Introduction
After the first case of the coronavirus was identified in Wuhan (People's Republic of China) in December 2019, the virus spread very quickly across the globe and led to the ongoing COVID-19 pandemic. In Germany, the first laboratory-confirmed case of the coronavirus was reported on 28 January 2020 (Robert Koch-Institut, 2020). Between then and the spring of 2022, Germany underwent five waves of the pandemic (Tagesspiegel Innovation Lab, 2022). During the first wave of the pandemic, the German government implemented social distancing and contact restriction measures, issued stay-at-home orders and ordered the closure of non-essential businesses starting in late March 2020 in order to slow down the spread of the virus. Compared to other countries, the containment and closure measures at the beginning of the pandemic were implemented both later and more slowly. Moreover, they were less restrictive than in other countries (Capano et al., Reference Capano, Howlett, Jarvis, Ramesh and Goyal2020). Nevertheless, the measures were socially disruptive, contributing to increased loneliness, impacts on mental health and lower levels of (domain) life satisfaction (Entringer et al., Reference Entringer, Kröger, Schupp, Kühne, Liebig, Goebel, Grabka, Graeber, Kroh and Schröder2020; Huebener et al., Reference Huebener, Spieß, Siegel and Wagner2020; Huxhold and Tesch-Römer, Reference Huxhold and Tesch-Römer2021; Möhring et al., Reference Möhring, Naumann, Reifenscheid, Wenz, Rettig, Krieger, Friedel, Finkel, Cornesse and Blom2021).
Relying on the existing literature, there are a number of reasons to assume that the wellbeing of individuals with support or care responsibilities for persons suffering from poor health, disability or age-related frailty (‘family care-givers’ in the following) was disproportionately affected by the COVID-19 pandemic. Even in non-pandemic times, studies confirm the assumptions underlying the care-giver stress process model (Pearlin et al., Reference Pearlin, Mullan, Semple and Skaff1990) by showing that family care-giving is a persistent cause of stress leading to negative wellbeing outcomes (e.g. Hirst, Reference Hirst2005; Hansen et al., Reference Hansen, Slagsvold and Ingebretsen2013; Kaschowitz and Brandt, Reference Kaschowitz and Brandt2017; Sacco et al., Reference Sacco, König, Westerlund and Platts2022). Specifically in Germany, which is often considered to have an ‘explicitly familialistic’ care regime, family care-givers are at the centre of maintaining the health and wellbeing of individuals in need of care (Leitner, Reference Leitner, Obinger and Schmidt2019; Fischer et al., Reference Fischer, Frisina Doetter and Rothgang2022). About 80 per cent of the 4.1 million individuals who are recognised as requiring care by the German long-term care insurance are cared for in their home environment (Statistisches Bundesamt (Destatis), 2020). Additionally, there is an undefined number of persons who are not (yet) recognised as care-dependent by the long-term care insurance but need regular support, help and care, which is most likely provided by their families, friends or neighbours (Geyer and Schulz, Reference Geyer and Schulz2014).
As the pandemic hit Germany in early 2020, many family care-givers experienced mounting family care responsibilities due to decreasing levels of support from professional care services and family, friends and neighbours (Eggert et al., Reference Eggert, Teubner, Budnick, Gellert and Kuhlmey2020; Brandt et al., Reference Brandt, Garten, Grates, Kaschowitz, Quashie and Schmitz2021; Klaus and Ehrlich, Reference Klaus and Ehrlich2021). Compared to 2019, family care-givers in 2020 used far fewer professional care services like day and night care (Tages- und Nachtpflege) and short-term care services (Kurzzeitpflege) (Bundesministerium für Gesundheit (BMG), 2021a, 2021b).Footnote 1 This is not surprising because the availability of many care facilities and services was not assured, or was considered unsafe with regard to the infection risk (Rothgang et al., Reference Rothgang, Wolf-Ostermann, Domhoff, Friedrich, Heinze, Preuss, Schmidt, Seibert and Stolle2020; Robert Koch-Institut, 2021). Additionally, family care-givers experienced less support due to the pandemic-related departure of paid 24-hour migrant home care workers (so-called foreign ‘live-ins’) (Eggert et al., Reference Eggert, Teubner, Budnick, Gellert and Kuhlmey2020; Wolf-Ostermann et al., Reference Wolf-Ostermann, Rothgang, Domhoff, Friedrich, Heinze, Preuß, Schmidt, Seibert and Stolle2020). Furthermore, in order to minimise the risk of infection for care receivers as well as for themselves, many family care-givers may have been reluctant to make use of support from family, friends and neighbours (e.g. Gilligan et al., Reference Gilligan, Suitor, Rurka and Silverstein2020). As a result, family care-givers found themselves in a new situation with less support from professional and privately provided care (e.g. Eggert et al., Reference Eggert, Teubner, Budnick, Gellert and Kuhlmey2020), which might aggravate the stress process and worsen family care-givers' mental health.
Another important aspect concerns family care-givers' social isolation. Although the entire population was called upon to distance themselves socially in order to contain the spread of the virus, family care-givers may have put even stronger social distancing measures in place: they needed to protect themselves from infection at a much higher level, not only to avoid putting their role as care-giver at risk but also to avoid passing the virus on to their family members who were in need of care and prone to infection. This protection was best ensured through strict social isolation of both the family care-giver and the person in need of care. Moreover, family care-givers may have maintained social isolation for health and safety reasons, even as the government eased contact restrictions after the peak of each wave of the pandemic (e.g. Gilligan et al., Reference Gilligan, Suitor, Rurka and Silverstein2020). This may have led to higher levels of loneliness among family care-givers than among non-care-givers.
As of May 2022, the impact of COVID-19 on family care-givers' wellbeing as compared to non-care-givers' wellbeing in Germany has not been systematically examined. Previous research was not able to identify a COVID-19 effect in the relationship between family care and wellbeing as it conducted analyses only on the basis of cross-sectional research designs, carer-only samples or non-probability samples (e.g. Eggert et al., Reference Eggert, Teubner, Budnick, Gellert and Kuhlmey2020; Wolf-Ostermann et al., Reference Wolf-Ostermann, Rothgang, Domhoff, Friedrich, Heinze, Preuß, Schmidt, Seibert and Stolle2020; Brandt et al., Reference Brandt, Garten, Grates, Kaschowitz, Quashie and Schmitz2021; Budnick et al., Reference Budnick, Hering, Eggert, Teubner, Suhr, Kuhlmey and Gellert2021). In order to analyse the impact of the COVID-19 pandemic on the relationship between family care and wellbeing, we draw on unique longitudinal and population-based data from the German Ageing Survey (DEAS). We contrast possible changes in family care-givers' and non-care-givers' wellbeing, i.e. general life satisfaction, depressive symptoms and perceived loneliness, between pre-pandemic (2017) and early pandemic times (June/July 2020). In June 2020, infection numbers were low, contact restrictions were comprehensively relaxed, and schools, kindergartens, museums, sports facilities and non-essential businesses re-opened under specific hygiene, physical distancing and/or contact tracing regulations (Bauer and Weber, Reference Bauer and Weber2021). At the same time, the perceived risk of infection for older or care-dependent people was still noticeable (Eggert et al., Reference Eggert, Teubner, Budnick, Gellert and Kuhlmey2020; Wettstein et al., Reference Wettstein, Vogel, Nowossadeck, Spuling and Tesch-Römer2020). At this point, the prospects for a vaccine were still remote and many experts stated that the pandemic was far from over. Therefore, we assume that the COVID-19 pandemic still posed an extraordinary burden on family care-givers at that time that translated into a worsening of their mental wellbeing. More specifically, we expect that as a consequence of the pandemic, loneliness and depressive symptoms of family care-givers have increased, and that their life satisfaction has declined to a greater extent than among non-care-givers. We conduct analyses by means of the first-difference regression technique. We are thereby able to identify the causal effect of the early COVID-19 pandemic and its associated containment and closure measures on individuals' mental wellbeing.
Method
Data
We employ panel data from the DEAS, provided by the German Centre of Gerontology (DZA) (Klaus et al., Reference Klaus, Engstler, Mahne, Wolff, Simonson, Wurm and Tesch-Römer2017). DEAS is a representative panel study (1996, 2002, 2008, 2011, 2014, 2017, 2020) of more than 20,000 adults aged 40 years and older living in private households in Germany. The DEAS is an excellent data source for analysing whether and to what extent the COVID-19 pandemic has impacted family care-givers' wellbeing as it provides rich longitudinal information on respondents' mental wellbeing, their family care-giver status and on other relevant confounders. Significantly, the 2020 survey took place in the period from 8 June to 22 July 2020. Although the first COVID-19 wave in Germany had flattened out at this time and some containment and closure measures had already been suspended, the feeling of threat and uncertainty in relation to the pandemic was still widespread, both subjectively and objectively, as the pandemic was not yet under control. As the start of the DEAS 2020 data collection by means of a sequential mixed-mode design combining a personal computer-assisted interview and an additional self-administered questionnaire (distributed in person) was suspended due to the unfolding COVID-19 outbreak, the DEAS team set up a special self-administered questionnaire (distributed by mail) in order to gather at least some information on its panel respondents' life circumstances during the pandemic (Engstler and Köhler, Reference Engstler and Köhler2021). This questionnaire collected data on the same topics as the regular DEAS, albeit in a shortened way. It also included specific questions on the COVID-19 pandemic.Footnote 2
Sample
This study employs data from 2017 and 2020 in order to analyse the impact of the COVID-19-related consequences on the wellbeing of family care-givers. Originally, the two DEAS waves contained 11,449 observations from 7,221 respondents. Respondents with missing information on the most important independent variable – family care – were excluded (n = 98). Respondents in each sample who were observed only once were also excluded (n = 3,248). The final balanced sample consists of 7,750 observations from 3,875 respondents.Footnote 3
The study's sample consists of four groups of (non-)care-givers. Family care-giving was captured via the following survey question: ‘In the last 12 months (2017)/in the last 3 months (2020), were there any people you regularly looked after or cared for on a private or voluntary basis due to their poor health?’ Those responding with ‘Yes’ were identified as family care-givers and those who responded with ‘No’ were identified as non-care-givers. However, as previous research suggests, the dynamics of family care (non-)provision should be taken into account more precisely as the relationship between family care and wellbeing can be different for those taking up, continuing or ceasing to provide family care (e.g. Hirst, Reference Hirst2005; Rafnsson et al., Reference Rafnsson, Shankar and Steptoe2017; Sacco et al., Reference Sacco, König, Westerlund and Platts2022; Gerlich and Wolbring, Reference Gerlich and Wolbring2021). Accordingly, for the purpose of this study, sample respondents responding with ‘Yes’ to the family care survey question in both years of a sample's observation were identified as ‘continuous care-givers’ (6.7% of the sample); those responding with ‘No’ in 2017 but with ‘Yes’ in 2020 were identified as ‘new care-givers’ (9.7% of the sample); those responding with ‘Yes’ in 2017 and with ‘No’ in 2020 were identified as ‘past care-givers’ (10.9% of the sample) and those responding with ‘No’ in both survey years were identified as non-care-givers (72.7% of the sample). Sample members were 66.5 years old on average (standard deviation (SD) = 10.2, range = 43–97 years) (in 2017), and 50.0 per cent were female.
For the purpose of performing further robustness checks, we constructed an additional balanced panel for the survey years 2014 and 2017 using an identical procedure resulting in 12,236 observations from 6,118 respondents.
Measures
Dependent variables
Life satisfaction information is based on the five-item Satisfaction With Life Scale (Pavot and Diener, Reference Pavot and Diener1993). Respondents rate statements such as ‘In most ways my life is close to my ideal’ or ‘If I could live my life over, I would change almost nothing’ on a five-point scale from (1) ‘strongly disagree’ to (5) ‘strongly agree’. The scale value is the mean of the five items (mean2017 = 3.89, SD2017 = 0.68; mean2020 = 3.88, SD2020 = 0.69). A higher scale value indicates a higher life satisfaction.
Depressive symptoms were captured on the basis of nine items (e.g. ‘During the past week I could not get going’) retrieved from the Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, Reference Radloff1977).Footnote 4 Respondents rated statements on a four-point scale from (1) ‘rarely or none of the time (less than 1 day)’ to (4) ‘most or all of the time (5–7 days)’. Two items worded in a positive manner were reversed. A total score ranging from 9 to 36 is calculated by adding together individual item scores (mean2017 = 13.81, SD2017 = 4.09; mean2020 = 15.56, SD2020 = 4.28), with higher scores indicating greater levels of depressive symptoms.
Loneliness is captured by the six-item De Jong Gierveld short scale for loneliness (De Jong Gierveld and van Tilburg, Reference De Jong Gierveld and van Tilburg2006). Items such as ‘There are enough people I feel close to’ or ‘I miss having a sense of security and warmth’ were rated on a four-point scale from (1) ‘strongly agree’ to (4) ‘strongly disagree’. Three items worded in a negative manner were reversed. A mean score is computed, with higher values indicating more loneliness (mean2017 = 1.73, SD2017 = 0.53; mean2020 = 1.87, SD2020 = 0.53). For a list of all items used as indicators for life satisfaction, depressive symptoms and loneliness, as well as further operationalisation details, see Appendix Table A1.
Covariates
As control variables, we take into account changes in respondents' labour market participation (employed or not), partnership status (partner or not), the number of household members and disposable household income. Table 1 includes descriptive statistics for all variables. Appendix Table A2 does so for the additional sample used in the robustness checks.
Table 1. Descriptive statistics of the study variables by survey year

Notes: Variables with missing information: life satisfaction (3.7%), depression (2.1%), loneliness (4.5%), employed (0.9%), partner (1.0%), household size (1.9%), household income (5.4%). SD: standard deviation.
Source: German Ageing Survey (DEAS), 2017–2020.
Analytical strategy
We perform linear first-difference regressions to identify changes over time and in family care-givers' wellbeing. First-difference models focus on the change in an outcome between two time-points (2017 and 2020) disregarding the level of that outcome. Applied to our case, we examine changes in the wellbeing indicators within the same person over time. All observed and unobserved stable characteristics of that person, such as gender, education or personality, are controlled for and do not distort our results (Allison, Reference Allison2009). The COVID-19 pandemic can be considered an exogenous treatment as it was not possible for individuals to self-select into or out of the lockdown scenario. Therefore, we are able to examine causal effects of the pandemic and the containment as well as closure measures on individuals' wellbeing. Moreover, during the pandemic the choice between family care and professional (full-time) care services was more restricted than in pre-COVID-19 times due to the limited capacities of professional care providers. Therefore, we are dealing with a much more significant exogenous shock than in other pre-crisis studies of family care. We include a binary variable for time that codes with 1 for the year 2020 in the regression models to capture the changes between 2017 and 2020 (Möhring et al., Reference Möhring, Naumann, Reifenscheid, Wenz, Rettig, Krieger, Friedel, Finkel, Cornesse and Blom2021). We include interaction effects of this variable with the care-giver status in order to identify differences in effects between the non-care-giving population and the three groups of care-givers (continuous, new and past).
In order to ensure that the changes we observe in the wellbeing of family care-givers are driven by the COVID-19 pandemic and are not to the result of general changes over time, we conducted additional first-difference regressions for the balanced panel of 2014 and 2017. The regression models were identical with respect to the dependent and most of the independent and control variables. Instead of a time-point variable for 2020, we included a time-point variable for 2017 to capture changes between 2014 and 2017. All estimations were performed with Stata 15.0.Footnote 5
Results
Table 2 shows selected results from the first-difference regressions of our three wellbeing indicators and Appendix Table A3 includes the full regression results. For the non-care-givers, we find significant changes in depressive symptoms and loneliness between 2017 and 2020, while life satisfaction did not change significantly between the two time-points. Compared to 2017, their depressive symptoms increased by 1.801 scale points (p = 0.000) on the scale from 9 to 36, and loneliness by 0.128 scale points (p = 0.000) on a scale ranging from 1 to 4.
Table 2. First-difference regression models on three aspects of wellbeing
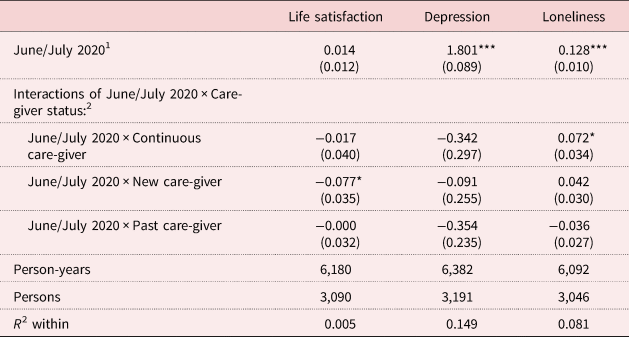
Notes: Controlling for labour market participation, partnership status, number of household members, household income. Standard errors are in parentheses. 1. The time-point dummy reflects the changes in each wellbeing indicator between 2017 and 2020. Due to our modelling strategy, the main effect shows these changes for non-care-givers. 2. The interaction effects of different types of family care-givers with the 2020 time-point dummy reflect the difference in the change for the respective care-giver type compared to non-care-givers.
Source: German Ageing Survey (DEAS), 2017–2020.
Significance levels: * p < 0.05, *** p < 0.001.
The interaction effects of family care-giver types with the 2020 time-point variable indicate that changes in wellbeing significantly differed for some care-givers compared to non-care-givers. This applies to life satisfaction of new care-givers and feelings of loneliness of continuous care-givers. Taking up a caring responsibility between 2017 and 2020 is associated with a decrease in life satisfaction by 0.077 scale points (p = 0.030). The change in feelings of loneliness is 0.072 scale points (p = 0.035) higher among continuous care-givers compared to the change in scale points observed among non-care-givers.
The additional first-difference regressions for the balanced panel of 2014 and 2017 yield no significant changes of the 2017 time-point dummy on the three wellbeing indicators under study (Appendix Table A4). However, those who took up a caring responsibility in the sample period 2014–2017 showed a significant increase in depressive symptoms. Together with the result on the significant decline in life satisfaction among new care-givers between 2017 and 2020, this finding indicates that the impairment of new care-givers' wellbeing does not represent a period effect but stems from the new care provision situation. Furthermore, the non-significant time-point dummies in the robustness checks indicate that the significant changes we observed in depressive symptoms (‘June/July 2020’ time-point dummy) and loneliness (‘June/July 2020’ time-point dummy, ‘June/July 2020 × Continuous care-giver’ interaction) between 2017 and 2020 among (non-)care-givers represent a period effect, i.e. an effect of the COVID-19 pandemic and its subsequent containment and closure measures.
Discussion and conclusion
In this study, we examined the impact of the COVID-19 pandemic and its related containment and closure measures on three wellbeing indicators among different groups of family care-givers and non-care-givers. Our data cover June and July 2020, when infection rates in Germany were low and most of the COVID-19 restrictions were eased. However, the perceived risk of infection and serious illness for people with pre-existing medical conditions and/or for people aged 60 and above was still high at this time, and prospects for a vaccine were still remote. Using a longitudinal first-difference design combining the 2020 information with data for 2017, we show, first, that differentiating between distinct wellbeing indicators and different groups of family care-givers is crucial when analysing the impact of the COVID-19 pandemic on individuals' wellbeing. Second, we demonstrate that (non-)care-giving adults living in private households in Germany experienced a decrease in specific wellbeing dimensions during the pandemic, and that this decrease was more pronounced for family care-givers – depending on the duration of care-giving and the wellbeing dimension under study.
We found that loneliness increased for (non-)care-giving adults during the COVID-19 pandemic. This finding is consistent with prior research that shows increased levels of loneliness due to the pandemic among the overall population in Germany (Entringer et al., Reference Entringer, Kröger, Schupp, Kühne, Liebig, Goebel, Grabka, Graeber, Kroh and Schröder2020; Huxhold and Tesch-Römer, Reference Huxhold and Tesch-Römer2021). In addition, we showed that the increase in loneliness was even more pronounced for continuous family care-givers than for the non-care-giving population. Although this difference is rather moderate, this finding suggests that continuous family care-givers might have adhered more strictly to social distancing measures than non-care-givers as they needed to protect themselves as well as their care receivers from infection much more strictly, ultimately leading to a higher increase in loneliness. Furthermore, the result also suggests that the care situation of continuous care-givers during the COVID-19 pandemic is very different from that of new care-givers (past care-givers, respectively), who did not differ significantly from the non-care-giving population with regard to changes in loneliness: continuous care-givers' care recipients are likely to have a longer history of illness and thus a worse health status on average than new care-givers' care recipients (e.g. Rothgang et al., Reference Rothgang, Kalwitzki, Müller, Runte and Unger2016; Rothgang and Müller Reference Rothgang and Müller2021). Therefore, continuous care-givers' care recipients might even be more vulnerable, which is why continuous care-givers probably apply stricter social distancing measures during the COVID-19 pandemic than new care-givers (past care-givers, respectively).
We found an increase in depressive symptoms resulting from the COVID-19 pandemic among (non-)care-giving adults. This finding broadly supports the results of other studies that observed an increased level of depressive symptoms in the early stages of the pandemic among the overall population (Entringer et al., Reference Entringer, Kröger, Schupp, Kühne, Liebig, Goebel, Grabka, Graeber, Kroh and Schröder2020; Mata et al., Reference Mata, Wenz, Rettig, Reifenscheid, Möhring, Krieger, Friedel, Fikel, Cornesse and Blom2021; Wettstein et al., Reference Wettstein, Nowossadeck and Vogel2021). However, for the specific group of family care-givers, the COVID-19 pandemic did not play out as an additional risk factor with regard to their psychological health, i.e. depressive symptoms, as we did not detect any significant differences between family care-givers and the non-care-giving population. Although prior research has shown that family care provision is a consistent source of stress resulting in increasing depressive symptoms (e.g. Pinquart and Sörensen, Reference Pinquart and Sörensen2003; Hansen et al., Reference Hansen, Slagsvold and Ingebretsen2013; Hiel et al., Reference Hiel, Beenackers, Renders, Robroek, Burdorf and Croezen2015; Kaschowitz and Brandt, Reference Kaschowitz and Brandt2017; Kaufman et al., Reference Kaufman, Lee, Vaughon, Unuigbe and Gallo2019; Kaschowitz and Lazarevic, Reference Kaschowitz and Lazarevic2020), the COVID-19 pandemic did not aggravate depressive symptoms to a greater extent among family care-givers than among non-care-givers. This rather unexpected finding might be due to this study's broad definition of family care provision. The family care measure does not presuppose, for example, a certain temporal involvement in family care tasks. Family care-givers in this study meet the requirement of having regularly looked after or cared for a person suffering from poor health on a private or voluntary basis over the last 12 months (2017)/3 months (2020). Accordingly, family care-givers included in this study may vary greatly in the extent of support and/or care provided: from care-givers helping with household chores or grocery shopping every second or third week or on weekends only to care-givers providing intensive care for several hours each day. Thus, our study rather provides a lower bound of effects of the COVID-19 pandemic on family care-givers' depressive symptoms because pandemic-induced changes (e.g. reduction of informal as well as formal support, possibly stricter self-imposed social isolation, possibly more negative appraisal of the pandemic as threat) may have a greater impact on intensive care-givers' depressive symptoms.
Our results showed further that the COVID-19 pandemic did not lead to significant changes in non-care-givers', continuous and past care-givers' life satisfaction. This finding corresponds with existing research showing that life satisfaction did not decrease substantially in the early phase of the pandemic among the overall population in Germany (Entringer et al., Reference Entringer, Kröger, Schupp, Kühne, Liebig, Goebel, Grabka, Graeber, Kroh and Schröder2020; Huebener et al., Reference Huebener, Spieß, Siegel and Wagner2020; Wettstein et al., Reference Wettstein, Nowossadeck and Vogel2021). However, we did find a decrease in life satisfaction for new care-givers who provided care in 2020 but not in 2017. This finding may be connected to a care-givers' recent transition into family care, as prior research has shown that particularly new care-givers experience declines in life satisfaction and quality of life (Sacco et al., Reference Sacco, König, Westerlund and Platts2022; Gerlich and Wolbring, Reference Gerlich and Wolbring2021).
In general, the not existing ‘COVID-19 effect’ on life satisfaction, but on depressive symptoms and loneliness, is in line with previous research (e.g. Entringer et al., Reference Entringer, Kröger, Schupp, Kühne, Liebig, Goebel, Grabka, Graeber, Kroh and Schröder2020; Wettstein et al., Reference Wettstein, Nowossadeck and Vogel2021). Wettstein et al. (Reference Wettstein, Nowossadeck and Vogel2021) argue that the COVID-19 pandemic has a greater impact on (primarily) affective (depressive symptoms, loneliness) than on judgemental (life satisfaction) wellbeing dimensions (for a deeper discussion, see Wettstein et al., Reference Wettstein, Nowossadeck and Vogel2021: 176, 182ff).
This study's findings highlight the need to not only monitor the wellbeing of the general population closely during the further course of the pandemic, but also that of family care-givers. The rise in loneliness among continuous care-givers might point to a particularly heightened form of social isolation experienced by family care-givers in the first stage of the COVID-19 pandemic (see Eggert et al., Reference Eggert, Teubner, Budnick, Gellert and Kuhlmey2020; Klaus and Ehrlich Reference Klaus and Ehrlich2021). It is an open question whether these higher levels on loneliness will return to baseline levels over time or whether they will stabilise at similar or even higher levels. Lasting loneliness has been shown to be a stressful experience that may interfere negatively with health (e.g. Böger and Huxhold, Reference Böger and Huxhold2018). Consequently, our results suggest that policies to mitigate the impact of the COVID-19 pandemic on population health also need to be directed towards (continuous) family care-givers as maintaining their health also benefits care recipients, whose health-care needs can only be met if their care-givers are in good condition.
To our knowledge our study is the first to show the impact of the pandemic on the wellbeing of family care-givers in Germany. While many previous studies draw on cross-sectional data collected in 2020, care-giver-specific samples or non-probability sampling designs (e.g. Eggert et al., Reference Eggert, Teubner, Budnick, Gellert and Kuhlmey2020; Wolf-Ostermann et al., Reference Wolf-Ostermann, Rothgang, Domhoff, Friedrich, Heinze, Preuß, Schmidt, Seibert and Stolle2020; Brandt et al., Reference Brandt, Garten, Grates, Kaschowitz, Quashie and Schmitz2021; Budnick et al., Reference Budnick, Hering, Eggert, Teubner, Suhr, Kuhlmey and Gellert2021), we are able to analyse COVID-19-driven changes in family care-givers' wellbeing by drawing on longitudinal data from a population-based sample of community-dwelling individuals.
However, our study has some limitations. For example, in 2020, the regular interviewer-administered and the subsequent self-administered questionnaire mode was replaced by a self-administered questionnaire mode without previous personal interviewer–interviewee contact. As a consequence, there is potential for estimation bias (selection, measurement error) due to changes in the data-collection mode. Also, in 2020, a shortened version of the DEAS questionnaire was used. Therefore, we were not able to examine the impact of different family care time demands or care tasks on family care-givers' wellbeing. Moreover, the 2020 survey was conducted after the peak of the first COVID-19 wave in Germany. Therefore, we might underestimate the immediate negative effects of the pandemic. Another limitation of this study results from the long, three-year period which passed between each survey. Therefore, on the one hand, our estimates might conceal changes in family care-givers' mental wellbeing due to adaptation processes (e.g. Haley and Pardo, Reference Haley and Pardo1989; Townsend et al., Reference Townsend, Noelker, Deimling and Bass1989; Pinquart and Sörensen, Reference Pinquart and Sörensen2003); on the other hand, the family care indicators used in this study may not completely mirror respondents' dynamics in family care provision, as, for example, some of the continuous family care-givers may have stopped providing family care for a period of time between the two surveys. Further, although we were able to rule out time-invariant unobserved heterogeneity by running first-difference regressions, time-variant unobserved heterogeneities might still cause bias as first-difference models are based on the assumption that the growth rate in wellbeing over time remains unaffected by between-group variation (Brüderl and Ludwig, Reference Brüderl, Ludwig, Best and Wolf2014).
Notwithstanding these limitations, our results yield heterogeneities in wellbeing between family care-givers and the non-care-giving population in the first stage of the pandemic: while family care-givers as well as non-care-givers experienced an increase in depressive symptoms and feelings of loneliness, only continuous care-givers showed more pronounced increases in loneliness compared to non-care-givers. Building on this research, detailed further analyses of the COVID-19 pandemic's longer-term consequences on family care-givers' as well as non-care-givers' wellbeing are necessary. For example, in order to gain greater insights into the wider context of the pandemic, future analyses should make use of population-based panel surveys covering further COVID-19 waves to investigate the evolution of family care-givers' wellbeing over the course of the pandemic. Moreover, future research should build on our approach and include a broad spectrum of wellbeing dimensions to obtain a nuanced and comprehensive picture of how family care-givers' and non-care-givers' wellbeing were affected at different stages of the pandemic. Finally, by considering other types of care-giving, future research may provide a more differentiated understanding of the family care–wellbeing association in times of the COVID-19 pandemic.
Data
Microdata of all the German Ageing Survey (DEAS) waves used are available free of charge for research, teaching and theses.
Acknowledgements
The authors would like to thank the anonymous reviewers for their helpful feedback and advise as well as Svenja M. Spuling and Georg Henning for their valuable suggestions.
Author contributions
All authors contributed to the study conception and design. Ulrike Ehrlich performed the data analyses and wrote the first draft of the manuscript. All authors contributed to material preparation and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Financial support
The German Ageing Survey (DEAS) is funded by the German Federal Ministry for Family Affairs, Senior Citizens, Women, and Youth (BMFSFJ) (grant number 301-1720-2/2). The content is the sole responsibility of the authors.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
The German Ageing Survey (DEAS) is a nationwide representative cross-sectional and longitudinal survey of the German population aged 40 and older. Ethical approval is not mandatory for general surveys in Germany. The DEAS is approved and funded by the Federal Ministry for Family Affairs, Senior Citizens, Women and Youth (BMFSFJ). The data assessments were carried out by the infas – Institut für angewandte Sozialwissenschaft GmbH (infas Institute for Applied Social Sciences) in Bonn in two phases. First, an oral, face-to-face interview usually conducted in the respondent's home. These personal interviews were held by trained interviewers with a standardised questionnaire. Second, respondents were also given a questionnaire to fill out. During the face-to-face interview, two tests were conducted starting from 2008: the digit–symbol test assesses the participants' ‘psychomotor speed’ and a peak-flow-meter is used in order to measure the respondents' lung capacity. Invasive methods are not part of the DEAS. DEAS survey participants give their informed consent by taking part on a voluntary basis after being invited and receiving detailed written information on the aims of the study, the voluntariness of participation, the assurance of data protection and of using collected data for scientific purposes only. At the end of the first interview, those respondents who are willing to further take part in the panel study give signed consent to save their address and to allow us to contact them again for the next survey waves. They are informed that they may revoke their consent whenever they want, that participation always is voluntary and that they are free to deny further participation. Informed consent after the initial survey participation is mandatory for future survey participation. The DEAS is counselled by a steady scientific academic advisory committee (https://www.dza.de/en/research/deas/advisory-committee) which receives all information on sampling, procedures to obtain the informed consent of participants, on questionnaires, topics and aims of each DEAS survey wave and thus ensures the scientific quality of the survey.
Appendix
Table A1. Items for the assessment of life satisfaction, depressive symptoms and loneliness
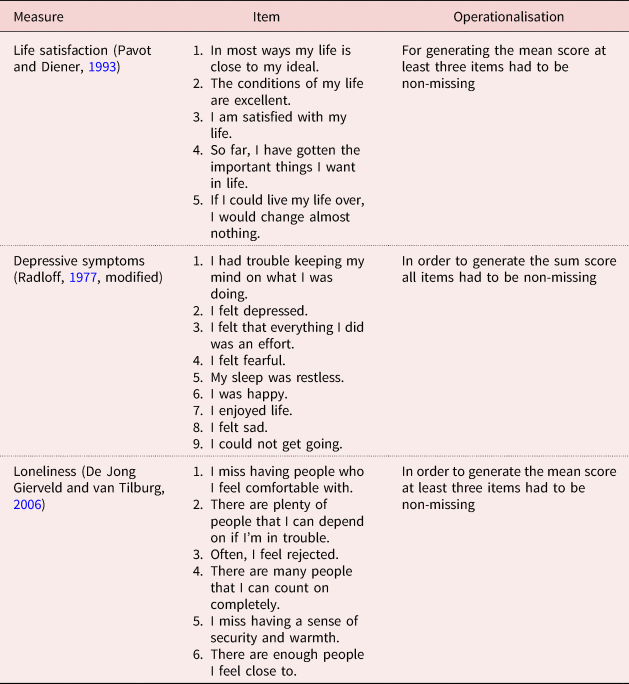
Table A2. Descriptive statistics of the study variables by survey year
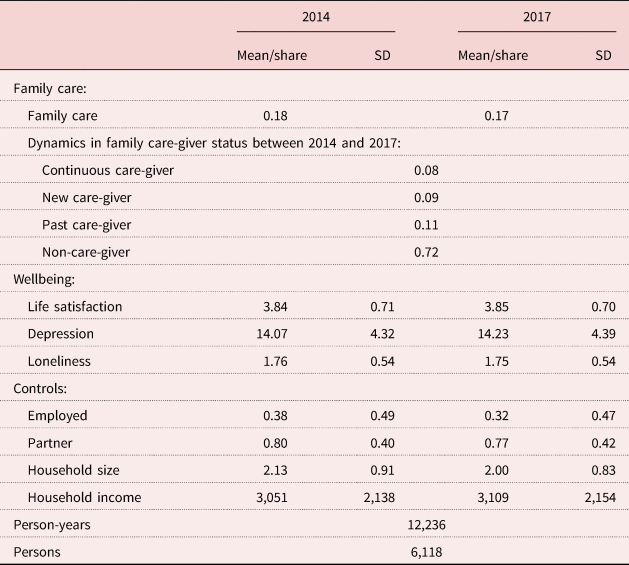
Table A3. Full first-difference regression models on three aspects of wellbeing, 2017–2020

Table A4. Full first-difference regression models on three aspects of wellbeing, 2014–2017











