Introduction
The majority of patellar dislocations occur in females, especially female adolescents, and the dislocation is most commonly lateral. The literature shows, depending on the study, that 30%–72% of patellar dislocations are trauma-related, especially during sports.Reference Tsai, Hsu and Hung 1
Knee flexion and valgus have been noted as the leading mechanisms of injury associated with patellar dislocation. This can be a result of powerful contraction of the quadriceps in combination with sudden flexion and external rotation of the tibia on the femur. Another mechanism is a direct trauma to the medial patella with the knee in flexion, forcing it laterally out of the femoral groove in which it rides.
The initial management of a first-time traumatic patellar dislocation is controversial, with no evidence-based consensus to guide decision-making. For acute patellar dislocation in children and adolescents, a 2008 study by Palmu et al demonstrated no improved long-term benefits to acute operative repair compared with non-operative management, and advocated against routine operative repair of the torn medial stabilizing soft tissues for the treatment of acute patellar dislocation in children and adolescents.Reference Palmu, Kallio and Donell 2
Traditional method of reducing lateral patellar dislocations
Patients often present with severe pain in the emergency department (ED) with their knee flexed and the patella displaced laterally. As with most dislocations, the longer the patella remains out of joint, the more swelling there will be in and around the joint, which makes reduction technically harder. Thus, the faster the patella can be reduced back into normal anatomical position, the better.
However, due to the severe pain associated with patellar dislocation, the reduction is done only after adequate procedural analgesia. This would usually take some time to organize, especially in busy EDs.
Analgesia can be effectively provided by giving nitrous oxide with oxygen; this can also allow sufficient procedural sedation for reduction of the patellar dislocation. This is usually done for the pediatric patients in the author’s ED. Reduction is achieved by pushing the dislocated patella medially with firm pressure, whilst extending the knee. As the leg extends, the patella under a medial stress will “pop” back into normal anatomical position.
Novel method of reducing acute lateral patellar dislocations
Many emergency physicians may have encountered patients with spontaneous reduction of patella dislocation even before coming into the ED. This novel method of patellar reduction utilizes the conditions for which these spontaneously self-reductions optimally occur. Atraumatic methods for reduction of joint dislocation, especially for the shoulder, have been well described, which use massage (Cunningham’s method) to relieve spasming muscles while keeping the optimal joint position for self-enlocation.Reference Cunningham 3
Based on the above principles, a novel method was conceived for reduction of lateral patellar dislocations. The technique is simple and involves massaging the mid to lower quadriceps muscles of the affected knee to relieve the spasm, whilst extending the knee very gently and slowly initially. The patella can usually be seen to be tracking medially back. When this occurs, extend the knee fully while continuing to massage the quadriceps. There is no actual direct manipulation of the patella required (see Figure 1).
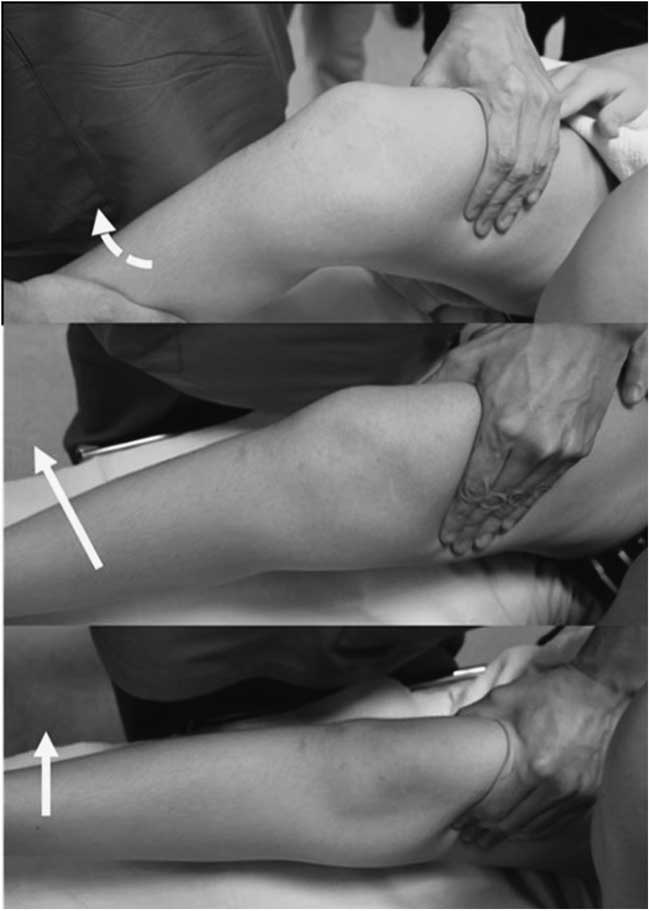
Figure 1 Step-wise pictorial demonstration of the novel method of patellar reduction.
Explain to the patients and family that the thigh muscle spasm may be relieved by simple massage, and that the painful knee will not be manipulated initially.
The knee and hip are usually held in flexion after a lateral patellar dislocation. Continuously massage the quadriceps whilst extending the knee very gently and slowly. The dislocated patella can be seen to be passively tracking medially when quadriceps spasm is relieved. Once this is achieved, fully extend the knee and hip to completely reduce the patella.
If the patella does not passively track medially during the massage of the quadriceps while gently extending the knee from its initial flexed position, do not forcefully extend the hip and knee fully. This might result in unnecessary pain. Provide the necessary analgesia and repeat.
Potential benefits of the novel method
Literature has shown that 25%–39% of lateral patellar dislocations are associated with osteochrondral fractures. However, magnetic resonance imaging and arthroscopic studies have reported that up to 95% of acute traumatic first-time lateral patellar dislocations were associated with osteochondral and/or chondral injuries (which may be subclinical).Reference Elias, White and Fithian 4 - Reference Mashoof, Scholl and Lahav 6
There are theoretical benefits to avoiding forceful manipulation of the dislocated patella during reduction, in terms of further trauma, pain and analgesia/sedation needed. This is especially the case when excessive force is used in the pediatric population, or reduction is done by inexperienced physicians. The objective of this study is to report a pilot study of five cases where the patellar dislocation was reduced employing this novel method of patellar relocation.
Methodology
A pilot study was carried out with five pediatric patients (less than 16 years of age; convenience population) who presented to KK Women’s and Children’s Hospital’s Children’s Emergency between January 1, 2014, and June 30, 2014, with first-time, acute traumatic lateral patellar dislocations. All five patients were managed using the novel method of patellar reduction as described above. Oral consent from parents and assent from the pediatric patients were obtained. All videography and/or photography were taken with signed parental consent (see supplementary material).
This specific population was chosen for the fact that patellar reduction for this group may potentially be technically more difficult, or may require greater force, compared with reducing a spontaneous or recurrent patellar dislocation.
Results
All five reductions were successfully performed in a single attempt by a single operator using the novel method as described above. See Table 1.
Table 1 Pediatric patient profile
Patient A had a significant medical history of Turner syndrome with hypothyroidism on thyroxine supplementation. She requires supervision for her activities of daily living due to neurocognitive delay and attends a special school. While she is fully self-ambulating without walking aids, she also has mild right hemiplegia (spastic) and a history of right tendo-archilles contracture, which was surgically lengthened at 9 years of age. The patient’s right hemiplegia, while mild, could have potentially decreased the rate of success of this novel method, but the reduction was uneventful and unexpectedly took less than a minute.
Patients C and D were in severe pain and were in extreme distress at presentation at the ED. Intranasal fentanyl was thus given for their extreme pain at presentation, after which they were able to calm down enough to allow for discussion and consent for the new method of patellar reduction. The reductions themselves did not require further analgesia and took less than a minute.
All the patients and their families were positive about their experience and all were discharged promptly from the ED after appropriate radiological investigations and ED management with outpatient orthopaedic follow-up.
Discussion
This novel method appears to be a useful single-operator method that delivers an atraumatic patellar reduction. Theoretically, this new patellar reduction technique should also be applicable for non-traumatic, spontaneous and/or recurrent patellar dislocations in children and adolescents, as these tend to be easier to reduce.
While there need to be larger trials for comparative analgesia requirements for this novel method versus the traditional method, the investigators were able to successfully reduce the majority of the patellar dislocations with minimal analgesia in these five cases. With potentially less need for analgesia and sedation, this method may be especially advantageous in non-hospital environments or when medical attention may be significantly delayed.
Although it cannot be proven that this method is superior until further studies are done, this technique may serve as an alternative to the traditional method of patellar reduction, especially for pediatric patients. Validation of this technique is required on a larger scale to ascertain reproducibility of success rates. It also remains to be seen if this novel method is useful for adults.
Acknowledgment
The author would like to thank and acknowledge the invaluable contribution of Dr. Suraj Manickam, who assisted in the pilot study and assisted in recruiting patients and performing the procedure, and who took the photographic and videographic documentation of the procedure.
Competing Interests: None to declare.
Supplementary material
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/cem.2015.7






