and, therefore, less anxiety-provoking. Some patients also found the home a safe place to do therapy online.
Subcategory: Home environment issues
On the contrary, three patients reported that the home environment was not ideal for discussing their problems; they were familiar with discussing therapy issues outside of the home or felt that home was usually associated with relaxing and sleeping. In addition, two patients reported that the safe therapeutic space typically provided by in-person therapy was removed, resulting in a lack of mental distance between home and treatment. Finally, three patients also found that being at home provided unwelcomed distractions and motivation for therapy was difficult.
Similarly, CBT videoconferencing in the home was not ideal for some patients, as described by six therapists, due to the need for therapeutic space and boundaries outside of the home to feel safe. In addition, a few therapists described remote therapy as unsuitable for people with PTSD and CPTSD due to the risk of dissociation. Dissociation is characterised as disrupting the normal integration of consciousness, memory, identity, emotion, perception, body representation, motor control and behaviour (American Psychiatric Association, 2013). Therefore, a patient at risk of dissociation may be more problematic to support without the therapist being present in the room. Furthermore, the home environment provided unwanted distractions from the therapy session itself for the patient.
Subcategory: Privacy issues
Eight patients reported being unable to speak freely in their own homes, resulting in worries about confidentiality and privacy. Three patients explained that due to COVID-19 lock-down, housemates or family members would be present in the home. A third of therapists also shared concerns about their patient’s privacy, which may have resulted in difficulties with engagement with some patients.
Subcategory: Technical issues
Almost a third of patients reported technical issues such as software difficulties or internet connection, as did therapists. Two therapists stated that poor internet connection resulted in problems building a therapeutic alliance. In addition, implementation issues such as administering measures and setting up videoconferencing were time-consuming. Close to a third of therapists reported that patients had digital poverty; patients have limited access to technology such as the internet, smartphones, and other smart devices. The finding suggests that such patients are at a disadvantage in accessing therapies.
Theme 3: High telepresence and the negative impact on therapeutic alliance
Theme 3 contains two categories: telepresence and negative therapeutic alliance.
Category: Telepresence
Five patients reported no differences between CBT videoconferencing than in person and that the quality of the therapy received in videoconferencing was the same. This finding suggests telepresence and acceptability of CBT videoconferencing. Two patients said this was also the case when doing BEs during video call sessions. Five therapists also reported telepresence while using imagery rescripting and that imagery rescripting was successful. Imagery rescripting involves a pre-existing negative mental image that is transformed or ‘rescripted’ into a more positive image, or a new positive image is created instead to capture positive meanings required to offset the central psychological beliefs for a person (Holmes et al., Reference Holmes, Arntz and Smucker2007).
Category: Negative therapeutic alliance
Almost half of the patients reported that videoconferencing impacted the therapeutic alliance adversely; the medium contributed to feeling impersonal, with poor rapport, less communication, and less human interaction. Without being in the same room as their therapist, some patients thought it was not easy to read facial expressions and body language, which meant that subtle communication might have been lost. Two therapists also reported that CBT videoconferencing harmed the therapeutic relationship. Two therapists explained that it was difficult to notice emotional responses and that videoconferencing was not ideal in addressing affect in the room. Three therapists described that some imagery experiences through CBT videoconferencing made assessing the patients’ affect or emotion more difficult than when in the room. Furthermore, some therapists felt a loss of non-verbal communication, resulting in reduced therapeutic rapport and intimacy.
Theme 4: COVID-19 restrictions may influence attitudes towards CBT videoconferencing positively
This theme has two categories: no attitude change and positive change in attitude.
Category: No attitude change
Less than a fifth of patients and a fifth of therapists reported no attitude change towards CBT videoconferencing. Some patients who were towards the end of their treatment stated that despite the COVID-19 restrictions causing them to transition from in-person CBT to videoconferencing, they had no change in attitude towards video call, whether positive or not. Two other patients reported no change in their existing positive attitude towards CBT videoconferencing. Of this one-fifth of therapists, three therapists also reported no change in their initial positive attitude. These therapists also remained positive and amenable towards videoconferencing.
Category: Positive change in attitude
Over a third of patients and half of the therapists reported a positive attitude towards video calls due to the COVID-19 restrictions enforcing services to use CBT videoconferencing. This resulted in a willingness to use CBT videoconferencing in the future, beyond the pandemic. Five patients and five therapists were initially sceptical towards videoconferencing before the COVID-19 restrictions occurred, and it took the pandemic to overcome this. However, five patients were surprised to see that videoconferencing was possible and worked in general. Two patients also reported that their confidence in using technology had, in general, increased. Since moving to remote working, four therapists have changed their attitudes; one reported that it increased their confidence in videoconferencing and welcomed more videoconferencing sessions in the future.
Discussion
The results from the content analysis revealed four themes that may further the understanding of patient and therapist experiences of CBT videoconferencing. The findings also suggest that most patients were satisfied with CBT videoconferencing, and most patients were likely to recommend the service to their friends and family. Furthermore, COVID-19 restrictions meant that patients had no alternative but to use videoconferencing, consequently leading to more experiences with using videoconferencing, which may have contributed to changes in patients’ and therapists’ attitudes towards CBT videoconferencing. In summary, the results suggest that CBT videoconferencing had a favourable impression on patients and therapists.
Theme 1: Behavioural experiments work well if the problem lends itself to videoconferencing
Theme 1 encapsulates patients’ and therapists’ experiences of how successful some BEs were in CBT videoconferencing due to psychological problems that were amenable to being addressed virtually both inside and outside the home. However, some BEs may have been limited due to several factors, including the COVID-19 lockdown restrictions. Nevertheless, BEs are a key active change technique used in CBT and are central to testing key cognitions when treating anxiety disorders (Bennett-Levy et al., Reference Bennett-Levy, Butler, Fennell, Hackmann, Mueller and Westbrook2004; Clark, Reference Clark1999; Wells et al., Reference Wells, Clark, Salkovskis, Ludgate, Hackmann and Gelder2016).
Examples of patients who experienced some successful BEs were patients with OCD who had contamination obsessions who avoided touching objects within their home. The home environment was ideal as therapists could see patients in their own space and support them in vivo, while patients learnt that they could tackle their OCD on their own, outside of the therapy room. Our findings align with a previous study that demonstrated CBT videoconferencing was an acceptable treatment, with high patient satisfaction (Himle et al., Reference Himle, Fischer, Muroff, Van Etten, Lokers, Abelson and Hanna2006). For BEs that occurred outside and were amenable to videoconferencing, this virtual medium allowed the therapist to accompany patients on BEs whilst out on a walk whilst simultaneously providing support and coping strategies to the patient in real-time via a phone. COVID-19 lockdown restrictions may have limited other BEs. For some patients with SAD and agoraphobia, the act of coming to therapy sessions at CADAT was exposure itself for patients, and this opportunity was missed. Furthermore, some patients with OCD were co-habiting and could not do anti-OCD experiments, such as leaving the window open and leaving their homes. Housemates at home meant they would share the responsibility if something terrible happened.
Theme 2: CBT videoconferencing has practicalities but has some home environment implications
The second theme highlights the largest practical advantage for both patients and therapists; saving on costs and travel and capturing the implications of the home environment on CBT videoconferencing. Other practical benefits to CBT videoconferencing included opportunities to continue therapy during the pandemic, the ease of sharing therapy documents through share-screen functions and emails and saving on costs and travel. In addition, the Microsoft Teams platform made self-review easier for some patients to watch back, reflect, and retain information. Furthermore, computer software programs, such as MS Office packages, enabled resources to be sent and received easily and allowed clients and therapists to write notes during sessions. The findings are in line with previous literature (Luo et al., Reference Luo, Sanger, Singhal, Pattrick, Shams, Shahid, Hoang, Schmidt, Lee, Haber, Puckering, Buchanan, Lee, Ng, Sun, Kheyson, Chung, Sanger, Thabane and Samaan2020; Simpson et al., Reference Simpson, Bell, Knox and Mitchell2005).
Many patients and therapists reported negative and positive experiences of CBT videoconferencing when received and delivered at home. Therapists felt that patients could receive therapy in the comfort of their own homes whilst also allowing more opportunities to address concerns centred around the home. Conversely, the home environment had some issues regarding therapeutic space, privacy, and technical issues. For example, patients reported that typical therapeutic space and boundaries in in-person therapy were removed from video call sessions at home. Furthermore, some patients with PTSD who discussed trauma in their own homes felt that the lack of therapeutic space removed a sense of safety. For example, they struggled with processing trauma memories when implementing re-living techniques in their own home. This is congruent with other studies demonstrating mixed positive and negative experiences of CBT videoconferencing (Ashwick et al., Reference Ashwick, Turgoose and Murphy2019; Stubbings et al., Reference Stubbings, Rees and Roberts2015).
Due to the UK Government imposing restrictions where patients and therapists stayed and worked from home, some therapists often felt privacy issues in the home environment, which led to poorer engagement in CBT videoconferencing sessions. For example, some therapists felt that their client’s attention might be divided due to family members being present. Similarly, patients reported they could not speak freely due to fear of being overheard by housemates or loved ones. This finding contrasts with earlier research that videoconferencing may facilitate disclosure and the freedom to talk openly (Gibson et al., Reference Gibson, Coulson, Miles, Kakekakekung, Daniels and O’Donnell2011). In addition, COVID-19 lockdown restrictions may have likely exacerbated this unsuitable home environment by forcing the public to be at home. The finding further suggests that privacy is a significant concern when interventions are delivered via videoconferencing, in line with previous literature (Connolly et al., Reference Connolly, Miller, Lindsay and Bauer2020; Gibson et al., Reference Gibson, Coulson, Miles, Kakekakekung, Daniels and O’Donnell2011; Kramer et al., Reference Kramer, Mishkinda, Luxton, Shore, Myers and Turvey2013; Simpson et al., Reference Simpson, Bell, Knox and Mitchell2005).
There were numerous reports of software difficulties and Wi-Fi connection issues, although this did not seem to impact the patient’s self-reported satisfaction with the treatment overall. Technical and connection problems are not new to the literature (Aafjes-van Doorn et al., Reference Aafjes-van Doorn, Békés and Prout2020; Deslich et al., Reference Deslich, Stec, Tomblin and Coustasse2013). Moreover, therapists felt setting up video calls was time-consuming, reporting implementation issues. Nevertheless, the findings indicate that improving or ensuring high-quality broadband may help address these connection issues in the future.
Theme 3: High ‘telepresence’ and the negative impact on therapeutic alliance
The findings from this study imply the occurrence of ‘telepresence’ in CBT videoconferencing among patients and therapists. Telepresence is the sense that one is in the room with another and not in some remote location. If ‘telepresence’ was low, this lack of presence negatively impacted the therapeutic alliance (Bouchard et al., Reference Bouchard, Dumoulin, Michaud and Gougeon2011). Given that this study’s qualitative results suggest some evidence of telepresence and that most patients were satisfied with therapy, poor therapeutic alliance is unlikely; however, a standard measure of therapeutic alliance would be required in future studies.
There were some concerns around therapeutic alliance, despite positive experiences of telepresence. A few therapists felt that videoconferencing diminished the emotional part of re-living the memory during imagery rescripting. Most patients also described that CBT videoconferencing felt less personable, enabling poor communication and weaker therapeutic rapport. Therapists thought it was harder to read facial expressions, body language, and other subtle communications. The findings raise crucial questions about the impact of CBT videoconferencing on the therapeutic alliance, as a strong therapeutic alliance is often considered a pre-requisite for effective CBT (Robillard et al., Reference Robillard, Bouchard, Fournier and Renaud2003). Nonetheless, many studies have demonstrated that CBT videoconferencing has little impact on therapeutic alliance (Himle et al., Reference Himle, Fischer, Muroff, Van Etten, Lokers, Abelson and Hanna2006; Simpson and Reid, Reference Simpson and Reid2014). Furthermore, patients in the current study reported high satisfaction levels with videoconferencing therapy.
Theme 4: COVID-19 restrictions may positively influence patients’ and therapists’ attitudes towards CBT videoconferencing
At CADAT, the shift to remote working due to COVID-19 may have positively changed most patients’ and therapists’ attitudes. Both patients and therapists became more open to the idea of videoconferencing as their confidence increased. Many patients and therapists were sceptical beforehand and surprised by the experience being better than they initially thought. This is consistent with previous studies that demonstrated that therapists’ and patients’ views on videoconferencing tended to become positive after testing out and using videoconferencing (Aafjes-van Doorn et al., Reference Aafjes-van Doorn, Békés and Prout2020; Békés and Aafjes vanDoorn, Reference Békés and Aafjes vanDoorn2020; Connolly et al., Reference Connolly, Miller, Lindsay and Bauer2020). Consequently, patients and therapists showed a willingness to continue receiving and offering CBT videoconferencing beyond the pandemic.
Clinical implications
The results from this study have several clinical implications. First, the themes in this study imply a need to assess whether CBT videoconferencing is appropriate or not for the patient, even beyond the pandemic, and this would require training therapists in conducting CBT videoconferencing assessments. Assessment questions may address the study’s themes, the patient’s privacy at home, patient access to IT equipment and internet, the patients presenting psychological problem and their virtual suitability and more information about the home environment. Assessments may also address any concerns around therapeutic alliance, perhaps offering a combination of in-person and videoconferencing CBT.
In terms of technological issues, securing funding for costs to ensure high-quality broadband may be appropriate; however, some studies have demonstrated that successful psychological videoconferencing depends more on how therapists and patients adapt to technology rather than on solving technical issues (Békés and Aafjes vanDoorn, Reference Békés and Aafjes vanDoorn2020; Connolly et al., Reference Connolly, Miller, Lindsay and Bauer2020). Furthermore, increased online usage is likely to lead to more positive attitudes among therapists (Sharma, Reference Sharma2017) and fewer technical and implementation issues. Another consideration is that therapists will feel more confident and competent with usage and thus more likely to increase positive patient experiences. Therefore, encouraging patients to have a trial of sessions may lead to positive experiences and clinical results. Future therapist training in general videoconferencing may include how best to discuss the likelihood of technical issues with the patient before they arise and how best to adapt and overcome them when they occur.
Another clinical implication is that therapists need time and training to prepare creative BEs and exposure and response prevention (ERP)-based tasks, especially if patients are restricted to the home environment. Previous studies have also highlighted the importance of videoconferencing preparation (Fineberg et al., Reference Fineberg, Van Ameringen, Drummond, Hollander, Stein, Geller, Walitza, Pallanti, Pellegrini, Zohar, Rodriguez, Menchon, Morgado, Mpavaenda, Fontenelle, Feusner, Grassi, Lochner, Veltman and Dell’Osso2020; Himle et al., Reference Himle, Fischer, Muroff, Van Etten, Lokers, Abelson and Hanna2006). Therefore, therapist training, specifically how to optimise CBT techniques during videoconferencing, may be the solution.
Limitations and future research
There are some limitations to this study. The results should be approached with caution due to its descriptive nature; causality cannot be inferred. For example, although the results capture the subjective experience of therapists and patients that the COVID-19 lockdown restrictions were an influencing factor in their experiences of CBT videoconferencing, other factors such as general issues with videoconferencing may have also been in operation. The study also used purposive sampling, which may elicit researcher selection bias, potentially questioning the sample’s representativeness (Morgan et al., Reference Morgan, Patrick and Magaletta2008) and participant selection bias (Fowler, Reference Fowler2009). It may be that participants who chose to participate had positive experiences, therefore potentially misrepresenting those who did not.
Future research may include experimental studies capturing data relating to the themes in this study: therapeutic alliance, telepresence, and therapist and patient anxiety in using CBT videoconferencing. It is important to note that over a quarter of patients had an OCD diagnosis in this study, suggesting that other future research may include disorder-specific measures and comparison of change measures for specific disorders such as OCD. Additional future research is warranted to compare health outcomes of those using CBT videoconferencing, those receiving full CBT in person, and those receiving a combination of in-person and videoconferencing CBT.
Conclusion
Evidence suggests that integrated, collaborative care models, including videoconferencing, may effectively treat anxiety disorders (Aafjes-van Doorn et al., Reference Aafjes-van Doorn, Békés and Prout2020; Connolly et al., Reference Connolly, Miller, Lindsay and Bauer2020). However, few studies have explored both patient and therapist perspectives in using CBT videoconferencing. Therefore, this study sought insight into therapist and patient experiences of CBT videoconferencing.
The findings emphasise the importance of assessing for whom CBT videoconferencing is most suitable, training for therapists to optimise CBT techniques and the importance of privacy and telepresence during treatment sessions. This emphasis on providing training for therapists may help reduce stress and improve confidence and competence, leading to positive experiences for patients. Due to COVID-19, many mental health services have resorted to providing treatment through videoconferencing. Although initially, this method may be considered a less than ideal medium, it has created a positive change in attitude towards virtual treatments for both therapists and patients. In this discussion, the guidelines and ideas set out can inform protocol for specialist services such as CADAT to treat anxiety disorders.
Key practice points
-
(1) Specific CBT videoconferencing training for therapists is required, particularly for behavioural experiments and exposure-based tasks.
-
(2) Training for CBT videoconferencing assessments for therapists is necessary to ascertain whether CBT videoconferencing is appropriate for patients, incorporating questions based on the themes from this study.
-
(3) Technical and practical video conferencing training should be offered to therapists and patients; issues can be addressed in the first video conferencing session.
-
(4) Encouragement should be given for therapists and patients to use CBT videoconferencing; usage and practice often increase confidence and positive experiences.
-
(5) Offering a combination of in-person and videoconferencing CBT sessions may be beneficial.
Supplementary material
To view supplementary material for this article, please visit: https://doi.org/10.1017/S1754470X22000083
Data availability statement
The data that support the findings of this study are available from Southwark Directorate Information Governance Team at the South London and Maudsley NHS Foundation Trust (SLAM). Restrictions apply to the availability of these data, which were used under licence for this study. Data are available from the authors with the permission of Southwark Directorate Information Governance Team at SLAM.
Acknowledgements
We thank CADAT staff and patients who took part in this study. We are indebted to Mara Avramescu and Dr Terence Sergeant for their help in the content analysis.
Author contributions
Li-Ling Song: Conceptualization (equal), Data curation (lead), Formal analysis (lead), Investigation (lead), Methodology (lead), Project administration (lead), Resources (lead), Software (lead), Supervision-Supporting, Validation (lead), Visualization (lead), Writing – original draft (lead), Writing – review & editing (lead); Chloe Foster: Conceptualization (equal), Data curation (supporting), Formal analysis (supporting), Funding acquisition (lead), Investigation (supporting), Methodology (supporting), Project administration (supporting), Resources-Equal, Software (equal), Supervision (lead), Validation (supporting), Visualization (supporting), Writing – original draft (supporting), Writing – review & editing (supporting).
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
The authors declare none.
Ethical statements
This study received ethical approval from the Southwark Directorate Information Governance Team, the Clinical Director, and Head of Psychology and Psychotherapy for Southwark at the South London and Maudsley NHS Foundation Trust (SLAM). Researchers removed all personal identifying information to protect patients’ and therapists’ identities. In addition, the authors in the study have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the British Association of Behavioural and Cognitive Psychotherapy (BABCP) and the British Psychological Society.








Comments
No Comments have been published for this article.