The Canterbury earthquakes in New Zealand started with a 7.1 magnitude earthquake on 4 September 2010 and continued for more than 2 years, with further major earthquakes in February, June and December 2011 and over 10 000 aftershocks. As a consequence of the Canterbury earthquakes, the general public, media and health professionals were concerned that there would be widespread adverse effects on the mental health of young persons.Reference Keogh1,Reference Stewart2 These concerns are consistent with psychiatric literature that reports higher rates of psychiatric disorder and mental distress following natural disasters in adults.Reference Norris, Friedman, Watson, Byrne, Diaz and Kaniasty3–Reference Beaglehole, Mulder, Frampton, Boden, Newton-Howes and Bell6 Studies that examine the effects of disasters on children and young people are less common but in general these also report adverse effects (predominantly increased rates of anxiety, depression, sleep disturbance, general psychological distress and post-traumatic stress disorder)Reference Norris, Friedman, Watson, Byrne, Diaz and Kaniasty3,Reference Bartels and VanRooyen7–Reference Wang, Chan and Ho11 and emphasise the importance of family and community in recovery.Reference Aptekar and Boore9,Reference Vogel and Vernberg10,Reference Hafstad, Gil-Rivas, Kilmer and Raeder12
Dispensing data following a natural disaster have previously been used to monitor community psychiatric morbidity,Reference Rossi, Maggio, Riccardi, Allegrini and Stratta13–Reference Beaglehole, Bell, Frampton, Hamilton and McKean15 although we are unaware of their use to monitor young people. Generally, psychiatric medication is recommended as a second-line intervention for treating young people who remain impaired by mental illness after psychological interventions have been tried.Reference Malhi, Bassett, Boyce, Bryant, Fitzgerald and Fritz16,Reference Andrews, Bell, Boyce, Gale, Lampe and Marwat17 This means that psychiatric medicine dispensing rates for young people can be used as a proxy for the prevalence of significant and persistent psychiatric problems (as opposed to psychological distress and mild psychiatric disorder, which are usually managed with community resources and psychological interventions). The aim of this study is therefore to establish the impact of the Canterbury earthquakes on the prevalence of psychiatric problems requiring medication in young people through an examination of long-term dispensing data for the Canterbury District Health Board (DHB) compared with national data.
Method
Data were accessed from the Pharmaceutical Collection, a data warehouse that contains all dispensing data for New Zealand. The amount of medication dispensed, in units, by all pharmacies is routinely recorded nationally for district health boards (DHBs) (regional organisations that provide health and disability services to populations within a defined geographical area). A unit of medication is defined as a tablet of any strength. In general, units of medication dispensed will correlate with the total amount of medication used by the population.
We examined the units dispensed of the pharmaceutical classes of antidepressants, antipsychotics, anxiolytics, and sedatives/hypnotics as defined by the Pharmaceutical Management Agency (PHARMAC, a New Zealand Crown agency that decides which medicines and related products are subsidised for use in the community and public hospitals) limited to persons aged 18 and under. We also examined data specifically for quetiapine, given the common off-label use of this medication for anxiety, and methylphenidate, in case dispensing of these medications were affected by the earthquakes.
We examined pharmacy dispensing over an extended period from January 2008 to August 2018. This provided the opportunity to examine local and national trends existing before the onset of the earthquake series in September 2010 and to clarify any short- and long-term effects of the earthquakes on medication dispensing. Short-term effects were defined as time-limited signals detected in the 2 months following the most devastating quake of February 2011, whereas long-term effects were considered to be present if sustained effects in the years following the onset of the earthquake sequence were detected.
We compared dispensing data for those aged 18 and younger in the Canterbury DHB region with national figures, excluding the Canterbury DHB. The Canterbury DHB provides health services to around 550 000 people in the city of Christchurch, outlying towns and rural areas. The dispensing data include all prescriptions dispensed in this region (approximately 11.5% of the national population). Greater Christchurch (defined as the city of Christchurch and immediate outlying towns within a commuter belt) comprises 85% of the population serviced by the Canterbury DHB and was the area most affected by the series of earthquakes.
Statistics New Zealand provided annual population estimates for those aged under 19 over the study period. Data were therefore corrected for annual changes in population and are reported as a ratio of Canterbury dispensing per 100 000 under-19-year-old population compared with rest-of-New Zealand dispensing per 100 000 under-19-year-old population in order to directly compare Canterbury DHB and national dispensing. A ratio of 1 means rates of dispensing in Canterbury are equal to rates of dispensing in the rest of New Zealand. Increases in the ratio following the onset of the earthquakes would suggest deteriorating mental health, whereas reductions would indicate the opposite.
Ethics approval was not sought because no individual data were received and large-scale population data were provided and analysed in aggregated form.
Results
In January 2008, there were 129 870 individuals who were aged 18 years and under in the Canterbury DHB catchment area and 1 082 400 in the rest of New Zealand. These numbers had increased to 139 410 and 1 119 415 respectively by the study end in August 2018.
Antidepressants
Assuming a typical dose of one antidepressant daily, approximately 0.9% of young people were dispensed antidepressants in Canterbury at the start of the study period, rising to 1.7% by the study end. This compares with 0.4 and 1.2% respectively for the rest of New Zealand.
Children and adolescents in Canterbury were dispensed antidepressants at a higher rate than children and adolescents in the rest of New Zealand for the entire study period (Fig. 1). The ratio of Canterbury:rest-of-New Zealand dispensing was decreasing prior to the earthquakes. This ratio of dispensing flat-lined between September 2010 and May 2014 and then reduced steadily for the remainder of the study. The period in which the ratio flat-lined suggests a possible effect of the earthquakes on dispensing, although the predominant features of antidepressant dispensing are higher dispensing rates for antidepressants in Canterbury matched by dispensing for the rest of New Zealand ‘catching up’ over the study period. Supplementary Appendix A (available at https://doi.org/10.1192/bjp.2019.273) provides the raw data for dispensing of antidepressants and the other study medications in spreadsheet form.
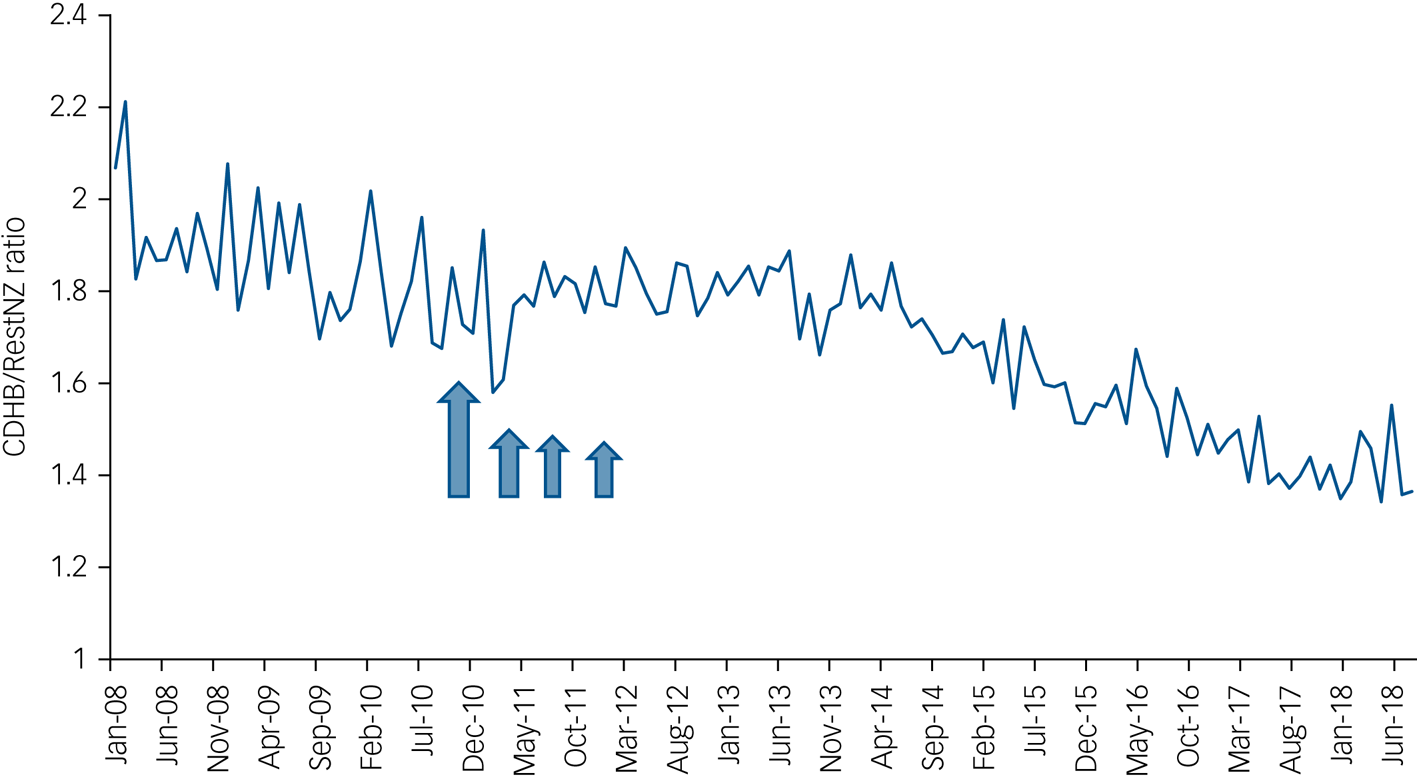
Fig. 1 Population-adjusted dispensing of antidepressants for young people under 19 years of age in the Canterbury District Health Board (DHB) region as a ratio of dispensing in the rest of New Zealand (CDHB/RestNZ), scaled per 100 000 population to allow direct comparison between the Canterbury DHB and national population to be made. Arrows are included to highlight the start of the earthquake sequence and the timing of major aftershocks.
Antipsychotics
Assuming a typical dose of one antipsychotic tablet daily, approximately 0.2% of young people in Canterbury and the rest of New Zealand were dispensed antipsychotics in the pre-earthquake period. This rose to approximately 0.5% for both populations by the study end.
Children and adolescents in the Canterbury DHB area tended to be dispensed antipsychotics at a higher rate than those in the rest of New Zealand over the study period (Fig. 2). The ratio of dispensing fell after February 2011, before climbing again and remaining steady until late 2017, when it fell once again. The highest ratio of dispensing was in the pre-earthquake period.
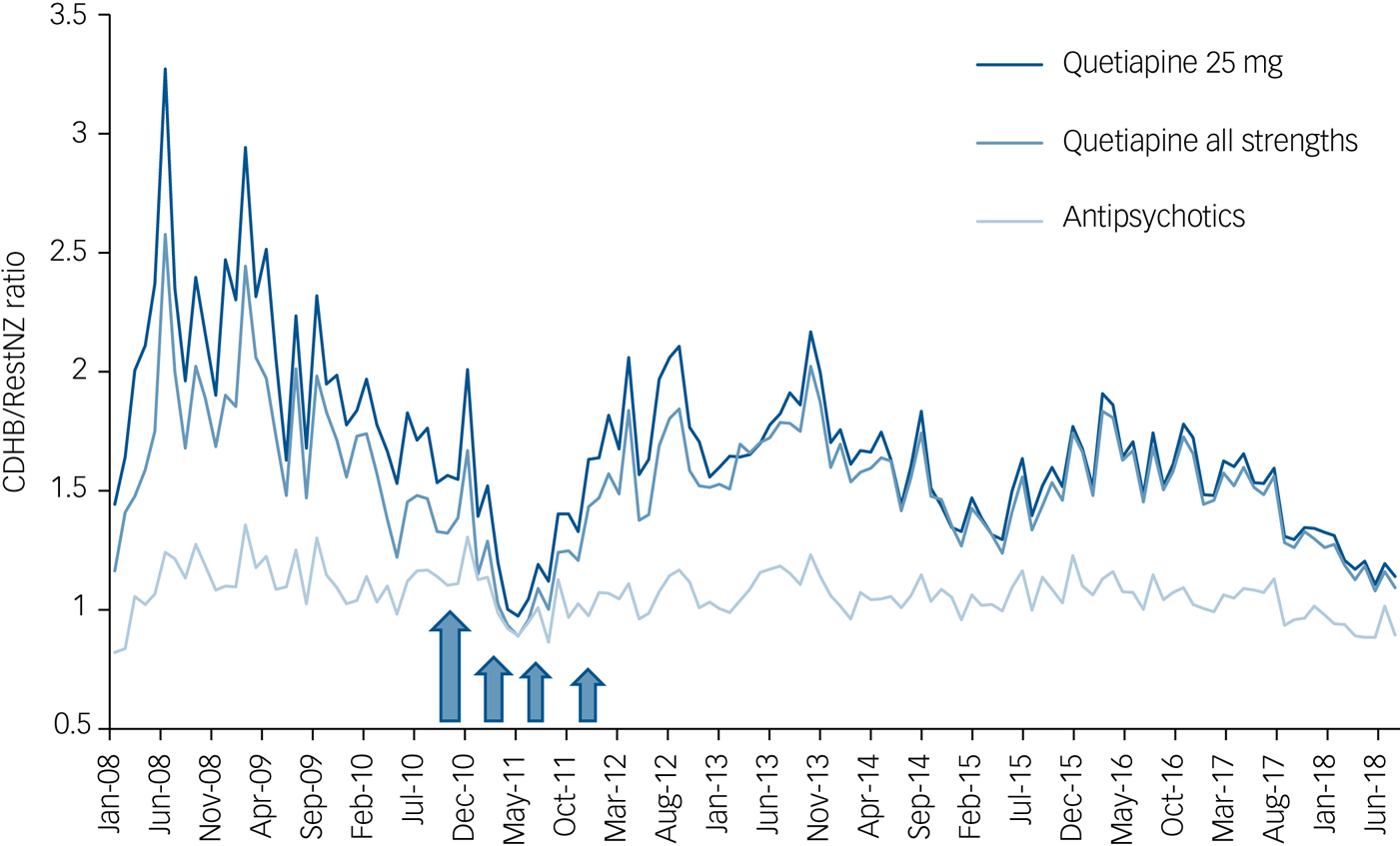
Fig. 2 Population-adjusted dispensing of antipsychotics and quetiapine for young people under 19 years of age in the Canterbury District Health Board (DHB) region as a ratio of dispensing in the rest of New Zealand (CDHB/RestNZ), scaled per 100 000 population to allow direct comparison between the Canterbury DHB and national population to be made. Arrows are included to highlight the start of the earthquake sequence and the timing of major aftershocks.
Children and adolescents in Canterbury were also dispensed quetiapine (all strengths and 25 mg tabs) at a higher rate than in the rest of New Zealand for the majority of the study period (Fig. 2). The ratio of dispensing fell between 2009 and April 2011, before climbing and fluctuating for the remainder of the study period. Although adverse effects of the earthquakes were not apparent, the lowest ratio of dispensing for antipsychotics and quetiapine occurred in the months after the February 2011 earthquake, suggesting possible earthquake-related influences on dispensing for these medications.
Anxiolytics and sedatives/hypnotics
Assuming a typical dose of one anxiolytic or sedative/hypnotic daily, approximately 0.05% of young people in Canterbury and the rest of New Zealand were dispensed anxiolytics and sedatives/hypnotics in the pre-earthquake period. This rose to 0.07% of young people in Canterbury and the rest of New Zealand by the study end. Melatonin became subsidised for young people with persistent insomnia secondary to a neurodevelopmental disorder in 2017, causing a steep rise in the recorded use of sedatives/hypnotics, but it was excluded from this calculation as it was unavailable for most of the study period.
The ratio of dispensing of anxiolytics and sedatives/hypnotics for children and adolescents in Canterbury compared with the rest of New Zealand fluctuated over the study period (Fig. 3). No clear longitudinal or earthquake-related trends were apparent, although the dispensing ratios tended to be above 1, indicating that rates of dispensing in Canterbury were higher than in the rest of New Zealand for most of the study period.
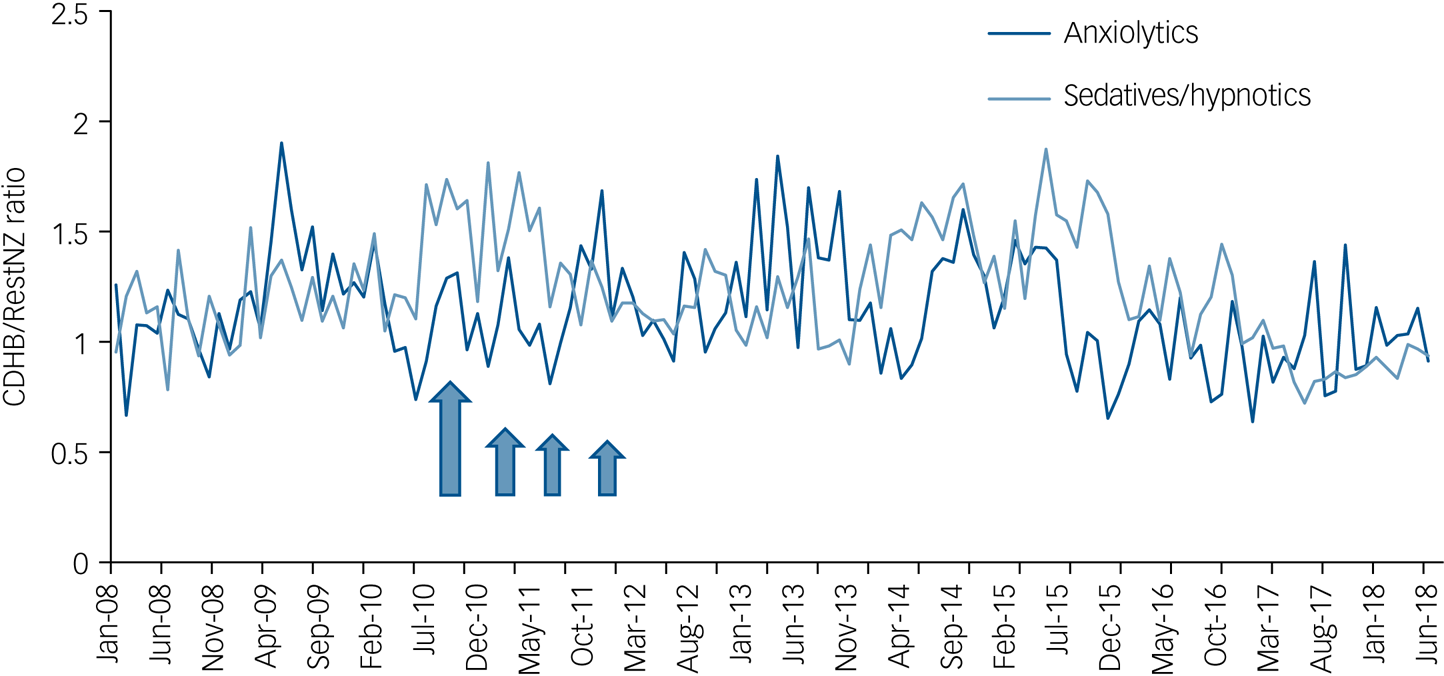
Fig. 3 Population-adjusted dispensing of anxiolytics and sedatives/hypnotics for young people under 19 years of age in the Canterbury District Health Board (DHB) region as a ratio of dispensing in the rest of New Zealand (CDHB/RestNZ), scaled per 100 000 population to allow direct comparison between the Canterbury DHB and national population to be made. Arrows are included to highlight the start of the earthquake sequence and the timing of major aftershocks.
Methylphenidate
Assuming a typical dose of two methylphenidate tablets daily, approximately 0.5% of young people in the Canterbury DHB region were dispensed methylphenidate in the pre-earthquake period (Fig. 4). This rose to 0.6% by the end of the study period. This compares with 0.3 and 0.7% respectively for the rest of New Zealand. The ratio of dispensing for children and adolescents in Canterbury compared with the rest of New Zealand was 1.7 at the beginning of the study period. It fell steadily during the pre-earthquake period and then remained around 1 between March 2011 and June 2018. No earthquake-related effects on dispensing were apparent.
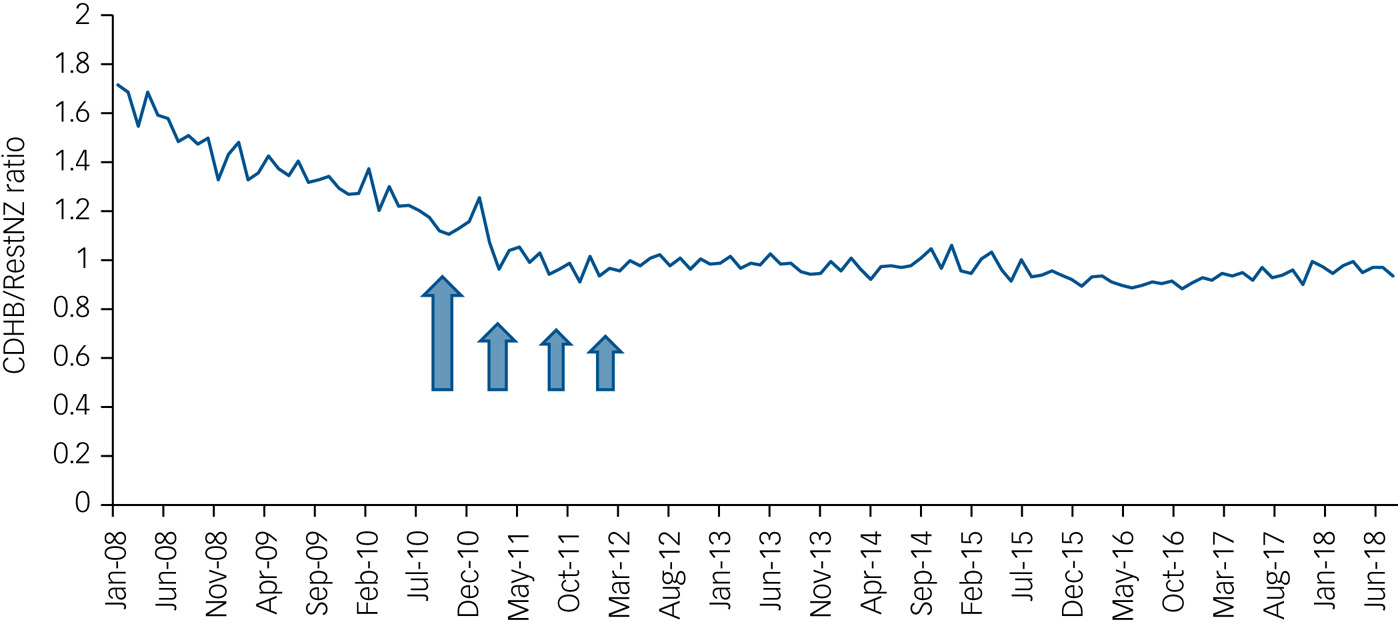
Fig. 4 Population-adjusted dispensing of methylphenidate for young people under 19 years of age in the Canterbury District Health Board (DHB) region as a ratio of dispensing in the rest of New Zealand (CDHB/RestNZ), scaled per 100 000 population to allow direct comparison between the Canterbury DHB and national population to be made. Arrows are included to highlight the start of the earthquake sequence and the timing of major aftershocks.
Discussion
We did not detect an increase in dispensing of psychotropic medication for children and adolescents. The flat-lining of dispensing of antidepressants for the Canterbury DHB region compared with the rest of New Zealand represents a possible adverse effect attributable to the Canterbury earthquakes, although no increase in the ratio of dispensing is present. For all medication types, the pre-earthquake baseline ratio of dispensing was higher than the ratio of dispensing by the end of the study period.
Comparison with previous studies
Our study was strengthened by the use of longitudinal data commencing prior to the onset of the earthquakes and the use of appropriate controls. For example, if antidepressant dispensing were evaluated only in Canterbury following the onset of the earthquakes, large increases of antidepressant dispensing would be reported. However, pre-earthquake data reveal that increases in dispensing started before the earthquake sequence. In addition, the use of controlled data highlights that increases in Canterbury were matched by steeper increases in the rest of New Zealand, suggesting that adverse effects of the Canterbury earthquakes do not account for the increase in antidepressant dispensing recorded.
We previously identified two studies evaluating the mental health of young people in Canterbury following the Canterbury earthquake.Reference Beaglehole, Mulder, Boden and Bell18 The first study examined parent-reported emotional and behavioural problems in 4-year-old children as part of a New Zealand-wide health and development check prior to school entry and did not identify any adverse effects in Canterbury children as a result of the earthquake sequence.Reference Thomson, Seers, Frampton, Hider and Moor19 The second study, by Liberty et al,Reference Liberty, Tarren-Sweeney, Macfarlane, Basu and Reid20 utilised teachers to rate the behaviour of 212 5-year-olds several years after the onset of the earthquake sequence and reported the opposite. Although each study used pre-disaster measures and appropriate controls, large population studies include many individuals with lesser degrees of earthquake exposure and are therefore less sensitive to detecting change than studies that only sample individuals with high earthquake exposure. The study by Liberty et al Reference Liberty, Tarren-Sweeney, Macfarlane, Basu and Reid20 was situated in an area of greater earthquake damage and children in this area may therefore have greater earthquake-related difficulties than children from a wider sampling pool. The use of teachers who were also likely to have been exposed to the earthquakes and have a heightened awareness of the negative effects of trauma on behaviour may also have introduced reporting bias to the study design that is not present in studies such as ours, which used dispensing as a proxy for rates of significant mental illness.
Our study sits within the broader literature evaluating the impacts of disasters on young people. In general, these studies report adverse effects on mental health,Reference Norris, Friedman, Watson, Byrne, Diaz and Kaniasty3,Reference Bromet and Dew8–Reference Vogel and Vernberg10 although methodological problems have also been highlighted in reviews of the disaster literature (principally the failure to use longitudinal data, the absence of appropriate controls, and sampling techniques that do not evaluate the population of interest).Reference Goldmann and Galea4,Reference Rubonis and Bickman5,Reference Norris21 These methodological concerns were addressed by our study design and therefore place weight in support of the findings of our study.
What is it about the post-earthquake disaster setting in Canterbury that meant only minimal adverse effects of the earthquake were detected? Following the earthquakes, there was a large-scale community and public health effort (the All Right? campaign: https://allright.org.nz/about-us), designed to promote mental health in those affected by the earthquakes. This was coupled with extensive school interventions, free counselling and extended general practice consultations for all. It is likely that these and other community initiatives minimised any adverse effects that may have occurred as a result of the earthquakes. It is also possible that the widespread availability of support services in Canterbury following the earthquakes reduced the demand for medications in Canterbury in a way that did not occur nationally, where such services were not present.
Limitations
For the majority of common psychiatric conditions affecting children and adolescents, first-line treatments are usually psychosocial, and medication is used after a failed trial of a psychological therapy, for prolonged symptomatology or after specialist consultation.Reference Malhi, Bassett, Boyce, Bryant, Fitzgerald and Fritz16,Reference Andrews, Bell, Boyce, Gale, Lampe and Marwat17 The percentage of young people in Canterbury taking any of the study medications ranged from 0.05% for anxiolytics and sedatives/hypnotics to 1.7% for antidepressants. These figures are lower than for the corresponding adult population.Reference Exeter, Robinson and Wheeler22 They suggest that in New Zealand, psychiatric medication is only being used for young people with significant and persistent mental health concerns. This means that there is a gap between total community morbidity and that measured by our dispensing records. However, the data provided tracked morbidity of particular relevance to physicians and healthcare services, although other methods will identify a larger pool of potential patients.Reference Tannenbaum, Lexchin, Tamblyn and Romans23
The use of dispensing as a proxy for morbidity is only valid if the threshold for prescribing psychiatric medication by clinicians remained constant over the earthquake period. It is conceivable that general practitioners are less likely to prescribe psychiatric medication if there is an obvious psychosocial context for the presenting problem. In the adult population, increasing dispensing of psychiatric medication has been reported following disasters (at least in the short term).Reference Rossi, Maggio, Riccardi, Allegrini and Stratta13–Reference Beaglehole, Bell, Frampton, Hamilton and McKean15 This suggests that reduced propensity to prescribe is unlikely to be a dominant explanation, although we are unable to quantify this possibility for younger populations. We also considered whether other factors, such as religious faith, may provide a helpful context to the dispensing patterns reported. Religious faith increased in the post-earthquake period but this was not associated with improved subjective well-being.Reference Sibley and Bulbulia24 Subjective well-being fell for the minority who lost religious faith in the post-earthquake period but this group constituted only a small percentage of the overall population, suggesting the absence of significant effects of religion on prescribing for mental illness.Reference Sibley and Bulbulia24
In the post-disaster setting, adequate access to healthcare is essential if dispensing records are to be a useful measure of morbidity and service need. Following the Canterbury earthquakes, access to primary and secondary services was enhanced for children and adolescents through post-quake initiatives, suggesting that in Canterbury the use of dispensing data as a proxy for community morbidity of a severity to result in treatment with psychiatric medication is reasonable.
Author contributions
G.J.H. and T.Z.: data extraction and analysis and review of write-up. B.B.: study design, data analysis and write-up. C.M.A.F., C.J.B., J.M.B. and R.T.M.: study design, data analysis and review of write-up. S.M.: data analysis and write-up.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2019.273.









eLetters
No eLetters have been published for this article.