Introduction
The Royal Flying Doctor Service South Eastern (RFDS SE; Sydney, NSW, Australia) provides aeromedical prehospital and retrieval services in rural New South Wales, Australia. Many trauma cases are “primary in-hospital” cases, where the patient is brought from the scene to a remote clinic or hospital. In these remote health care facilities, access to critical care services is limited. Retrieval teams therefore assesses and stabilize the patient locally before transferring them by a combination of road vehicle or fixed wing aircraft (Beechcraft King Air; Textron Aviation, Wichita, Kansas USA) to the receiving center. A common problem in the retrieval environment is pain management.Reference Lamb1 Thoracic trauma can be very painful, which can impact respiratory function and increase morbidity.Reference Unsworth, Curtis and Asha2 Presented are two cases where erector spinae blocks (ESBs) were successfully used in an aeromedical retrieval setting to control pain in chest trauma.
Cases
Written consent to publish their cases was obtained from both patients following their retrieval.
Case 1
A 52-year-old male was brought to a remote clinic following a motor bike accident. He had no significant past medical history and no regular medications. Chest X-ray in the clinic demonstrated a left hemopneumothorax with second to sixth rib fractures and a mid-scapula fracture. His pain score was 8/10 despite multiple doses of morphine, and his breathing was impaired. The patient was not able to lie flat due to pain. An ultrasound-guided ESB was performed by the retrieval team with 30ml of 0.75% ropivicaine, followed by the insertion of an intercostal catheter. A total of 40mg intravenous (IV) ketamine was given to facilitate tube thoracostomy. Following these interventions, the pain score dropped to 1/10 and his breathing pattern improved. The patient was transferred in a lying position via ambulance and aircraft to the receiving facility and did not require further analgesia for six hours. After arrival at the receiving hospital, pain was controlled with multimodal pain therapy. The patient was discharged from the high dependency unit 48 hours later.
Case 2
A 24-year-old male presented to a remote clinic having fallen onto a tool box and impaled his chest on a 10cm screwdriver. The patient removed the screwdriver himself prior to attending medical services. He had no other injuries. His past medical history included attention deficit hyperactivity disorder (ADHD), cigarette smoking, and daily consumption of cannabis.
Chest X-ray and extended focused assessment with sonography for trauma (eFAST) did not show any significant pathology. Despite treatment with 10mg morphine IV, 1g paracetamol, and 400mg ibuprofen, the patient was in severe pain (8/10) and could not take deep breaths or cough. An ESB was performed under ultrasound guidance with 20ml of 1% ropivicaine, following which his pain score reduced to 1-2/10. His breathing pattern improved and he was transported to the receiving hospital via ambulance and aircraft without any further analgesic requirements. The patient was discharged 24 hours later.
Discussion
The cases presented describe the benefits of regional anesthesia in providing high-quality, opiate-sparing analgesia for prolonged aeromedical retrieval.
The use of regional anesthesia prehospitally has been described for the management of femoral fractures;Reference Hards, Brewer, Bessant and Lahiri3 and more recently, the use of serratus anterior blocks as analgesia for rib fractures in aeromedical transfer has also been published.Reference McLean, Cooke, Burns and Reid4 This is the first report in the literature of single-injection ESB being used in the retrieval environment, despite their established use in-hospital.Reference Hamilton and Manickam5
The ESB is performed with the patient in either the upright sitting or lateral decubitus position, with inline ultrasound guidance. The erector spinae muscle (ESM) complex runs vertically in the back, lateral to the spinal column. It is comprised of the spinale, longissimus thoracis, and iliocostalis muscles. The ESM lies directly on top of the transverse process (TVP) of the vertebral body. The TVP is identified in a longitudinal parasagittal plane approximately 3cm lateral to the midline on the affected side using ultrasound (Figure 1). The TVP appears as a flattened, squared acoustic shadow with minimal pleura visible (Figure 2). In contrast, the image of a rib appears rounded with associated pleura underlying (Figure 3). The needle tip is directed onto the TVP and local anesthetic is injected below the ESM on top of the TVP. The anesthetic spreads in a cranio-caudal plane by one dermatome for approximately each 3.4ml of injectate,Reference De Cassai and Tonetti6 so the target injection site should be in the middle of the area to be blocked. The mechanism of action of the ESB is by anterior diffusion of anesthetic into the paravertebral and epidural spaces, and lateral diffusion into the intercostal spaces.Reference De Cassai and Tonetti6-Reference Ueshima and Hiroshi8 This blocks the dorsal and ventral rami of the spinal nerves, which provide sensation to both the anterior and posterior chest wall.

Figure 1. Positioning of the Patient in the Upright Sitting Position. Note: 1 = midline/spinous process; 2 = approximate position of the transverse processes; 3 = position of the scapulae.

Figure 2. View of the Transverse Process Deep to the Erector Spinae Muscle in the Longitudinal Parasagittal Orientation with a Linear 13-6MHz Probe. Note: The transverse process is a square acoustic shadow with no pleura visible. Dotted line: desired needle placement for block.
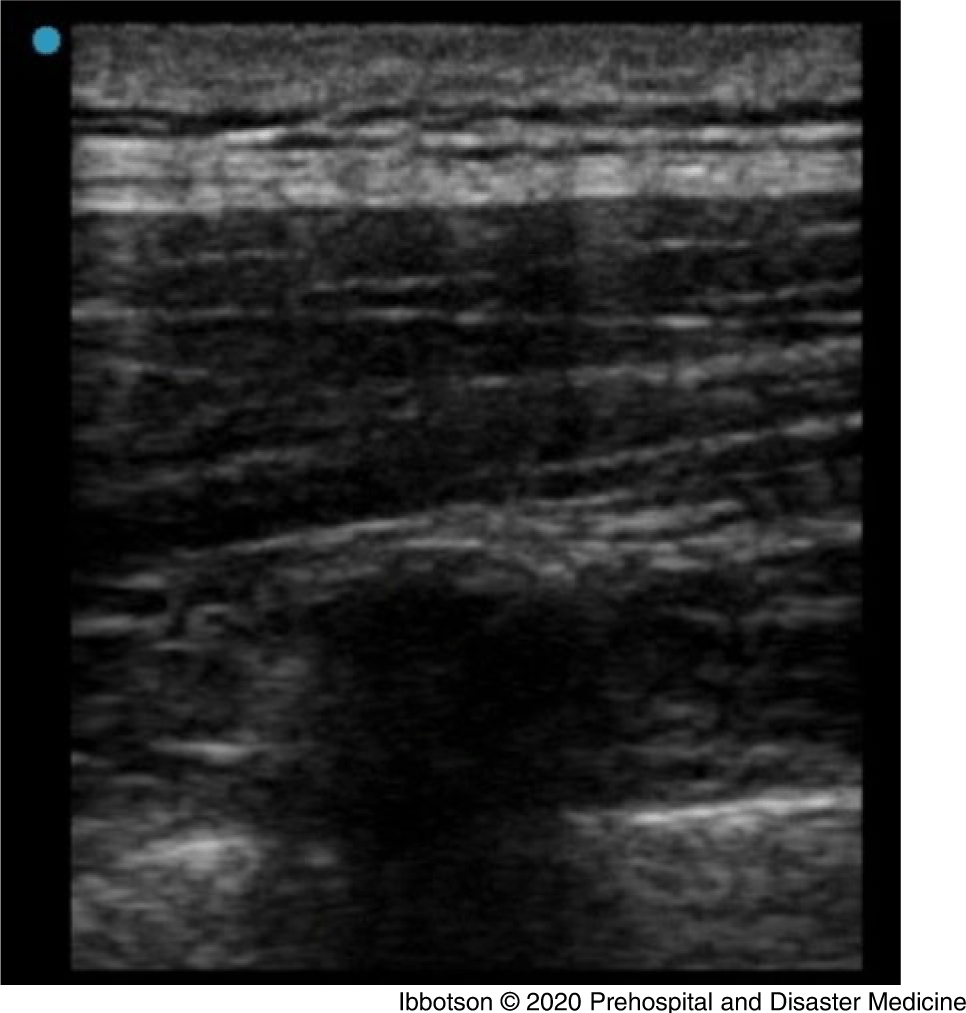
Figure 3. View of a Rib in the Longitudinal Parasagittal Orientation with a Linear 13-6MHz Probe. Note: Deep to the erector spinae muscle, the rib appears as a rounded acoustic shadow with underlying pleura.
Complications of the ESB are rare. The block is superficial and performed in an area without significant vascular structures. In-hospital use has been described in coagulopathic patients without complications.Reference Ayub, Talawar, Kumar, Bhoi and Singh9,Reference Adhikary, Prasad, Soleimani and Chin10 The underlying bony anatomy makes identification of the target area easy and protects underlying structures from damage should needle placement be off target. Reported complications include pneumothorax,Reference Ueshima11 incomplete blockade,Reference Ueshima and Otake12 and motor block.Reference Selvi and Tulgar13 Hematoma is also a theoretical complication, but has not been described in the literature. No complications were reported with either case published.
As with any use of ultrasound, performance of an ESB is an operator-dependent procedure. Different levels of training and clinical background my lead to different challenges and success rates in performing ESBs. Challenges while performing an ESB include: identification of anatomic structures in patients under spinal precautions, or with large body habitus, and maintaining continuous needle visualization.
Other alternative regional anesthetic procedures for rib fractures in-hospital include thoracic epidurals and paravertebral blocks. However, these blocks are more complex to perform in a retrieval environment, require a greater level of operator skill, are closer to vulnerable anatomic structures, and are contra-indicated in coagulopathic patients.
The use of serratus anterior block for chest traumaReference May, Hillermann and Patil14 has also been used in retrieval medicine;Reference McLean, Cooke, Burns and Reid4 however, it lacks coverage of the chest posterior to the mid axillary lineReference Durant, Dixon, Luftig, Mantuani and Herring15 and so may not provide analgesia to posterior rib fractures.
One case report from a military retrieval service reports a multi-injection ESB in a prolonged transfer of a patient with chest trauma.Reference Fabich, Greene, Tighe, Devasahayam and Becker16 In contrast, in this case series, a larger injection volume was used to reduce the technique to a single injection.
At the time of publication, no studies have been performed to assess the relative efficacy and safety of myofascial plane blocks (such as the ESB), so it is not possible to ascertain whether the ESB is superior to other forms of regional anesthesia.
Limitations
The provided data are a retrospective case series. Therefore, generalizing the information to other aeromedical services may be limited due to different settings, methods of transfer, distance of transfer, or level of expertise with ultrasound of the provider. Additional to this, reporting bias by the authors may exist. Therefore, the provided data should only be used to create the hypothesis that ESB are suitable blocks for the management of chest trauma in the aeromedical retrieval setting.
Conclusion
This case series demonstrate the successful use of single-injection ESBs in the aeromedical retrieval setting as part of multimodal analgesia. Further studies are required to assess the practicability and safety of ESBs in the management of pain from chest trauma during aeromedical retrievals.
Conflicts of interest
none







