Introduction
Background
Visual hallucinations (VH) are relatively common, with around 27% of individuals with a diagnosis of schizophrenia (Waters et al., Reference Waters, Collerton, Jardri, Pins, Dudley and Blom2014) reporting VH. The presence of VH is linked to increased disability and greater likelihood of in-patient status (Meuser, Bellack and Brady, Reference Mueser, Bellack and Brady1990; Waters et al., Reference Waters, Collerton, Jardri, Pins, Dudley and Blom2014). Given the prevalence, distress and impact of VH there is a need for effective treatments. However, there is an absence of evidence of specific benefit of medication for VH (Collerton, Mossimann and Perry, Reference Collerton, Mosimann and Perry2015) or for psychological therapies (Waters et al., Reference Waters, Collerton, Jardri, Pins, Dudley and Blom2014). There are a few case reports using cognitive behavioural therapy for psychosis (CBTp) (Callcott, Dudley, Standardt, Freeston and Turkington, Reference Callcott, Dudley, Standardt, Freeston, Turkington, Hagen, Turkington, Berge and Grawe2010; Hutton, Morrison and Taylor, Reference Hutton, Morrison and Taylor2012; O'Brien and Johns, Reference O'Brien and Johns2013). Whilst interesting as case studies, there is little in the reports to show that the VH specifically were targeted in treatment, and further evidence is required before it is possible to conclude that there is evidence of effective treatment for distressing VH.
Cognitive behavioural therapy for VH
Collerton and Dudley (Reference Collerton and Dudley2004) adapted the cognitive model of distressing auditory hallucinations (AH) (Morrison, Reference Morrison2001) to help understand and treat distressing VH. The key aspects of this model are that the person appraises a VH as a threat to their physical or psychological wellbeing (Gauntlett-Gilbert and Kuipers, Reference Gauntlett-Gilbert and Kuipers2003, Reference Gauntlett-Gilbert and Kuipers2005), which understandably leads to fear or anxiety, and in turn leads to the use of safety seeking behaviours (such as avoidance and escape) to prevent the feared outcome. This may inadvertently lead to the maintenance of the appraisal and the distress, as the person does not learn that they are actually safe and will not be hurt.
Some empirical support for the model exists (Dudley, Wood, Spencer, Brabban, Mossiman and Collerton, Reference Dudley, Wood, Spencer, Brabban, Mosimann and Collerton2012; Aynsworth, Nemat, Collerton, Smailes and Dudley, Reference Aynsworth, Nemat, Collerton, Smailes and Dudley2017b), and its treatment utility was considered in a multiple baseline single-case (n = 4) study of CBT for distressing VH (Wilson, Collerton, Freeston, Christodoulides and Dudley (Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016)). Single-case methods were used as they are ideally suited to novel treatment development. Where there is replication across cases there is greater confidence that the treatment is beneficial. Also, staggered baselines imply that it is the addition of the intervention, rather than external events or time alone, that accounts for change. Finally, single-case methods often use daily recording by the participant of key variables specified in the model (appraisals, emotional reactions and behaviours). This helps to determine if any change in the VH is associated with changes in theoretically important mediators. Hence, such approaches can inform not only if the treatment works, but can help identify the possible mechanism by which it works; the neglect of which is a criticism of the research on CBT for psychosis (Thomas, Reference Thomas2015). Wilson et al. (Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016) reported that the treatment was acceptable, and individuals who had good outcomes showed the expected change on appraisals of threat. However, the work was limited in terms of the therapy and methodology.
Limitations in therapy
(1) People were not only distressed about their VH owing to appraisals about harm, but in some cases because of the content of what they saw (i.e. gruesome and violent images) or the sheer persistence of the experience (‘it will go on for ever’, ‘I have no control’, etc.). Consequently, the impact of content and appraisals about persistence were incorporated into a revised model of VH in psychosis.
(2) The treatment offered in the study by Wilson et al. (Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016) was brief (8–10 sessions). Typically more sessions are required for this population (Rodriguez-Sanchez et al., Reference Rodriguez-Sanchez, Crespo-Facorro, Gonzalez-Blanch, Perez-Iglesias and Vazquez-Barquero2007; NICE, 2014). Hence a larger dose of treatment was offered in the revised treatment protocol.
Limitations in the methodology
(1) There is an absence of validated VH specific measures that are sensitive to change (Aynsworth, Collerton and Dudley, Reference McCarthy-Jones, Smailes, Corvin, Gill, Morris and Dinan2017a).
(2) A strength of single-case approaches is the use of daily recordings, but in Wilson et al. (Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016) there were difficulties in achieving baseline stability, which reduces confidence that any subsequent change was attributable to the treatment package. Hence, changes were made to increase the likelihood of establishing baseline stability. Improved methods to increase completion of the daily diary were also developed, through the use of a wage-payment model for participants in recognition of their efforts in completing the diaries.
(3) Improvements were also made to the sensitivity of the diary measure as Wilson et al. (Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016) reported it was difficult to identify subtle safety behaviours used in response to the VH, and these were not captured in the daily recordings. Hence changes were made to the process of eliciting behaviours for the diary, and to improve the understanding of the exact function of a behaviour during the early stages of diary recording (which helps establish it is a safety seeking behaviour).
To help address issues of design, measurement, intervention and statistical analysis the Clearing House Single-Case Design Technical Guidance (Kratochwill et al., Reference Kratochwill, Hitchcock, Horner, Levin, Odom, Rindskopf and Shadish2010) was used to ensure a standard of quality within the methodology.
Aims
The primary aims of this study were to:
-
(1) Examine the value of the refined CBT for VH treatment package in reducing the specific distress associated with experiencing VH.
-
(2) Consider in more detail patterns of variability in the baselines using more advanced methods of analysis, to help ensure stability is achieved prior to intervention phase, and is offered to help allow more meaningful conclusions to be made as to the value of treatment.
-
(3) Improve the sensitivity of standardized measures and diaries, improving specification of behaviours.
Method
Design
A multiple-baseline single-case design was used (Blampied, Reference Blampied1999). It consisted of baseline (A), intervention (CBT for VH) (B), and follow-up (C).
Baseline length
A minimum baseline period of 3 weeks (27 days) was set to ensure sufficient data points for each phase, and to improve the likelihood of capturing stable baseline data (Kratochwill et al., Reference Kratochwill, Hitchcock, Horner, Levin, Odom, Rindskopf and Shadish2010). To establish the presence of stability, the researcher considered variability, trend and cyclicity (Kratochwill et al., Reference Kratochwill, Hitchcock, Horner, Levin, Odom, Rindskopf and Shadish2010). Given that baseline data might have high variability (Wilson et al., Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016) rather than randomize the baseline length, sufficient time was allowed for stability to be achieved. Stability was established at different time points for each participant, leading to differing baseline lengths.
Participants
Six participants were approached, and five were recruited into the study. Four people completed the full treatment, while one person began therapy but disengaged. Participants were aged between 18 and 30 years and met the following criteria: aged over 18 years; currently experiencing psychosis of which distressing VHs were a predominant symptom; in receipt of care co-ordination from the Early Intervention in Psychosis (EIP) Service; has capacity to give informed consent and stable on medication for the last three months. Exclusion criteria were: reporting suicidal intention; dependent upon alcohol or other illegal substances; received psychological therapy within the last six months.
Participant details
Participant 1. Josh met criteria for psychotic disorder unspecified, and did not take medication. Josh reported VH since the age of 13. Josh described the main target VH for therapy as fantastical creatures such as gargoyles. The VH differed on each occasion. The presence of the VH left Josh feeling anxious and thinking ‘I'm losing control’. To cope, Josh would often distract himself. Following a baseline phase of 3 weeks, he received 13 sessions of CBT for VH, with one review session during the follow-up phase.
Participant 2. Sarah met criteria for paranoid schizophrenia, post-traumatic stress disorder and social anxiety. She had a clinical diagnosis of unspecified non-organic psychosis. She chose not to take medication. Sarah reported VH from the age of 14. The target VH was identified as a vision of an old woman. This VH often left Sarah feeling terrified, and although she was aware the VH was not a real person she worried that the VH ‘might hurt the people I love’. To manage, Sarah relied on avoidance behaviours. After a baseline phase of 4 weeks Sarah received four sessions of CBT for VH. At this point Sarah disengaged with therapy owing to health issues affecting a close family member.
Participant 3. Leanne met diagnostic criteria for paranoid schizophrenia and social anxiety. She was not prescribed medication. Leanne had been seeing VH for six months and experienced three different VH daily; all of which were insects or spiders. The main target VH was a talking insect. The presence of this VH caused Leanne to have the thought ‘I'm going crazy’, often leaving her feeling highly anxious. At times Leanne was talking back to the VH to manage her feelings of anxiety. Following a baseline phase of 4 weeks, Leanne received 16 sessions of CBT for the target VH. Following the CBT VH intervention, Leanne received additional therapy focusing on emotion regulation, and then a further six sessions of CBT for VH for a different target VH. Follow-up data were collected.
Participant 4. Andy met criteria for paranoid schizophrenia, previously having been diagnosed with emotionally unstable personality disorder. Andy was prescribed Olanzapine, and the dosage of this was increased during the initial-therapy phase. Andy reported VH from the age of 12. The target VH for therapy was a male figure that he saw daily. The presence of this VH often led to thoughts of ‘I'm going crazy’, which left Andy feeling anxious, and trying to distract himself. Andy completed a baseline phase of 4 weeks. Early in the intervention phase Andy had significant difficulties with managing feelings of anger, which led to a focus on risk assessment and anger management for the first eight sessions of therapy. This led to the addition of an extra phase in the design for this case. The VH focused intervention phase began from session 9, where Andy completed 12 sessions using a CBT for VH treatment approach. Andy was commenced on Clozapine medication and he and his family began concurrent family interventions in the latter phases of the VH treatment.
Participant 5. Lauren met criteria for paranoid schizophrenia and post-traumatic stress disorder. Lauren was prescribed Quetiapine, and was on a Methadone programme. Lauren had reported VH three years previously, which had lasted a year. However, the VH had recurred for the last six months. She experienced two types of VH daily (shadow creatures and moving objects). The main target VH was the moving objects which Lauren described as a disturbance within her visual field, with everything in her vision constantly moving. Her appraisal was she was ‘losing control’, and she felt stressed and overwhelmed. Often Lauren would close her eyes to cope with their presence. Following a baseline phase of 5 weeks, Lauren received 12 sessions of CBT for VH.
Measurements
Idiosyncratic measures to track daily change
An individual daily diary was the primary outcome measure for this study. To improve the specification of key appraisals and behaviours for the diary measure a newly developed workbook (based on the Distressing Visions Workbook, available on request from the corresponding author) and Appraisals and Reactions to Visual Hallucinations Interview; Dudley et al., Reference Dudley, Wood, Spencer, Brabban, Mosimann and Collerton2012) was used. A preliminary psychological formulation was developed by the researcher (C.T.) and a consultant clinical psychologist (D.C.) who was not involved in treatment but who has extensive experience of CBT and VH. The diary measure was then developed from the assessment information, the workbook and the formulation. The proposed diary was discussed with participants and amended in light of their feedback.
A numerical rating scale was agreed with participants (with four participants opting for a 0–10 scale, and one participant using a 0–5 scale) to capture daily ratings of conviction of appraisal, strength of affect, and use of safety behaviours. For the baseline phase, the researcher met weekly with participants to support use of the diary and to ensure the sensitivity and accuracy of the diary. All participants received daily text message reminders to complete their diary.
Standardized measures
The following measures were undertaken with participants by the researcher (C.T.), who was independent, but not blind, to the delivery of the treatment. Figure 1 outlines when each measure was completed.
Figure 1. Flow chart of the research procedure
North-East Visual Hallucinations Interview III (NEVHI) (Mosimann et al., Reference Mosimann, Collerton, Dudley, Meyer, Graham, Dean, Bearn, Killen, Dickinson, Clarke and McKeith2008). The revised version of the NEVHI (Mosimann et al., Reference Mosimann, Collerton, Dudley, Meyer, Graham, Dean, Bearn, Killen, Dickinson, Clarke and McKeith2008) was used to establish the presence of distressing VH, and to gather a detailed description of characteristics.
The Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID-I) (First et al., Reference First, Spitzer, Gibbon and Williams2007). This measure was administered to establish distressing or disabling psychosis features and to confirm diagnosis.
The following three measures were completed at each phase change (pre-baseline, pre-therapy, post-therapy, and follow-up):
The Psychotic Symptom Rating Scales (PSYRATS) (Haddock et al., Reference Haddock, McCarron, Tarrier and Faragher1999). The PSYRATS gathers details on the experiences of positive symptoms within psychosis (Haddock et al., Reference Haddock, McCarron, Tarrier and Faragher1999). As there is no equivalent measure for VH, the PSYRATS-VH scale was adapted and piloted by Wilson (2012). This measure was used to capture levels of distress associated with the VH at the start of the baseline phase, and then again at each phase change.
The Schizophrenia Change Scale (SCS). The SCS is a subscale of the Comprehensive Psychopathological Rating Scale (CPRS) (Montgomery et al., Reference Montgomery, Taylor and Montgomery1978). The SCS consists of 12 items that assess such things as sadness, disrupted thoughts, commenting voices, delusions, etc.
Work and Social Adjustment Scale (WSAS) (Mundt et al., 2002). This is a simple 5-item self-report measure, which assesses the impact of a person's mental health difficulties on their overall functioning.
Post-treatment interview
A semi-structured interview was used to capture the participants’ experiences of therapy, including acceptability, and any beneficial or adverse effects of treatment. It was based on The Change Interview (Elliot et al., Reference Elliot, Slatick and Urman2001) and the work of Wilson et al. (Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016). The interview was completed once at the end of the intervention phase.
Procedure
The procedure was similar to Wilson et al. (Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016) and is outlined in Fig. 1. Participants were recruited from EIP teams. The care team approached potential participants and gathered consent to be contacted. The researcher then contacted potential participants and collected consent to participate.
Participants were compensated for their time completing daily diary measures through a wage-payment model (Dickert and Grady, Reference Dickert and Grady1999). Compensation was provided in the form of gift vouchers for the calculated amount earned, and given to participants on a monthly basis.
Therapy intervention
Two therapists delivered the intervention (R.W. and R.D.). Both are clinical psychologists with postgraduate training in CBT and experience of working with individuals with psychosis. Audio-recorded therapy sessions and therapy record sheets were used alongside the Cognitive Therapy Scale-Revised (CTSR; Blackburn et al., Reference Blackburn, James, Milne, Baker, Standart, Garland and Reichelt2001) within regular supervision meetings to help ensure fidelity of treatment.
The CBT treatment package for VH was adapted to address the limitations identified in Wilson et al. (Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016). The target VH and associated appraisals are addressed using cognitive and behavioural approaches.
Ethical approval
A favourable ethical opinion was received from an NHS ethics committee, and the project was registered with the local NHS Trust Research and Development Department. All participants gave their informed consent for information to be included within the write-up of this study. To protect confidentiality, names and non-essential details have been changed or removed. All descriptions were shared with participants prior to write-up, and their feedback was incorporated into the final version.
Data analytic strategy
Visual analysis. Visual analysis is the main form of data analysis in single-case approaches. A formal visual inspection of the data was carried out by the researcher and an independent rater, both trainee clinical psychologists. The key factors, as defined by Kratochwill et al. (Reference Kratochwill, Hitchcock, Horner, Levin, Odom, Rindskopf and Shadish2010), were considered for each phase and phase change, with inter-rater agreement at 99%. Disagreements were resolved through discussion, and a consensus reached. Missing data are reported for each variable but were not replaced, as this may have distorted the visual analysis.
Statistical analysis. Where indicated by the data, Tau-U was the statistical method chosen to support the visual analysis. This method is based on the principals of non-overlapping data across phases, and was chosen as it is a robust method of analysis to control for baseline trend (Parker et al., Reference Parker, Vannest, Davis and Sauber2011). Tau-U values between 0.2 and 0.5 represent a small effect size; values between 0.5 and 0.8 are moderate to large (Galletta and Vogel-Eyny, Reference Galletta and Vogel-Eyny2015). An online calculator was used to determine Tau-U (Vannest et al., Reference Vannest, Parker and Gonen2011). The Tau-U statistic allows for a correction of baseline trend when this is indicated (details of this are provided in Parker et al., Reference Parker, Vannest, Davis and Sauber2011). This correction was applied using the online calculator when significant trend values were reported to be higher than 0.3, as this is the point at which trend is considered problematic (Parker et al., Reference Parker, Vannest, Davis and Sauber2011; Vannest and Ninci, Reference Vannest and Ninci2015).
Reliable and clinically significant change. The Leeds Reliable Index change calculator was used to calculate reliable (Morley and Dowzer, Reference Morley and Dowzer2014) and clinically significant change (Jacobson and Truax, Reference Jacobson and Truax1991) for the results of the standardized measures for each participant (accessed at: http://medhealth.leeds.ac.uk/info/2692/research/1826/research/2).
Results
Frequency
For Lauren, the shadow creatures VH, which were present daily during the baseline phase, showed a large decrease in frequency following intervention. Similarly, for Josh his VH were experienced on a weekly basis during the baseline phase. Following the introduction of the intervention the frequency reduced to between fortnightly and monthly. With two exceptions, from day 65 onwards the VH became non-existent. Both Lauren and Josh experienced this decrease in the frequency of their VH during therapy as an important and positive change. Table 1 shows frequency data for all participants.
Table 1. Frequency data

*Frequency = less than weekly.
Owing to low frequency reporting of the VH for Josh, and the VH (shadow creature) for Lauren, they are not included in the visual analysis.
Comparison across the majority of participants showed a similar process of change for appraisals (Fig. 2). Baseline data were stable for all participants, except Andy. Andy's data reached stability over the additional ‘stabilization’ phase included in his therapy. There was no significant trend in the baseline data for the majority of participants (p > .20.); however, Andy's baseline did show significant trend (Tau-U = –0.35, p < 0.02). This was corrected for using the Tau-U statistic.
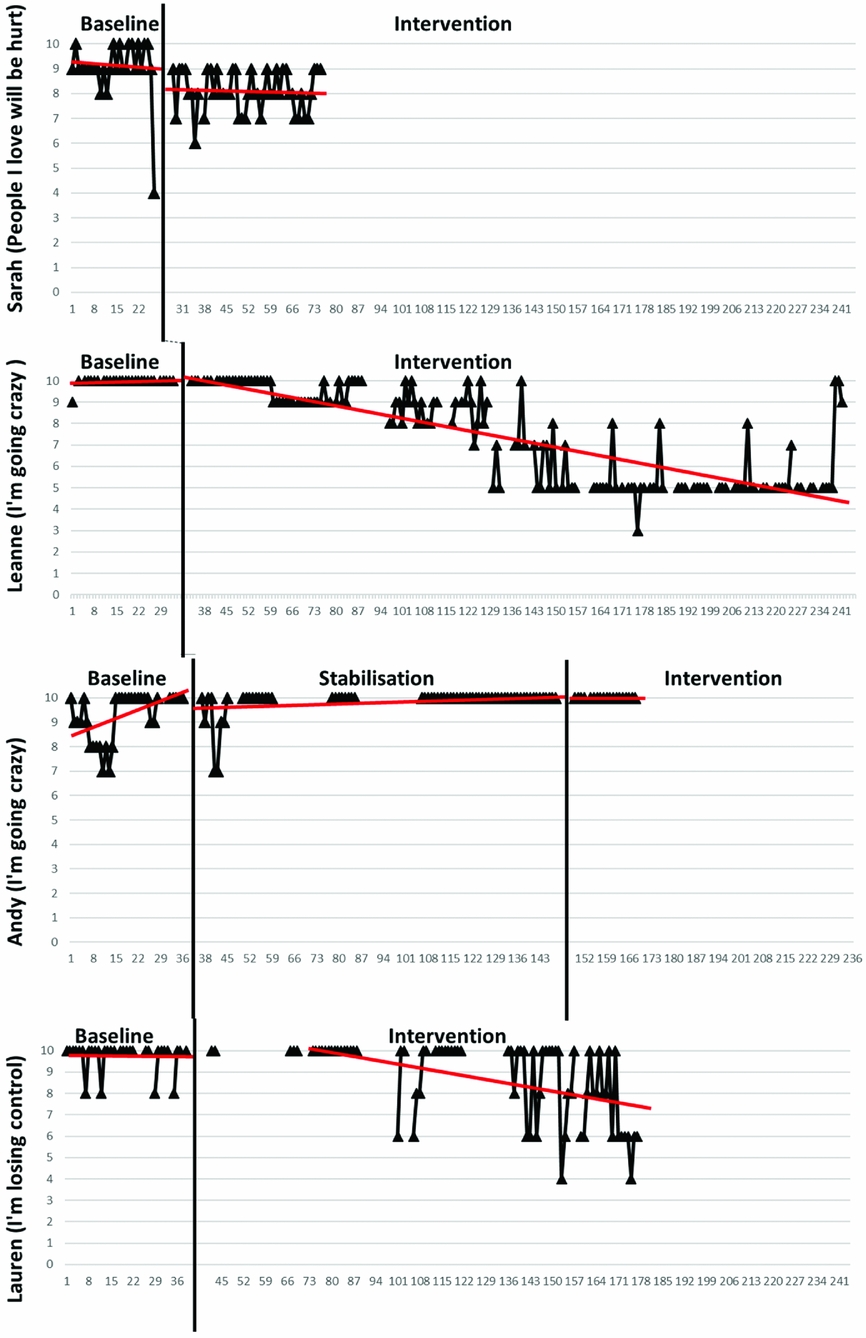
Figure 2. Appraisals
For the intervention data there is evidence of a gradual change in level, with a decreasing trend over a period of time in most cases. Sarah is an exception to this, in that a change in level happened more abruptly following the introduction of the intervention phase. The change in data pattern was significant across three cases (Table 2). Andy's data showed no significant change.
Table 2. Summary of Tau analysis for appraisals
*Significant change.
Comparison across the participants showed a slightly different process of change for affect (Fig. 3). Baseline data were again stable for all participants, except Andy. All participants showed higher variability in their level of affect than in their strength of appraisal. There was no significant trend in the baseline data for the majority of participants (p > .20.), except for Andy's data that had trend to a significant degree, which was corrected for in the intervention phase (Tau-U = –0.61, p < 0.0001). From discussion with Andy, it was felt that this might relate to him scoring the emotion of ‘anger’ very highly during the baseline period, which was a trigger for his VH experience, rather than a response to it. It took some time during the stabilization phase to support Andy in identifying the differences between these emotional responses, and this may account for the gradual increase in his recording of the emotion anxiety.
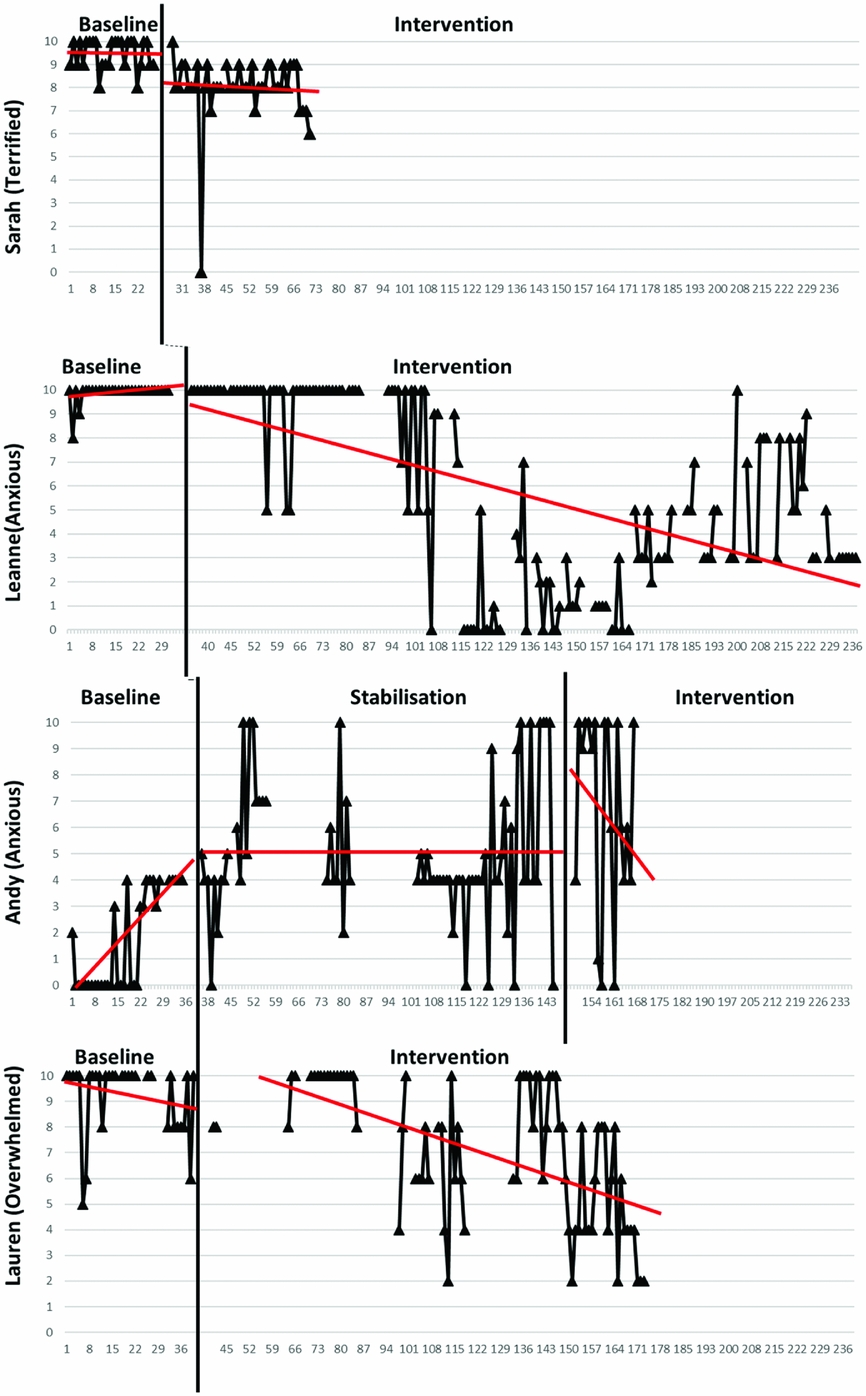
Figure 3. Affect
For the intervention data there is evidence of a gradual change in level, with a decreasing trend over a period of time in all cases. There is evidence of some variability within this trend in most cases. Again, Sarah is an exception to this, in that a change in level happened more abruptly following the introduction of the intervention phase. The change in data pattern was significant for Leanne, Sarah and Andy (Table 3). For Andy, however, affect increased from baseline. There was evidence of change for Lauren, but not to a significant degree.
Table 3. Summary of Tau analysis for affect
*Significant change; **baseline correction.
All cases show high variability and less stability in the baseline data for the behavioural domain, with a number of participants using this scale in a more categorical manner (Fig. 4). However, none of the cases showed trend to a significant level in the baseline phase (p > .20).
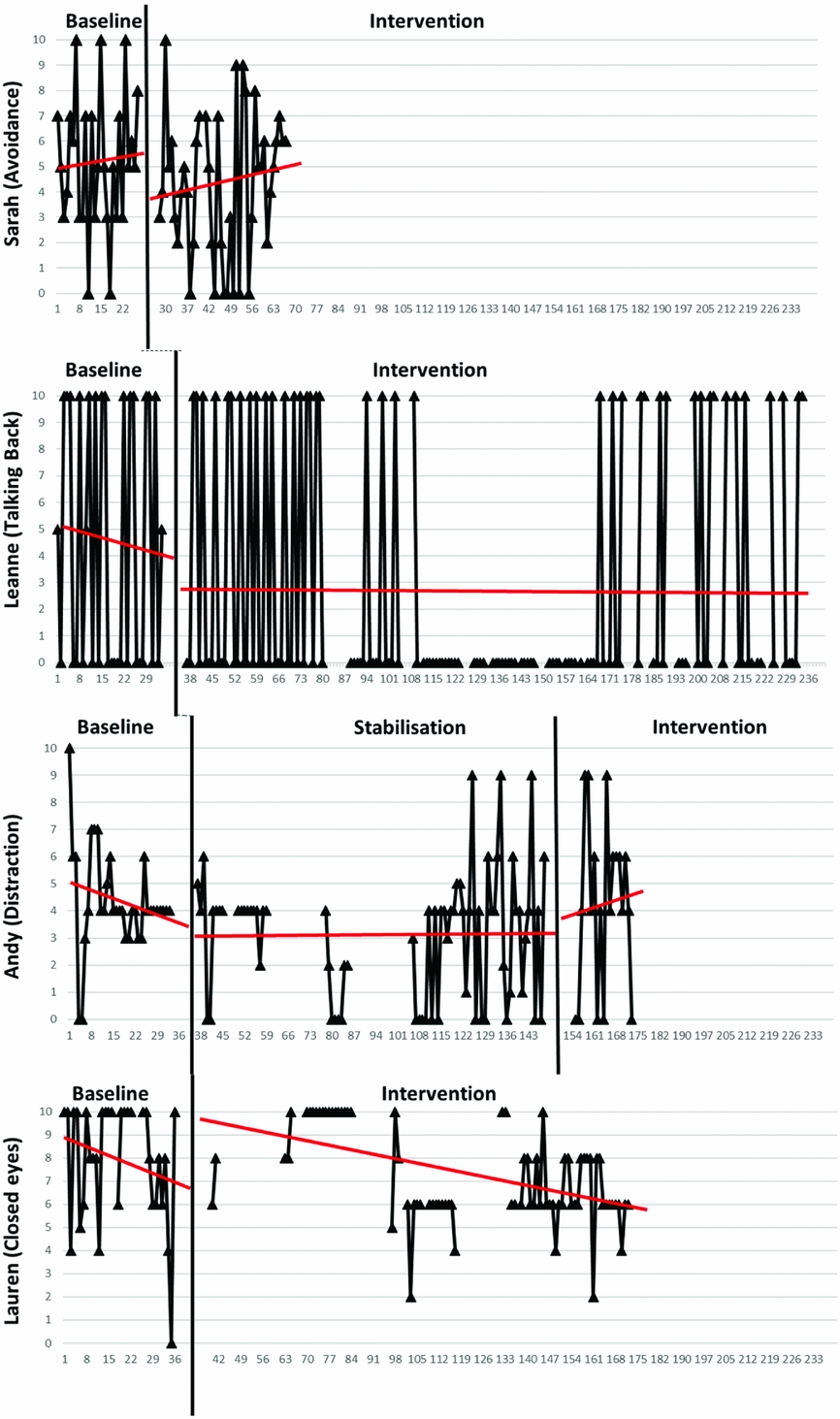
Figure 4. Behaviours
For the intervention phase the data remained variable for all participants, and the majority of participants showed no significant change in pattern (Table 4). The exception to this is Leanne, where there was a significant change observed, and which reflected a period of days where she stopped the behaviour entirely. Leanne felt that the graphs accurately captured her behaviour, and thought that the shift co-occurred with her being on holiday and the absence of an opportunity to be alone to ‘talk back’ to the VH. With highly variable data across all participants it is difficult to draw conclusions about change across the baseline and intervention phases.
Table 4. Summary of TAU analysis for behaviours
*Significant change.
Standardized measures
Table 5 displays the raw scores on the standardized measures and indicates whether clinically significant or reliable change was present. There was no significant change in the standardized measures during the baseline phase for any participant. For the majority of participants the change on standardized measures was not clinically significant or reliable. The only exception was for Lauren, who showed a significant change on the PSYRATS-VH measure. As Sarah did not continue with therapy there are no measures of reliable and clinically significant change to report for the intervention period.
Table 5. Raw scores for standardized measures
Phase A, initial baseline; phase B, pre-intervention; phase C, post-intervention.
Follow-up data were gathered from three of the participants who remained in the study. Sarah discontinued her involvement in the early stages of therapy and declined to give follow-up data. Lauren did not provide follow-up data.
The data gathered from Josh showed that his improvements were maintained across all measures following 1 month of no therapy. For Leanne, the results of the PSYRATS showed a return to baseline, but both the SCS and WSAS scores showed that results were maintained and continued to improve following the additional six sessions of therapy, but also following 1 month of no therapy. The follow-up data for Andy continues to show no change on any of the standardized measures.
Discussion
This study considered the process of change in the treatment of distressing VH. It addressed key limitations of a previous study (Wilson et al., Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016) in that the treatment was revised by considering the impact of the content of VH and their persistence, and the dose of treatment was increased. In addition, there were improvements to aspects of single-case design through close attention to ensuring baseline stability, as well as refinements to the diary measure and utilization of more advanced methods of analysis. There was also greater specification of safety behaviours including a detailed assessment at the beginning of treatment. These changes improved the quality of the single-case design methodology (Vohra et al., Reference Vohra, Shamseer, Sampson, Bukutu, Schmid and Tate2015; Tate et al., Reference Tate, Perdices, Rosenkoetter, Shadish, Vohra and Barlow2016).
The increased dose of treatment appeared to be acceptable with participants generally receiving between 12 and 16 sessions of CBT for VH. The results of the visual and statistical analysis indicate significant changes in the self-reported daily recordings of appraisal and affect in three participants. Two people reported reduced frequency of VH. Replication across cases, using multiple baselines, increases confidence that this change did not happen by time alone or by chance. Only one participant showed no beneficial change (Participant 4), which was also the case after he had been treated with Clozapine and engaged in family interventions. In contrast to the changes consistently observed in appraisal and affect, there was no evidence of change replicated within the behavioural domain.
The current treatment package appears to have a positive impact for most people experiencing distressing VH, and the change is consistent with theoretically important mediators. This suggests that targeting the specific VH symptom could be a useful approach (Freeman, Reference Freeman2007; McCarthy-Jones et al., Reference McCarthy-Jones, Trauer, Mackinnon, Sims, Thomas and Copolov2014). The results also indicate a link between reduction in distress and appraisal, with no case showing change in affect in the absence of change in conviction of appraisal. There is some evidence that frequency of VH may also be related to this process. Such changes have been shown in CBT for AH (Morrison et al., Reference Morrison, Turkington and Pyle2014), and would seem to support the CBT model of VH (Collerton and Dudley, Reference Collerton and Dudley2004). However, the positive findings from visual and statistical analysis of personal daily diary data were not reflected to a reliable or clinically significant level in the standardized measures. One case demonstrated change on the PSYRATS-VH measure, but this was where frequency of VH substantially reduced. This suggests the PSYRATS-VH may be sensitive to changes in frequency more than distress. It is also evident that there was not a change across non-targeted but related areas, such as voices, paranoia or mood (Joorman et al., Reference Joormann, Kosfelder and Schulte2005; Birchwood and Trower, Reference Birchwood and Trower2006). The findings of Wilson et al. (Reference Wilson, Collerton, Freeston, Christodoulides and Dudley2016) were similar in that there was not an apparent generalization of benefit to non-targeted symptoms, and such issues may need to be addressed separately.
It is also of interest that changes were not observed in the recorded behaviours. There are two likely explanations for this. First, it may be that this is related to a measurement issue in that behaviours are rated categorically (either present or not). Future studies need to consider alternative methods, such as activity monitors (Lyons et al., Reference Lyons, Lewis, Mayrsohn and Rowland2014), or behavioural analysis approaches such as frequency recording (Cooper et al., Reference Cooper, Heron and Heward2007), to monitor behaviours more objectively. A second issue is that the function of a behaviour may mean that its frequency is not the key issue. If a person copes with visions by avoiding going out, they may only need to avoid going out once a day, so frequency of a behaviour may be less directly related to the distress than appraisal. Methods to establish the purpose, and perceived importance of the behaviour may be more important than recording frequency.
Limitations
This is only the second single-case experimental design study evaluating the treatment of distressing VH in psychosis. Whilst these results encourage further refinement and testing of the treatment approach, a number of limitations need to be addressed. First, there is no immediate change in level or slope following the introduction of the intervention, which makes it more difficult to attribute change to this. However, this is not unexpected and is in line with our understanding of the processes of therapy (see Rachman, Reference Rachman1999) where change occurs incrementally.
Second, as discussed, changes were not observed in the recorded behaviours. It is possible that the improvements to the treatment package still do not fully address behavioural change.
The variability in the characteristics of the sample in terms of diagnoses, differences in the VH and the resultant distress and disability may make it difficult to characterize the target population. This may affect the generalizability of the findings. Of course, psychosis is a broad construct and even a diagnosis like schizophrenia has been critiqued as any two people with the diagnosis may have few if any symptoms/experiences in common. Hence, there is an issue about the generalizability of any investigation of treatments for psychosis and/or psychotic symptoms. However, all our participants experienced distressing VH and more broadly met entry criteria for EIP services that would encourage us to consider them as representative of the EIP population. In fact, we consider it unlikely that someone with such frequent and distressing visual hallucinations would be considered to have another non-psychotic disorder. Another factor that encourages us to think our work is generalizable is that we approached six service users and five agreed to participate. Given the high uptake it would encourage us to think that we were not seeing an unrepresentative sample of people in EIP services with distressing VH.
A final limitation is regarding Andy's participation, as the amount of VH treatment he actually received and the interpretation of the data are complicated by clinical need dictating changes to initial treatment focus, managing additional issues within therapy to support him, and adding concurrent treatment (medication and family therapy). We have retained Andy within the series to maintain transparency and reflect the realities of research within this population.
Future research
To further develop our understanding of the process of change, future single-case experimental designs may help demonstrate further replication across other centres and therapists (Horner and Kratochwill, Reference Horner and Kratochwill2012). Similarly, single-case methods used with VH could track appraisals not targeted in treatment to demonstrate specific change on theoretically important variables, and a lack of change on these non-targeted appraisals which would test further the model of VH. Of course, future research may consider evaluating CBT for VH in a larger trial that addresses whether treatment can be offered by other therapists to a wider population. For a larger trial of this nature, the development of a standardized and validated measure that is sensitive and specific to change in VH is needed to improve the likelihood of detecting meaningful clinical change.
Conclusions
We can conclude that CBT to manage distress associated with visual hallucinations shows promise as a potentially effective treatment. Further research is needed to refine its effectiveness and to show that it has delivered on that promise.
Main points
-
(1) Distressing visual hallucinations (VH) are a relatively common but often under recognized symptom of psychosis.
-
(2) VH seem to be associated with greater impairment and disability, but we have no specific treatment.
-
(3) Cognitive behavioural therapy for VH has shown some encouraging results, but is limited to case studies/case series.
-
(4) A refined cognitive behavioural therapy for VH was valuable in reducing distress, and in some cases reducing frequency of VH.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. It was completed as part of the Doctorate in Clinical Psychology educational degree.
Conflicts of interest
C.T. and M.F. have no conflicts of interest. R.D. has received royalties for books, or book chapters on the topic of cognitive therapy, and has received payment for leading workshops in cognitive therapy for visual hallucinations. R.W. has received payment for workshops in CBT for psychosis. D.C. is supported by a grant from the Great Britain Sasakawa Foundation.
Learning objectives
-
(1) To understand the prevalence, nature and impact of visual hallucinations for people in early intervention in psychosis services.
-
(2) To understand the role of appraisals and safety behaviour in the maintenance of distressing visual hallucinations.
-
(3) To understand how to utilize sophisticated single-case experimental designs to help investigate the process of change in targeted, symptoms-specific therapy.












Comments
No Comments have been published for this article.