Introduction
The most common causes of non-traumatic subarachnoid haemorrhage (SAH) are ruptured aneurysms and have very poor natural history.Reference van Gijn and Rinkel 1 Digital subtraction angiography (DSA) is commonly performed after CT angiography (CTA) when a patient is suspected to have an SAH to rule out intracranial aneurysms.Reference Thaker, Turner and Cobb 2 The most recent guideline from the American Heart and American Stroke Associations recommends using DSA for detecting aneurysms in patients with SAH.Reference Connolly, Rabinstein and Carhuapoma 3 The guidelines indicate that CTA can be used to guide decisions regarding aneurysm repair, but that DSA should be used when CTA is inconclusive. Despite these guidelines, clinicians and researchers are divided about the necessity of using DSA to detect aneurysms after SAH.Reference Agid, Andersson and Almqvist 4 - Reference MacKinnon, Clifton and Rich 9 Up to 20% of SAH patients have no aneurysm detected on initial angiography imaging.Reference Jadhav and Jovin 10 , Reference Rinkel, van Gijn and Wijdicks 11 Given that DSA is resource-intensive and invasive, CTA is increasingly being used to detect ruptured aneurysms following SAH.Reference McDonald, Kallmes and Lanzino 12
Imaging of head and neck vessels with CTA has improved since helical CT was introduced, and it provides high-resolution three-dimensional reconstructions and shorter acquisition time.Reference Agid, Andersson and Almqvist 4 In addition to these improvements in technology, radiologists’ increasing familiarity with interpreting source images has increased the utility of CTA.Reference Thaker, Turner and Cobb 2 Thus, interventional radiologists are able to diagnose patients more efficiently with suspected SAH because of enhancements in CTA imaging and training. Increased use of CTA, however, has not been accompanied by a matching decrease in DSA, resulting in multiple tests without gain in diagnostic yield.Reference McDonald, Kallmes and Lanzino 12 Given the improvements in CTA and the disadvantages of DSA, it is imperative to investigate whether a DSA is truly necessary for a negative SAH finding on a CTA.Reference Agid, Andersson and Almqvist 4 The purpose of this study was to review cases of suspected aneurysmal SAH at our institution to determine whether a CTA was sufficient to exclude a diagnosis of intracranial aneurysms in patients with suspected SAH.
Materials and Methods
Data Collection
The study was approved by our institutional research ethics board. In a retrospective study, all cerebral DSA performed from August 2010 to July 2014 for any indications were analysed. Subarachnoid haemorrhage was identified through positive finding on non-contrast computed tomography scans and/or lumbar punctures. Among those with confirmed SAH, only patients who had a negative CTA were selected for this study. Results from CTA with source images were compared with DSA.
Image Acquisition and Analysis
Following standard protocols, CTA was performed on 64-section multidetector CT scanners and DSA in a dedicated biplane neuroangiography unit (Axiom Artis, Siemens). All images were analysed on a Picture Archiving and Communication System (PACS) workstation. Retrieval of patient information and radiology reports were reviewed for patient selection. The CTA and DSA images of the patients with CTA-negative SAH were reviewed on PACS by a fellowship-trained neuroradiologist (JJSS) to confirm the diagnosis and to rule out any possibilities of dictation errors.
Results
In total, 857 DSA were performed during the study period; 50 (5.83%) DSA were performed in 35 patients who presented with SAH and had negative CTA for any possible aetiology of SAH. The patients’ demographic information is summarised in Table 1. Of the 35 patients, only 3 (8.57%) patients had positive findings on the DSA.
Table 1 Demographic details of the patients with CT angiography (CTA)-negative subarachnoid haemorrhage (SAH)

–ve=negative; +ve=positive; DSA=digital subtraction angiography; LP=lumbar puncture.
One patient presented with SAH in the pre-pontine and cerebellopontine cistern with CTA-negative for evidence of aneurysm (Figure 1). DSA showed irregularity in the V4 segment of the right vertebral artery. This was not obvious on CTA. In the absence of any other obvious aetiology and owing to the presence of maximum SAH around this area, this was thought to be a dissection. This was not obvious on CTA. This finding was equivocal and could have been a focal vasospasm from the presence of the SAH. Vasospasm on day 1 after SAH is extremely rare.

Figure 1 Patient presented with subarachnoid haemorrhage predominantly in the posterior fossa (A). CT angiogram did not show any source for this subarachnoid haemorrhage (B, C). Digital subtraction angiography showed irregularity in the wall of the V4 segment of the right vertebral artery (D), which was not very well seen on the lateral view (E). In the absence of any other source and owing to the proximity of this irregularity to the subarachnoid haemorrhage, this was diagnosed as dissection of the vertebral artery. No other imaging evidence of dissection was seen.
The second patient had SAH in the pre-pontine cistern with intra-ventricular extension with negative CTA for any evidence of aneurysm. On DSA, the only suspicious finding was a tiny (1.5 mm in maximum diameter) outpouching from the left paraclinoid ICA (Figure 2). The appearance favoured an infundibular origin of a hypoplastic posterior communicating artery. However, a tiny, sessile aneurysm could not be excluded. This finding did not show any change even on the third follow-up DSA. The patient did not receive any treatment for this finding, did not have a re-bleed and made an excellent recovery.

Figure 2 Patient had subarachnoid haemorrhage predominantly in the suprasellar and interpeduncular cistern more so on the right side (A). CT angiogram did not show any source of the subarachnoid haemorrhage (B). Digital subtraction angiogram showed a suspicious finding of a tiny infundibulum (arrow) from the contralateral (left) paraclinoid ICA (C). This remained stable on the 3rd follow-up for subarachnoid haemorrhage and was thought not to be the source of subarachnoid haemorrhage.
The third patient was referred to us from another institution with the initial diagnostic CT and CTA showing SAH but no aneurysms. The patient underwent DSA in our institution that demonstrated a small posterior inferior cerebellar artery aneurysm. This patient underwent another CTA in our institution before undergoing coiling, which demonstrated the aneurysm of exactly the same shape and size. In retrospect, the initial CTA did not cover the region of the aneurysm (Figure 3).
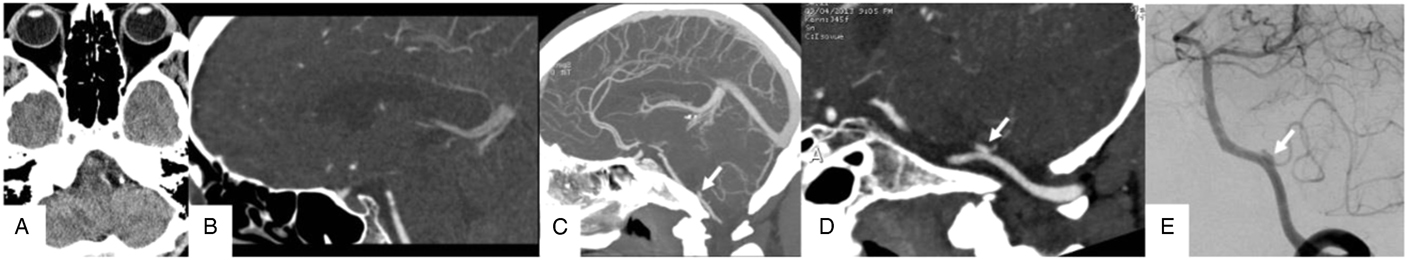
Figure 3 Patient had a small subarachnoid haemorrhage in the left cerebellopontine angle cistern (A). CT angiogram performed in an outside institution did not show any source of this subarachnoid haemorrhage (B), but this CT angiogram did not even cover the area of focal subarachnoid haemorrhage. CT angiogram repeated in our institution covering the whole brain (C) showed a left posterior inferior cerebellar artery origin aneurysm (C, arrow). This aneurysm (arrow) seen on the reconstructed image (D) looked exactly similar in size and shape to what was seen on the digital subtraction angiography (E, arrow).
Discussion
In this retrospective study comparing CTA with the criterion standard of DSA, we demonstrated the relative futility of DSA in patients with CTA-negative SAH. Of the 35 patients with CTA-negative SAH, three were reported to have positive findings on follow-up DSA. Dissection was suspected but could not be confirmed in the first patient. A tiny, sessile aneurysm could not be ruled out in the second case, but the patient received no treatment for an aneurysm and made a full recovery. In the third patient, a posterior inferior cerebellar artery aneurysm was not seen initially because the initial CTA did not cover the area of the brain where the aneurysm was located. When another CTA was performed immediately after the DSA, it showed the aneurysm very well. The final case underscores the importance of having properly trained professionals who meticulously follow standard protocols in optimising the use of CTA.
Our findings are consistent with earlier studies that report high sensitivity (97%-100%) of CTA for detecting intracranial aneurysms.Reference Kershenovich, Rappaport and Maimon 13 - Reference Prestigiacomo, Sabit and He 15 Similarly, results from a large systematic review and meta-analysis comprising 50 studies calculated the pooled sensitivity and specificity of CTA in the diagnosis of cerebral aneurysms in SAH to be 98% and 100%, respectively.Reference Westerlaan, van Dijk and van Dijk 16 In lieu of DSA, the aforementioned evidence provides strong support for CTA to serve as the sole diagnostic imaging modality for intracranial aneurysm detection within the SAH population.
However, a recent retrospective analysis of 643 patients suggests that CTA accuracy may be lower than presented in earlier investigations. Philipp et alReference Philipp, McCracken and McCracken 17 reported sensitivity of CTA to be 70.7% for overall SAH, 57.6% for very small aneurysms (<5 mm) and 45% for internal carotid artery aneurysms. As acknowledged by the authors, this was possibly a result of variability in imaging data relating to methods, locations, technology, time frame and expert staff in the study.Reference Philipp, McCracken and McCracken 17 The legitimacy of CTA in the diagnosis of cerebral aneurysms in patients with SAH has been challenged in the past. In addition to small aneurysms, previous studies have highlighted that CTA struggles with detecting aneurysms located adjacent to the bone/skull base or at a tortuous vessel loop.Reference Kallmes, Layton and Marx 6 , Reference Haider, Gottlich and Khahera 18 - Reference Moran 20
We argue that the sensitivity of CTA may have been underestimated in some studies owing to misinterpretation of imaging scans potentially because of the lack of observer experience. Earlier investigations have shown that the accuracy of CTA detection of intracranial aneurysms can improve as the readers gain more experience or exposure.Reference Pedersen, Bakke and Hald 21 , Reference Jayaraman, Mayo-Smith and Tung 22 One study reported sensitivities for CTA increasing from 69% on initial aneurysms (n=13) to 84% on subsequent aneurysms (n=13).Reference Jayaraman, Mayo-Smith and Tung 22 Similarly, neuroradiologists have been found to consistently perform better than non-neuroradiologists in detecting intracranial aneurysms via CTA.Reference White, Wardlaw and Lindsay 23 This underscores the importance of both, the use of correct protocol with modern CTA technology and increasing expertise with the interpretation of these images, in increasing the capability in depicting intracranial aneurysms on non-invasive CTA compared with DSA. For example, in a prospective study of 133 patients and five independent reviewers of images, the sensitivity for aneurysms <3 mm was reported to be greater for the 64-slice CTA (96.3%) compared with the DSA (85.2%).Reference Xing, Chen and Sheng 24
Although DSA has long been regarded as the golden standard, an increasing number of studies show that DSA is unnecessary, invasive and costly.Reference Jabbarli, Shah and Taschner 8 Specifically, we propose that a DSA is unnecessary for the diagnosis of patients with SAH when a thorough CTA with appropriate protocol and review returns negative findings. On the basis of the present study, if CTA identifies no aneurysm in patients with SAH, then it can be assumed that the origin of the SAH is non-aneurysmal in nature. Nevertheless, diagnostic accuracy is dependent on the physicians who interpret the images. As radiologists gain more experience with the technology, the advantages of CTA over DSA increase.Reference Thaker, Turner and Cobb 2 Trusting such negative findings on CTA can expedite further management.
Limitations
The limitations of this study must be considered when interpreting its findings. Specifically, the retrospective nature of the study design and its potential for selection bias may limit the generalisability of its results. Given our small sample size, additional studies may be required to fully elucidate CTA diagnostic capabilities related to SAH.
Conclusion
In patients with SAH, negative findings on a technically sound CTA are reliable in ruling out aneurysms in any pattern of SAH or no blood on CT. Our observations need to be confirmed with larger prospective studies.
Acknowledgement
The authors acknowledge the Radiology Research Foundation of Dalhousie University for their funding of the summer research student grant.
Financial Support
This study was supported by funding provided by our institution’s Radiology Research Foundation.
Conflicts of Interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Statement of Authorship
JJSS participated in the conception and design of the study. LH collected the raw data. LH and JJSS analysed and interpreted the data. JJSS was responsible for statistical expertise. JJSS, HW and JB were responsible for initial drafting of the manuscript. JJSS, HW, LH and JB were involved in critically reviewing the draft manuscript and will be participating in revisions of the final manuscript.
Disclosures
All authors declare that they have nothing to disclose.








