Introduction
Mealtimes and dining with others in residential care (e.g., retirement home, assisted living, and long-term care homes) offer unique opportunities to foster a sense of community and reinforce residents’ autonomy through involvement in meaningful meal-related activities (Genoe et al., Reference Genoe, Dupuis, Keller, Martin, Cassolato and Edward2010; Gibbs-Ward & Keller, Reference Gibbs-Ward and Keller2005; Henkusens, Keller, Dupuis, & Schindel Martin, Reference Henkusens, Keller, Dupuis and Schindel Martin2014). The dining room is often the central focal point in many residential care homes, as this space and activity support the development and reinforcement of relationships amongst those who live and work in these homes, particularly for those residents living with dementia (Campo & Chaudhury, Reference Campo and Chaudhury2012). Family members and volunteers play critical roles in not only assisting residents with their meals (Durkin, Shotwell, & Simmons, Reference Durkin, Shotwell and Simmons2014; Wu et al., Reference Wu, Morrison-Koechl, Slaughter, Middleton, Carrier and McAiney2020), but also enriching the mealtime experience through familiar and comforting connections (Petersen, Wilson, Wright, Ward, & Capra, Reference Petersen, Wilson, Wright, Ward and Capra2016; Tsai, Tsai, Tsai, & Liao, Reference Tsai, Tsai, Tsai and Liao2020). Mealtimes with these features are consistent with a philosophy of relationship-centred care where relationships and interactions are integral to aspects of the caring process (Tresolini & Force, Reference Tresolini1994). Unlike person-centred care, relationship-centred care makes explicit the interdependence and reciprocal nature of caring relationships, where residents give just as much as they receive, and that such therapeutic relationships extend beyond those who live and work within homes to include family members and the greater community (Adams & Gardiner, Reference Adams and Gardiner2005; Nolan, Davies, Brown, Keady, & Nolan, Reference Nolan, Davies, Brown, Keady and Nolan2004). However, the “systemizing of meals” is often observed in research examining mealtimes in residential care, where task-focused meal processes are prioritized over relationship-centred care practices (Henkusens et al., Reference Henkusens, Keller, Dupuis and Schindel Martin2014) in response to restrictive government and home policies (Banerjee & Armstrong, Reference Banerjee and Armstrong2015; Lowndes, Daly, & Armstrong, Reference Lowndes, Daly and Armstrong2018).
The conditions of mealtimes described in the literature are often portrayed as highly regulated and rushed (Lowndes, Armstrong, & Daly, Reference Lowndes, Armstrong and Daly2015; Lowndes et al., Reference Lowndes, Daly and Armstrong2018). In some provinces and territories, compulsory resident charting of resident food and fluid intake into the Resident Assessment Instrument – Minimum Data Set (RAI-MDS 2.0) requires considerable time from staff, detracting from time spent with residents and families (Armstrong, Daly, & Choiniere, Reference Armstrong, Daly and Choiniere2016; Lowndes et al., Reference Lowndes, Armstrong and Daly2015). Further, regulations paired with contextual factors can result in essential task-focused meal processes being prioritized over dignified social care, such as relationship-centred care practices. For example, regulations stipulate that meals must begin and end within a certain time frame (e.g., dinner between 5:00 p.m. and 6:00 p.m.), that staff may support up to two residents at a time with eating assistance for safety reasons, and that residents should have sufficient time to eat at their own pace (e.g., Ministry of Health and Long-term Care, 2007). While such regulations are reasonable, the reality is that eating assistance requires additional time and dedicated support (Lee, Lee, & McConnell, Reference Lee, Lee and McConnell2021; Simmons & Schnelle, Reference Simmons and Schnelle2006) that are not always possible given such factors as the increasing complex care needs of residents and limited staffing (Chamberlain et al., Reference Chamberlain, Gruneir, Hoben, Squires, Cummings and Estabrooks2017; Hsu, Berta, Coyte, & Laporte, Reference Hsu, Berta, Coyte and Laporte2016; McGregor et al., Reference McGregor, Tate, McGrail, Ronald, Broemeling and Cohen2006). Consequently, staff assist more than two residents at a time, stopping and starting assistance while attending to other residents and mealtime tasks (Lowndes et al., Reference Lowndes, Daly and Armstrong2018). In some instances, staff have been observed resorting to unsafe eating assistance practices, including intimidation tactics and force feeding to ensure adequate food intake (Lowndes et al., Reference Lowndes, Daly and Armstrong2018; Österholm, Taghizadeh Larsson, & Olaison, Reference Österholm, Taghizadeh Larsson and Olaison2015; Palese et al., Reference Palese, Gonella, Kasa, Caruzzo, Hayter and Watson2019; Schiamberg et al., Reference Schiamberg, Oehmke, Zhang, Barboza, Griffore and von Heydrich2012). For residents, this can result in feelings of exclusion, loneliness, and objectification (Hung & Chaudhury, Reference Hung and Chaudhury2011; Lowndes et al., Reference Lowndes, Daly and Armstrong2018). Further, residents with significant cognitive impairment may experience meaningful social contact only at mealtimes (Adlbrecht, Bartholomeyczik, Hildebrandt, & Mayer, Reference Adlbrecht, Bartholomeyczik, Hildebrandt and Mayer2021). As mealtimes are a key point for relationship development, they have the capacity to improve the quality of life of residents, staff, families, and volunteers.
In early 2020, a pandemic swept through the world with coronavirus disease (COVID-19) disproportionately affecting the vulnerable, including those living in residential care (Canadian Institute for Health Information, 2020; Estabrooks et al., Reference Estabrooks, Straus, Flood, Keefe, Armstrong and Donner2020; Moser et al., Reference Moser, Pariser, Verma, Razak, Wong and Pus2020). Canada was no exception, with a high proportion of deaths from this sector during the first wave (Estabrooks et al., Reference Estabrooks, Straus, Flood, Keefe, Armstrong and Donner2020). This resulted in regulations to mitigate the spread of the infection. When comparing British Columbia and Ontario, it was noted that infection control procedures varied by region due to jurisdictional oversight (Liu et al., Reference Liu, Maxwell, Armstrong, Schwandt, Moser and McGregor2020). Common changes put in place regardless of an outbreak were confining residents to rooms; spreading residents throughout common areas for group activities (Anderson, Grey, Kennelly, & O’Neill, Reference Anderson, Grey, Kennelly and O’Neill2020); restricting staff to working in one home (Moser et al., Reference Moser, Pariser, Verma, Razak, Wong and Pus2020); limiting visits from family or volunteers (Canadian Institute for Health Information, 2020); non-essential health professionals providing virtual care or telecare (e.g., dietitians); and redeploying staff and other external supports (such as the military and hospital personnel) in order to provide direct care, such as eating assistance (Moser et al., Reference Moser, Pariser, Verma, Razak, Wong and Pus2020).
Guidance to mitigate the infectious spread of COVID-19 in the first wave changed frequently, resulting in variable practices (Estabrooks et al., Reference Estabrooks, Straus, Flood, Keefe, Armstrong and Donner2020; Moser et al., Reference Moser, Pariser, Verma, Razak, Wong and Pus2020), some of which are now viewed as having been overly restrictive. Variability among homes was specifically noted with respect to family involvement and visitation (Canadian Foundation for Healthcare Improvement & Canadian Patient Safety Institute, 2020), and their mandated exclusion from the home was controversial. Quality of life and dignity of care became an important ethical debate in social and print media, raising issues of guaranteed protections, proper staffing, and appropriate funding (Suárez-González, Reference Suárez-González2020). It is now known that these infection control procedures have a human cost, in the form of resident loneliness and depression, as well as loss of mental and physical functioning (Holt-Lunstad, Robles, & Sbarra, Reference Holt-Lunstad, Robles and Sbarra2017; Plagg, Engl, Piccoliori, & Eisendle, Reference Plagg, Engl, Piccoliori and Eisendle2020; Woo, Reference Woo2020). Staffing hours and shortages varied both geographically and by home characteristics prior to the pandemic; these variances were exacerbated by COVID-19 (Estabrooks et al., Reference Estabrooks, Straus, Flood, Keefe, Armstrong and Donner2020; Liu et al., Reference Liu, Maxwell, Armstrong, Schwandt, Moser and McGregor2020). It has been suggested that relationship-centred care practices may have afforded some benefits to residents during the pandemic (Estabrooks et al., Reference Estabrooks, Straus, Flood, Keefe, Armstrong and Donner2020). Certainly, some practices consistent with relationship-centred care, such as cohorting of residents and consistent staff assignment, were considered best practices to reduce the spread of the virus (Government of Canada, 2020). The built environment has also been identified as a key factor in the pandemic response and risk for infection and mortality (Estabrooks et al., Reference Estabrooks, Straus, Flood, Keefe, Armstrong and Donner2020). For example, if dining rooms were not deemed sufficient for physical distancing, they may have been closed, or plastic dividers put on tables to minimize risk of droplet contamination. Staff have reported conflict between balancing best practices, like relationship-centred care, with infection control procedures (Canadian Foundation for Healthcare Improvement & Canadian Patient Safety Institute, 2020).
To date, there is limited to no empirical knowledge of the impact of infection control procedures and the pandemic response on resident nutrition and mealtimes in residential care settings. One non-peer-reviewed report suggests that 13% of residents were eating in the dining room, while 64% were restricted to their rooms most of the time (Montgomery, Slocum, & Stanik, Reference Montgomery, Slocum and Stanik2020). There have also been non-empirical reports that have suggested that virtual visits with family could stimulate appetite (Hado & Friss Feinberg, Reference Hado and Friss Feinberg2020). Evidence on practice changes and their impacts on mealtimes and food intake are lacking. The purposes of this study were to 1) describe the change in mealtime practices in residential care as a result of the safety precautions, 2) describe providers’ perceptions of the most significant impact of infection control procedures and mandated policies on resident mealtimes, 3) assess providers’ feelings of conflict between safety and relationship-centred care, and 4) determine the factors (e.g., geographic regions, pre-pandemic relationship-centred vs. task-focused mealtime activities, participant and home characteristics, pandemic mealtime practices) independently associated with feeling conflict and reporting of top mealtime challenges.
Materials and Methods
Research funding was received to investigate perceptions of residential care providers on relationship-centred care in long-term care and retirement homes using an online survey. Since funding was received in the midst of the first wave of the pandemic in Canada and recognizing the importance of home responses to mandatory infection control procedures and the potential impacts on mealtimes, four questions related to COVID-19 responses were added to the survey. Broad reach and a high response rate were desired. Thus, the survey was limited in length (~12 minutes) to promote completion. The survey was open from July 8 to September 30, 2020, after the peak of the first wave of the pandemic in Canada.
Participant recruitment was based on snowball and convenience sampling. Stakeholder organizations in Canada (Dietitians of Canada; New Brunswick Association of Nursing Homes; Ontario Long-Term Care Action Group; Institute for Continuing Care Education and Research; Canadian Gerontological Nursing Association; Alberta Gerontological Nurses Association; Northern Alberta Dietitian Interest Group; AgeCare; Southern Alberta Continuing Care Dietitian Interest Group; Canadian Society of Nutrition Managers; Gordon Food Services; Sysco) and the United States (Association of Nutrition & Foodservice Professionals; Sysco) were invited to disseminate the online survey link to their networks and members. The authors, who represent various regions of Canada, also sent invitation e-mails to their provider/residential home networks and re-issued these invitations in August and September 2020. Multiple social media platforms were used to stimulate interest in the survey. There were no financial incentives for participation.
The online questionnaire was developed by the research and clinician team through several iterations and its functionality tested before release. Questionnaires were provided in English and French with an introductory statement and information about the purpose of the study and an explicit consent question. The first question used in this analysis rated participants’ satisfaction with the resident mealtime experience prior to COVID-19 (“very dissatisfied,” “dissatisfied,” “satisfied,” “very satisfied”). The second question asked participants to identify whether any of a list of 26 mealtime practices routinely occurred in their home’s dining room(s) before COVID-19. These items were based on the construct valid and reliable Mealtime Relational Care Checklist (Iuglio et al., Reference Iuglio, Chaudhury, Lengyel, Morrison, Boscart and Carrier2019). Participants were blinded to the identification of these practices as relationship-centred (15 items) or task-focused (11 items) to prevent social desirability bias. These items were summed into a relationship-centred score and task-focused score. Four COVID-19 response-specific questions were included. The first listed 20 diverse mealtime practices that either occurred before COVID-19 (e.g., food delivery method) or were initiated during the first wave of the pandemic (e.g., closing the dining room). Participants selected whether the practice had occurred before or was initiated during the pandemic. The second question asked participants to identify the greatest mealtime challenge that their home faced as a result of the pandemic; only one response was allowed from a list of 10 options (e.g., inadequate staffing, keeping food hot, reduced opportunity for residents to socialize at meals), with “other” being an option to gather participant-specific responses. An open text question asked respondents to provide any activities that their home had engaged in during the pandemic to promote social, enjoyable mealtimes for residents. The final COVID-19 response question asked respondents to indicate whether they felt conflicted while balancing safety and relationship-centred care for residents in their home (“yes,” “no,” “not sure”). The remaining items used in this analysis describe the respondent and their home’s characteristics. As per ethics requirements, participants could skip any question. The study was reviewed and clearance was provided by the University of Waterloo Research Ethics Board (ORE#42335)
Statistical Analysis
Descriptive analyses (mean, SD, proportions) were completed for each variable. As it was known that there was regional variation with respect to infection control procedures in homes, geographic location was used as an independent covariate in analyses, rather than a clustering factor. Due to the small sample from some provinces, logical groupings of regions were made. The Maritime provinces (Nova Scotia, New Brunswick, Prince Edward Island) were grouped together for analysis due to low numbers and the policy of the “Atlantic Bubble” during the first wave of the pandemic. Manitoba and Saskatchewan were also grouped together as these provinces are contiguous and experienced low levels of infection during the first wave. Two items were considered dependent variables in this analysis: 1) participants’ perception of the greatest mealtime challenge resulting from the pandemic, and 2) their feeling of conflict between relationship-centred care and safety. For bivariate and multivariable analyses, selection of any of the top four most frequently reported mealtime challenges was used as the outcome variable. For multivariable analyses, the following home and respondent characteristics and their subsequent categories were used as covariates: geographic location (British Columbia, Alberta, Saskatchewan/Manitoba, Ontario, Maritime provinces, United States), home size (≤ 49, 50-99, ≥ 100 beds), continuum of care (yes, no), part of a chain (yes, no), profit status (non-profit/municipal, for-profit), age of building (< 5, 5-10, 11-20, > 20 years), respondents’ level of satisfaction with residents’ mealtime experience pre-pandemic (very satisfied, satisfied, dissatisfied, very dissatisfied), and respondents’ job title (food/food service, direct care, other). The top four mealtime challenges reported, as well as initiation of mealtime pandemic practices were dichotomized as either selected or not selected for multivariable analyses.
IBM® SPSS® Statistics Version 26, Release 26.0.0.1 was used. Statistical significance for all analyses was determined by p < .050 unless otherwise specified. Only cases with complete data for variables in analyses were included; n values for analyses are specified in each table. The χ2 analyses were conducted to test bivariate associations with the outcome variables and for post-hoc analyses. If χ2 assumptions were violated (i.e., ≥ 20% of expected cell counts less than 5, or any expected cell count less than 1), the Fisher-Freeman-Halton exact test was reported. Adjusted standardized residuals were used as post-hoc testing for χ2 analyses (statistical significance determined by adjusted standardized residual > |1.96|; i.e., 97.5th percentile).
Independent sample t-tests were used to determine the association of selecting one of the top four mealtime challenges and both task-focused and relationship-centred care practices pre-pandemic; violations of Levene’s test of homoscedasticity resulted in reporting Welch’s t-test. A between-subjects analysis of variance (ANOVA) tested the association between a respondent’s level of satisfaction with mealtimes pre-pandemic and the relationship-centred care practices score with Games-Howell post-hoc testing. Two between-subjects ANOVAs were conducted to determine the level of conflict experienced balancing safety and relationship-centred care with both task-focused and relationship-centred care practices pre-pandemic, with Tukey’s test used for post-hoc analyses. Only bivariate analyses between the outcomes and satisfaction with mealtimes and relationship-centred and task-focused mealtime practices pre-pandemic are reported in the results.
Binary logistic regressions were completed for the top four mealtime challenges experienced with COVID-19 and covariates. Here, the focus was on determining the potentially different covariates associated with these mealtime challenges. For the outcome of experiencing conflict while balancing safety and relationship-centred practices (dichotomized to “yes” vs. “no/not sure”), we were interested in the specific variable groupings that contributed to the overall explained variance. For this latter analysis, a 5-step hierarchical binary logistic regression was completed. The first step tested geographic region, with remaining home and respondent characteristics added in the second step (home size, continuum of care, chain and profit affiliation, age of building, respondent job title, and level of satisfaction with residents’ mealtime experiences pre-pandemic). Pre-pandemic task and relationship-centred care scores were added in the third step, and the four mealtime challenges experienced with COVID-19 were added in the fourth step. The final fifth step included key pandemic-initiated practices.
Results
A total of 1,138 participants consented and entered the survey, and 1,036 (91.0%) completed at least the first question used in this analysis regarding their satisfaction with the resident mealtime experience (Table 1). Of those participants who provided their gender, almost all identified as a woman and 64.7% of respondents were over the age of 40. Almost one-third had worked in their current home for at least 11 years, and 73.6% worked in food and nutrition services (e.g., food service manager, dietitian, food service worker/cooks). The highest proportion of participants worked in Ontario (29.5%), while 16.7% worked in the United States. Homes of employment were large, with 56.9% being 100 or more beds and two-thirds being buildings older than 20 years. Approximately one-third of respondents worked in a for-profit home or a home that was part of a chain, with more than half being attached to a continuum of care (e.g., retirement, assisted-living). Pre-pandemic, 85.2% of respondents were satisfied (62.5%) or very satisfied (22.7%) with the resident mealtime experience in their home, while 11.3% and 3.5% were dissatisfied or very dissatisfied, respectively.
Table 1. Participant demographics and reported home characteristics

Table 2 reports specific relationship-centred and task-focused practices; the means for relationship-centred care (9.69, SD 2.96, max 15) and task-focused practices (4.89, SD 1.99, max 11) pre-pandemic were moderate to low, respectively. Pre-pandemic, common relationship-centred practices included addressing residents using their preferred names (90.2%) and making the dining room available outside of meals (79.7%). Common task-focused practices included team members not sharing the mealtime with residents (81.7%) and use of assigned seating (81.3%). The relationship-centred care practice score was significantly associated with respondents’ level of satisfaction with resident mealtimes pre-pandemic: F(3, 125.86) = 52.94, p < .001. Compared to dissatisfied respondents, respondents who were satisfied or very satisfied reported significantly higher relationship-centred care practices by 3.27 and 4.21 points, respectively (p < .001 for both). Respondents who were very satisfied reported 0.94 greater relationship-centred care practices than respondents who were just satisfied (p < .001), and respondents who were very dissatisfied reported 3.50 more relationship-centred care practices than respondents who were only dissatisfied (p < 0.001); however, caution should be taken when interpreting this result as only 3.5% of participants reported being very dissatisfied.
Table 2. Reported pre-pandemic mealtime practices (n = 922)

Table 3 outlines the pre-pandemic mealtime food delivery and care activities, and those initiated during the pandemic. Pre-pandemic, most respondents reported that residents ate in a dining room with a restaurant-style service with food plated at a servery or stationary steam table (63.9%). During the pandemic, more than 50% of respondents reported residents eating in their rooms and almost 30% had closed their dining rooms. Disposable dishware was reportedly initiated by more than 40% of homes. In-room dining was predominately supported by trays (53.2%), rather than a bulk mobile cart (11.6%). During the pandemic, more one-on-one assistance for eating was provided, and family/volunteer involvement was restricted due to mandated precautionary measures.
Table 3. Reported pre-pandemic mealtime practices and practices initiated during the pandemic

a n = 842 respondents
b n = 837 respondents
Table 4 provides the results of a content analysis based on 480 responses to the open text question where participants noted how they attempted to promote social interaction and enjoyable meals for residents during the first wave of the pandemic. These were categorized by type of activity/provision: staff meal participation, including more staff, staff socially interacting with residents (n = 94); new seating options, for example, capitalizing on friendships when planning for new two-resident tables (n = 83); meals in new locations throughout the home (n = 81); special menu items, including theme meals and special treats (n = 77); physical distancing for mealtimes, including using plexiglass barriers at tables (n = 64); music and entertainment, using poems as conversation starters (n = 58); management and other staff participating in providing the meal (n = 8); improved décor, such as use of center pieces or theme placemats and napkins (n = 7); rotational schedule for meal seating, either as twice per meal or rotating residents who dined in the dining room versus their own room (n = 5); and other, such as extended mealtimes (n = 3).
Table 4. Strategies described by participants to support social interaction and mealtime enjoyment (n = 480 responses)

Most Frequently Reported Mealtime Challenge During Wave One of the Pandemic
Respondents identified the greatest mealtime challenge in their home resulting from the pandemic to be: reduced opportunities for residents to socialize at meals (29.3%); inadequate staffing (22.8%); lack of family/volunteers to help at meals (16.7%); and assisting residents with eating (10.5%) (Table 5). In bivariate analyses, participants who chose inadequate staffing as their greatest challenge reported more task-focused practices: 5.35 ± 1.89 vs. 4.75 ± 1.98; t(830) = 3.72 p < .001; and fewer relationship-centred mealtime practices pre-pandemic: 9.12 ± 3.25 vs. 9.94 ± 2.76; t(273.02) = 3.17 p = .002. When reporting lack of family/volunteer help at meals as the greatest challenge, respondents also reported a higher mean score for task-focused practices: 5.21 ± 1.78 vs. 4.82 ± 2.01; t(830) = 2.10 p = .036. Participants who identified their greatest concern with the pandemic to be reduced opportunities for residents to socialize at meals reported a lower mean score for task-focused: 4.41 ± 1.96 vs. 5.08 ± 1.95; t(830) = 4.52 p < .001; and a higher mean score for relationship-centred mealtime practices, 10.34 ± 2.52 vs. 9.51 ± 3.01; t(535.66) = 4.08, p < .001 (pre-pandemic), than those who chose other areas of greatest concern. These differences between groups, although statistically significant, were generally small.
Table 5. Greatest mealtime challenge and level of conflict experienced balancing safety and relationship-centred care during the pandemic

In bivariate analysis, the main mealtime challenges of inadequate staffing and reduced opportunities for residents to socialize were significantly associated with level of satisfaction with residents’ mealtime experience pre-pandemic: χ2(3) = 8.69, p = .034; χ2(3) = 21.37, p < .001 (respectively). Significantly more respondents who were very dissatisfied with resident mealtimes pre-pandemic reported inadequate staffing as their primary challenge during the pandemic (adj. std. residual = 2.29). More respondents who selected the greatest pandemic mealtime challenge to be reduced opportunities for residents to socialize reported being very satisfied (adj. std. residual = 4.44) with residents’ pre-pandemic mealtime experience.
Binary logistic regressions for the four top mealtime challenges during the first wave of the pandemic reported by respondents are provided in Table 6. The binary logistic regression for the mealtime challenge of inadequate staffing was significant: χ2(30) = 63.09, p < .001; and the modeled covariates explained 8.6% of variance for this outcome. Every 1-point increase in the pre-pandemic relationship-centred mealtime care score was significantly associated with 10% reduced odds of selecting inadequate staffing as the primary challenge: χ2(1) = 7.01, p = .008, CI [0.83, 0.97]. However, those who reported starting volunteer/family mealtime support during the first wave of the pandemic (Table 3) had a 5.94 (CI [1.36, 25.91]) increased odds of selecting inadequate staffing as their greatest concern.
Table 6. Binary logistic regressions testing mealtime challenges experienced during the pandemic with home and respondent characteristics, and mealtime practices initiated during wave one of the pandemic
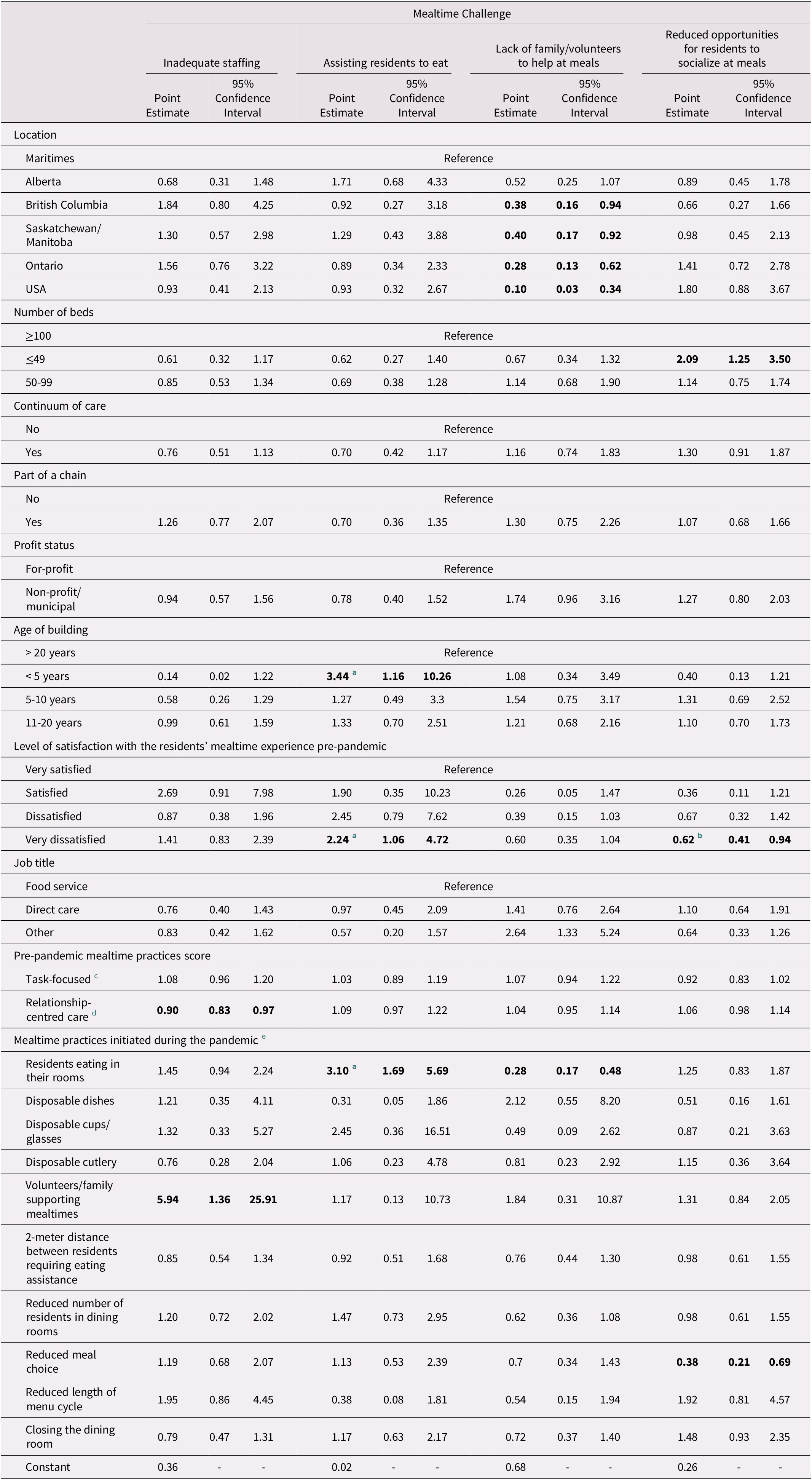
Note: Modeling the odds of experiencing one of the top four mealtime challenges; n = 704 for all models.
Statistical significance is indicated by bolded values.
a Overall model not statistically significant.
b Global effect not statistically significant.
c Sum of 11 practices.
d Sum of 15 practices.
e Versus not initiating this practice.
The model for assisting residents to eat was marginally non-significant, χ2(30) = 41.32, p = .082, and the modeled covariates explained 5.7% of variance for this outcome. Respondents working in buildings that were less than 5 years old had a 3.44 (CI [1.16, 10.26]) greater odds of choosing the challenge of assisting residents to eat as compared to homes that were in old (> 20 years) buildings. Those who were very dissatisfied with the mealtime experience pre-pandemic were also 2.24 (CI [1.06, 4.72]) times more likely to choose assisting residents to eat as the greatest challenge during the first wave of the pandemic, than those who were very satisfied with the mealtime experience. If the home used the pandemic strategy of residents eating in their rooms, respondents were 3.10 (CI [1.69, 5.69]) times more likely to choose this challenge of assisting residents to eat as their greatest challenge in the first wave of the pandemic.
The model reporting lack of family/volunteer help at meals as the greatest concern during the first wave of the pandemic was significant, χ2(30) = 107.31, p < .001, and the modeled covariates explained 14.1% of variance for this outcome. Respondents from British Columbia, Saskatchewan/Manitoba, Ontario, and the United States had significantly lower odds of selecting this challenge by 62%, 60%, 72%, and 90%, respectively, as compared to respondents from the Maritimes, χ2(5) = 18.09, p = .003. Respondents with “other” job titles (e.g., allied health, other management) were 2.64 (CI [1.33, 5.24]) times more likely to select this challenge versus food/food service related staff, χ2(2) = 7.96, p = .019. Having residents eat in their rooms because of the pandemic was associated with significantly lower odds of selecting this challenge by 72%: χ2(1) = 21.83, p < .001, CI [0.17, 0.48].
The model testing key covariates for the challenge of reduced opportunities for residents to socialize at meals was significant, χ2(29) = 80.02, p < .001, and the modeled covariates explained 11.6% of variance for this outcome. The odds of respondents from smaller homes (≤ 49 beds) reporting this challenge were higher by 2.09 times as compared to large homes (≥ 100 beds): χ2(2) = 7.93, p = .019, CI [1.25, 3.50]. Respondents who indicated that they were very dissatisfied with resident mealtime experiences pre-pandemic were 38% less likely to choose reduced social opportunities for residents as their greatest concern as compared to those who were very satisfied with resident mealtime experiences pre-pandemic. Finally, those who initiated reduced food choice for residents had reduced odds of selecting low resident socialization as their main concern as a result of pandemic procedures during the first wave: χ2(1) = 10.16, p = .001, CI [0.21, 0.69].
Feelings of Conflict Between Relationship-Centred Care and Safety
More than 70% of participants reported feeling conflicted balancing safety and relationship-centred care for residents in their home during the pandemic, with 9.8% being unsure (see Table 5). Respondents’ level of conflict with balancing safety and relationship-centred care was associated with satisfaction with residents’ pre-pandemic mealtime experience in bivariate analyses: χ2(6) = 24.28, p <.001. Those dissatisfied with the mealtime experience pre-pandemic were more likely to report feeling conflict (adj. std. residuals = 2.85, -3.32), and those satisfied with the pre-pandemic mealtime experience were less likely to report this conflict (adj. std. residuals = -3.72, 3.34). Task-focused and relationship-centred practice scores were associated with feelings of conflict: F(2, 833) = 3.45, p = .032; F(2, 833) = 7.65, p = .001. Conflicted respondents reported more task-focused practices pre-pandemic than non-conflicted respondents (4.98 ± 1.97 vs. 4.51 ± 1.99; p = .024) in bivariate analyses. Those who experienced no conflict reported more relationship-centred practices pre-pandemic (10.48 ± 2.69) than those who felt conflicted (9.68 ± 2.89) or were unsure (9.02 ± 2.98) in bivariate analyses (p = .006; p < .001). Although statistically significant, differences between groups were small.
The multivariable model for this outcome of experiencing conflict in balancing safety and relationship-centred care during the pandemic was statistically significant: χ2(34) = 73.07, p = < .001, and is provided in Table 7. Geographic location (step 1), home characteristics, respondent job title, and level of satisfaction with residents’ mealtime experience pre-pandemic (step 2), task-focused and relationship-centred care mealtime practices pre-pandemic (step 3), the four key mealtime challenges experienced during the pandemic (step 4), and mealtime-related pandemic practices initiated (step 5) explained 3.2%, 2.9%, 0.0%, 0.2%, and 4.6%, respectively, of additional variance following each step, resulting in a total of 10.7% of total explained variance. Respondents from Alberta and Saskatchewan/Manitoba were 2.80 and 3.04, times more likely to feel conflicted versus respondents from the Maritimes: χ2(5) = 14.38; p = .013, CIs [1.15, 6.81], [1.06, 8.69]. Feeling dissatisfied or very dissatisfied with residents’ mealtime experience pre-pandemic was significantly associated with higher odds of reporting feeling conflicted by 5.72 or 1.70 times, respectively, as compared to respondents who felt very satisfied with the resident mealtime experience: χ2(3) = 9.49; p = .023, CIs [1.76, 18.54], [1.02, 2.82]. Having residents eat in their rooms during the pandemic was significantly associated with respondents reporting conflict while balancing safety and relationship-centred care, with the odds of experiencing conflict being 2.21 higher for those who indicated this practice was put into place during the first wave of the pandemic: χ2(1) = 9.57; p = .002, CI [1.34, 3.65]. Volunteer/family support being initiated at meals during the pandemic was associated with being less likely to experience conflict by 85%: χ2(1) = 5.96; p = .015, CI [0.03, 0.69].
Table 7. Binary logistic regression testing associations between respondent conflict balancing safety and relationship-centred care during the pandemic with home and resident characteristics, common mealtime challenges, and mealtime practices initiated during the first wave

Note: Table is for the final step of the hierarchical binary logistic regression. Modeling the odds of experiencing conflict while balancing safety and relationship-centred care practices during the COVID-19 pandemic, Yes versus No, n = 626.
Statistical significance is indicated by bolded values.
a Sum of 11 practices.
b Sum of 15 practices.
c Versus not selecting this as the primary mealtime challenge during COVID-19.
d Versus not initiating this practice.
Discussion
During the first wave of the COVID-19 pandemic in North America (e.g., March–June 2020), several precautionary safety measures to limit the spread of the virus were put into place that altered mealtimes for older adults in residential care. These changes had the capacity to negatively impact residents, including their food intake and quality of life. Some of the most common pandemic strategies were having residents eat in their rooms and physically distancing during meals. Not surprising then, respondents noted that the greatest challenge for resident mealtimes was the reduced social interactions available during meals. Furthermore, over 70% of respondents felt conflicted about the balance between relationship-centred care and safety procedures due to the pandemic. This is consistent with prior qualitative findings that staff felt conflict during the first wave of COVID-19 (Canadian Foundation for Healthcare Improvement & Canadian Patient Safety Institute, 2020). Participants reported more relationship-centred practices than task-focused practices at mealtimes (see Table 2) prior to the pandemic, which is consistent with prior work (Iuglio et al., Reference Iuglio, Chaudhury, Lengyel, Morrison, Boscart and Carrier2019). In bivariate analyses, respondents working in homes with higher mean scores for relationship-centred care practices at mealtimes before the pandemic reported lack of socialization of residents at meals as their greatest concern as compared to those with a higher mean score for task-focused mealtime practices. However, respondents reporting higher mean scores for relationship-centred practices pre-pandemic were more likely to not feel conflict in bivariate analyses, suggesting that their home’s organizational culture and care philosophy was a potential protective factor supporting residents’ relationships and social interactions during this time. Relationship-centred mealtimes are an essential practice as we move forward with COVID-19 and other infectious diseases in residential care (Wee & Yap, Reference Wee and Yap2020). Professional organizations, such as Dietitians of Canada and the Canadian Gerontological Nursing Association, have created Best Practices and standards and competencies, respectively, that denote the importance of the mealtime experience and the specialized training required to promote pleasurable dining experiences and relational care (Dietitians of Canada, 2019; Gerontological Nursing Standards of Practice and Competencies, 2020).
Feeling conflict between balancing relationship-centred care and safety was predicted by several covariates in multivariable analyses. Respondents from Alberta and Saskatchewan/Manitoba were more likely to feel conflict as compared to the Maritime provinces. These provinces during the first wave had few cases of COVID-19 in the community as well as in residential care. This association may reflect community perspectives on the necessity for protective procedures or attitudes towards the no visitor/volunteer policy put into place in the first wave in homes in Alberta, Saskatchewan, and Manitoba. Those dissatisfied with the resident mealtime experience pre-pandemic also had higher odds of experiencing this conflict. It can be hypothesized that homes that prioritized the resident mealtime experience pre-pandemic (i.e., respondents satisfied with the resident mealtime experience) found ways to address the safety guidance required with the pandemic while maintaining some semblance of relationship-centred practices in the home. Certainly, bivariate analyses demonstrated that those with high pre-pandemic relationship-centred scores were more likely to be satisfied with resident meals. Two post-pandemic changes in mealtime practices were also associated with an increased likelihood of respondents feeling conflict between relationship-centred care and safety. Residents eating in their rooms was reported pre-pandemic by 15.7% of respondents but more than half reported this practice occurring during the pandemic. This practice was associated with feeling more conflict between relationship-centred care and pandemic safety procedures. Eating alone in one’s room would result in minimal interaction with staff and no interaction with visitors and other residents. Outside of a personal television, tablet/computer/phone, entertainment and communications would be limited. Thus, it is not surprising that those respondents who noted residents eating alone in one’s room reported feeling conflict between relationship-centred care and safety procedures.
Volunteers/staff to assist with mealtimes as a post-pandemic practice was negatively associated with feelings of conflict between safety and relationship-centred care. Respondents who reported the initiation of volunteer/staff assisting at mealtimes during the pandemic felt less conflict. This practice was reported by very few respondents (1.3%), as exclusion of volunteers and family from homes was a common precautionary measure during the first wave. Respondents reporting this activity were most often from Ontario, which experienced high levels of infection and deaths in residential care during the first wave of the pandemic. There was considerable concern and conflict over the exclusion of volunteers and family members from homes during the first wave (Canadian Foundation for Healthcare Improvement & Canadian Patient Safety Institute, 2020; Comas-Herrera et al., Reference Comas-Herrera, Salcher-Knorad, Baumbusch, Farina, Goodman, Lorenz-Dant and Low2020). Respondents from the very few homes that allowed visitors to support meals appear to have felt that this measure promoted relationship-centred care in the home. It is worth considering how visitors who specifically come into the home to support residents with eating could be continued, as it is an essential care activity. As noted in this survey, lacking family/volunteer support at meals for eating assistance was the third most common mealtime challenge reported.
More than 20% of respondents indicated that their greatest challenge during the first wave was either lack of resident socialization during meals or inadequate staffing. The other two greatest challenges were also focused on care needs: lacking family/volunteer support at meals and inadequate assistance for helping residents to eat. Inadequate direct care and dietary staff during the pandemic have been previously reported (Comas-Herrera et al., Reference Comas-Herrera, Salcher-Knorad, Baumbusch, Farina, Goodman, Lorenz-Dant and Low2020; Estabrooks et al., Reference Estabrooks, Straus, Flood, Keefe, Armstrong and Donner2020). When personnel are suspected to have COVID-19 or test positive and need to isolate or recover until symptoms are resolved, inadequate numbers of staff can result. Regulations were also put into place early in the pandemic requiring staff to limit their work to a single home, potentially resulting in a shortage of staff (Moser et al., Reference Moser, Pariser, Verma, Razak, Wong and Pus2020). The policy to limit visitors, which was common in Canada (Canadian Foundation for Healthcare Improvement & Canadian Patient Safety Institute, 2020), resulted in a sudden reduction in help with care activities, including meals. In our study, the challenge of inadequate staff was negatively associated with having a higher mean score for relationship-centred practices at mealtimes pre-pandemic in multivariable analyses. It could be hypothesized that homes with a more relationship-centred focus took an “all-hands-on- deck” (see Table 4) approach to mealtime care, where management, allied health care, and administrative staff were purposefully included in mealtimes to promote social interaction and an enjoyable meal. Inadequate staffing at meals was highly and positively associated with having volunteers/family involvement at meals initiated during the pandemic. It can be hypothesized that being especially concerned about staffing levels resulted in sourcing support from family/volunteers at meals, although it is unclear when or how this was achieved. Certainly, during the first wave of the pandemic, there was considerable family concern about being prevented from entering homes and supporting their loved ones. As the survey was available until the end of September, and visiting policies changed during that time, regulations may have supported family presence at mealtimes for selected residents and homes. Effort should be made to determine how essential family care providers can be in the home during a pandemic, as research has shown that residents eat more with assistance from a family member as compared to staff (Wu et al., Reference Wu, Morrison-Koechl, Slaughter, Middleton, Carrier and McAiney2020).
Respondents who indicated that lack of volunteers/family was their greatest challenge varied by region. The Maritimes experienced a bubble that limited exposure to the virus during the first wave of the pandemic. Maritime provinces were more likely to choose lack of volunteers/family as the greatest challenge compared to other provinces and the United States. The only exception was Alberta. This could suggest that the Maritime provinces had minimal pandemic-related challenges with staffing and were able to preserve social interactions at meals, thus they did not choose these as challenges. A structural difference among regions was size of home that respondents worked in. Post-hoc bivariates identified that size of home was associated with region, χ2(10) = 78.11, p < .001, with significantly more respondents from Ontario working in homes with ≥ 100 beds (adj. std. residual = 5.19), and fewer respondents from Alberta, Manitoba/Saskatchewan, and the United States worked in these larger homes (adj. std. residuals = -2.05, -3.41, -2.60). Furthermore, homes and regions varied in their social restrictions, including family visiting (Canadian Foundation for Healthcare Improvement & Canadian Patient Safety Institute, 2020). Non-food service/nutrition respondents were also more likely to identify lack of family/volunteers at mealtimes as the greatest challenge. This may have been due to direct experience and filling in for absent family members at meals, as staff from other areas were redeployed to direct care activities, including assisting with eating (Moser et al., Reference Moser, Pariser, Verma, Razak, Wong and Pus2020). Further, residents eating in their rooms was negatively associated with respondents identifying lack of family/volunteer meal support as the greatest challenge. Inadequate assistance for eating meals while residents were in their rooms, as noted below, was more likely to result from this pandemic practice.
Inadequate support for resident eating assistance was positively associated with residents eating in their rooms in multivariable analyses. Eating assistance is a time-intensive activity, and a typical practice is to have one staff member assisting two residents at the same time. This survey also found an increase in the proportion of respondents reporting that one-on-one assistance for eating occurred during the pandemic (see Table 3). The policy to physically distance residents during meals or assist residents in their rooms may explain this association in the multivariable analysis. Prior research has shown that requiring eating assistance is associated with a poorer mealtime experience (Iuglio et al., Reference Iuglio, Chaudhury, Lengyel, Morrison, Boscart and Carrier2019; Palese et al., Reference Palese, Gonella, Kasa, Caruzzo, Hayter and Watson2019), so it was not surprising to find an association between being dissatisfied with the resident mealtime experience pre-pandemic and choosing inadequate eating assistance as the greatest pandemic challenge. Respondents from homes that were built less than five years ago were also more likely to indicate that having inadequate eating assistance was the greatest mealtime challenge of the pandemic. Post-hoc bivariate analyses identified that profit status was associated with building age and size: χ2(3) = 11.76, p = .008; χ2(2) = 17.20, p < .001. Significantly more respondents working in for-profit homes worked in homes with 50-99 beds while significantly fewer worked in homes with ≤ 49 beds (adj. std. residuals = 2.36, -3.91). Also, more respondents working in for-profit homes reported their home was built within the past 5-10 or 11-20 years (adj. std. residuals = 1.99, 2.04), while significantly fewer were built ≥ 20 years ago (adj. std. residual = -3.39). These associations may suggest differences in staffing levels in these homes or other structural differences, such as size of home, that led to participants choosing inadequate eating assistance as their greatest pandemic challenge.
The most common mealtime challenge reported by respondents was reduced opportunities for resident social interaction at mealtimes (29.3%; see Table 4). Multivariable analysis identified that respondents from small homes (< 50 beds) as compared to large homes (≥ 100 beds) reported lack of resident social interaction as their greatest mealtime challenge. Small homes are more likely to have only one dining room that may not have been able to accommodate all residents while physically distancing. In smaller homes, there may also be fewer recreation staff and other opportunities for social interaction, as compared to larger homes. Being very dissatisfied as compared to satisfied with the resident mealtime experience pre-pandemic was negatively associated with choosing the loss of social aspects of mealtimes as the greatest challenge. We can hypothesize that respondents who were dissatisfied with mealtimes pre-pandemic were in homes where mealtimes were not as socially engaging for residents, and thus did not view the loss of social interaction as the biggest challenge. Finally, respondents were less likely to identify inadequate resident social interaction at meals as a challenge when they put into place the pandemic practice of reduced meal options. It can be hypothesized that reducing meal choices during the first wave was consistent with homes that had not fully embraced a relationship-centred care philosophy. An alternative hypothesis could be that these homes that reduced meal options could not maintain this mealtime person-centred practice due to the effects of the pandemic (e.g., losing staff due to infection). For these homes, their concerns for safety would have been paramount, and getting a meal provided to residents may have been their greatest concern. Finally, it could be hypothesized that these homes had inadequate structural supports such as hot mobile carts for resident-room food delivery that would have supported food choice. Hot mobile carts were used by a minority during the first wave of the pandemic.
This study is not without limitations. As the purpose of this survey originally did not include COVID-19, the number of questions that could be asked was limited. In addition, to achieve a high response rate for providers, the survey needed to be as short as possible. As a result, relatively few covariates that could explain the outcome variables were included, resulting in a modest variance in outcomes explained. Future work attempting to understand the conflict providers may feel between safety and relationship-centred care practices could include other covariates such as staffing ratios, proportion of residents with moderate or severe dementia, staff training, and other practices like consistent team member assignment. Respondents may not have been in their home during the height of the pandemic if they were considered non-essential staff; their perspective may be based on the report of others rather than their direct experience. We cannot extrapolate these findings to food intake, and further work should be done to determine the potential impact of precautionary measures on nutritional status. The dissemination strategy focused on food and nutrition services; as a result, most participants were food service managers, dietitians, or dietary staff, thus findings reflect these perspectives. As a result, a broader perspective on the impact of COVID-19 on mealtimes is not available, including nursing staff, residents, and family. Some provinces/territories of Canada were poorly represented, especially Quebec, which was a hot spot for COVID-19 in residential care at the time of survey administration. Perspectives from this group especially would have been relevant for helping identify better practices that supported resident mealtimes. As the sample is based on individual respondents, the number of homes represented by these data is not specifically known. Further, respondents cannot be considered to represent the region where they worked. While we have hypothesized possible reasons for the identified significant associations, this was a cross-sectional survey, and causality, and mechanisms of effect cannot be clearly established; as such, this analysis should be considered exploratory. Finally, as a result of the ethics requirement, not all questions were answered by all participants; most data missing occurred with participant demographics; there was the potential for these non-completers to be different from completers, and, as a result, we chose not to impute these data. Regardless, this very large sample was diverse, reporting from several provinces in Canada and with a good portion of respondents (16.7%) from the United States.
Conclusions
COVID-19 restrictions promoting physical distancing and other infection control procedures during the first wave in North America highlighted long-standing, pre-pandemic deficits in residential care (Moser et al., Reference Moser, Pariser, Verma, Razak, Wong and Pus2020). As shown in this study, pandemic precautions impacted mealtime practices resulting in concern for lack of resident social interactions at meals, inadequate staffing, inadequate assistance for residents who required eating assistance, and lack of family/volunteer involvement at meals. Providers felt conflicted between trying to keep residents safe and promoting relationship-centred care. Limiting residents to their rooms for meals should be a “last resort” measure, such as during an outbreak in a specific neighbourhood or unit. Training and supporting homes to develop relationship-centred practices is a best practice strategy that may evolve from the experience with COVID-19 (Woo, Reference Woo2020). Practical tools to support staff with prioritizing social interactions with residents are needed. Teams need to be able to practice and prioritize work so that, during outbreaks or in periods of short staffing, these essential practices of socialization, including eating with others, remain a top priority. Volunteers and family need to be seen as vital care providers who can support mealtimes (Comas-Herrera et al., Reference Comas-Herrera, Salcher-Knorad, Baumbusch, Farina, Goodman, Lorenz-Dant and Low2020; Wu et al., Reference Wu, Morrison-Koechl, Slaughter, Middleton, Carrier and McAiney2020). Understanding how the pandemic safety measures impacted resident quality of life and nutritional status should be the objective of future work to understand what was necessary and useful versus those strategies that were potentially harmful (Suárez-González, Reference Suárez-González2020).
Acknowledgements
The authors wish to acknowledge the following organizations that supported dissemination of the notice of the survey: Dietitians of Canada, Ontario Long-Term Care Action Group; New Brunswick Association of Nursing Homes; Institute for Continuing Care Education and Research; Canadian Gerontological Nurses Association; Alberta Gerontological Nurses Association; Northern Alberta Dietitian Interest Group; AgeCare; Schlegel-UW Research Institute for Aging; Schlegel Villages; Southern Alberta Continuing Care Dietitian Interest Group; Canadian Society of Nutrition Managers; Gordon Food Services; Sysco; and the Association of Nutrition & Foodservice Professionals. The authors also acknowledge the technical support of Cindy Wei for the Qualtrics survey development and administration.
Author Contributions
Conceptualization, HK, AC, SES, CL, HMO, NC, NR, SB, SQ, and SAW; methodology, HK, AC, SES, CL, HMO, NC, NR, SB, SQ, and SAW; formal analysis, VT and HD; writing—original draft preparation, HK and VT; writing—review and editing, AC, SES, CL, HMO, NC, NR, SB, SQ, SAW, and HD; funding acquisition, HK, AC, SES, CL, HMO, NC, NR, and SQ. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Social Sciences and Humanities Research Council, file number 892-2020-0044. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
The study was reviewed by a University of Waterloo ethics board and received clearance (ORE#42335).












