5.1 Introduction
The main aim of this chapter is to discuss linkages between nature and generic health from a One Health as well as transformative biodiversity governance perspective. Due to the COVID-19 pandemic, the interest in the linkages between nature and human health has increased drastically, in general but also in the biodiversity realm. The origin of the virus is still under investigation, but Reference Haider, Rothman-Ostrow and OsmanHaider et al. (2020) propose classifying COVID-19 as an “emerging infectious disease of probable animal origin.” The tens of millions of human COVID-19 infections reported internationally appear to have primarily emerged through human-to-human transmission. Thus, amidst the pandemic, the potential animal origin is of secondary interest for further containment of the disease. Still, in the public and international governance debate for example in the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services (Reference Daszak, Neves and AmuasiIPBES, 2020), a link is clearly made between zoonotic infectious diseases and the effects of human pressures on ecosystems. The dissemination of the virus, facilitated by intense global travel and high local connectivity, should also cause us to question our understanding of the fragilities of human health in a globalized world.
Early foundational steps regarding nature–human health linkages were present in the World Health Organization’s (WHO’s) contribution to the Millennium Ecosystem Assessment (WHO, 2005) and the State of Knowledge Review that was jointly produced by the Convention on Biological Diversity (CBD) and WHO (WHO-CBD, 2015). Until recently, however, for many in the biodiversity domain, linkages with human health were little known or taken into account in science, policy and practice. The concept of One Health is now often mentioned as a “silver bullet” solution to challenges like the COVID-19 pandemic (e.g. Reference Daszak, Neves and AmuasiIPBES, 2020). More or less in the background, One Health has been around for quite some time, including in the WHO-CBD knowledge review (2015), where it was proposed as an overarching concept for biodiversity and health governance. The concept was supported by the CBD member states in the final declaration of the Conference of the Parties in 2018, which “Invites Parties and other Governments to consider integrating One Health policies, plans or projects, and other holistic approaches in their national biodiversity strategies and action plans, and, as appropriate, national health plans” (CBD, 2018). But what does One Health entail, or rather, what can it entail, as we can question whether the beauty of One Health is the same in the eyes of many beholders? We do not have the ambition to present an exhaustive overview of nature–human health linkages or of One Health. We aim to discuss key aspects and challenges of One Health, highlight definitional diversity, and in doing so hope to give inspiration for transformative biodiversity governance.
5.2 Understanding the Concept of One Health
5.2.1 Biodiversity and Health
From the perspective of nature’s contributions to people (see Chapter 2 for more details on definitions of nature), it may seem that human health is only one of many elements of the ways in which nature and biodiversity can contribute to human well-being. This is illustrated by the fact that in modern scientific literature on the conceptual and operational development of the concept of ecosystem services, health is often “only” considered to be a subsection of cultural values (Reference Bryce, Irvine and ChurchBryce et al., 2016; Reference Bullock, Joyce and CollierBullock et al., 2018), or is even absent (Reference Cheng, Van Damme, Li and UyttenhoveCheng et al., 2019). An explanation is that the concept emerged in the realm of biological sciences, with biologists trying to link the importance of “their world” to societal relevance, with as a main first step economic valuation (Reference Ring, Hansjürgens, Elmqvist, Wittmer and SukhdevRing et al., 2010). This is the same the other way around: Until recently the word “ecology” in the health sector often had limited reference to nature, but rather to the social or societal environment of a patient (Reference Hoffmann, Ristl, George, Maier and PichlhöferHoffmann et al., 2019; Reference WhiteWhite, 1997), and nature was only considered to a limited extent in, for example, primary health care (Reference Lauwers, Bastiaens, Remmen and KeuneLauwers et al., 2020), and even the concept of “green prescription” initially had few linkages with nature, but mainly referred to environmental pollution and climate change challenges, lifestyle and nonmedicinal prescriptions (Reference Anderson, Taylor, Grant, Fulton and HofmanAnderson et al., 2015; Reference Patel, Schofield and KoltPatel et al., 2011; Reference Swinburn, Walter, Arroll, Tilyard and RussellSwinburn et al., 1997). A prominent exception is the WHO Ottawa Charter on Health Promotion (WHO, 1986: 1), which has highlighted the importance of a stable ecosystem: “The fundamental conditions and resources for health are peace, shelter, education, food, income, a stable ecosystem, sustainable resources, social justice and equity. Improvement in health requires a secure foundation in these basic prerequisites.” Apart from this example, the (more tangible) negative drivers relating to environment, like pollution, have dominated. There was relatively little discussion on the positive and negative contributions of ecosystems and biodiversity.
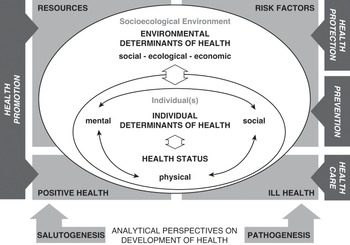
The mechanisms linking nature and biodiversity on the one hand and human health on the other are complex and intertwined, and can result in human health benefits and risks (IPBES, 2018a; WHO-CBD, 2015). Figure 5.1 (Reference Marselle, Hartig and CoxMarselle et al., 2021) shows how biodiversity and human health and well-being are related through diverse pathways and a wide array of moderating factors.
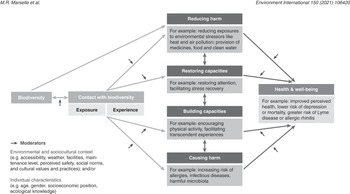
Figure 5.1 Pathways linking biodiversity to human health
Biodiversity supports the ecosystem services that mitigate heat, noise and air pollution, which all mediate the positive health effects of green spaces (see Chapter 14). In the topical domain of medicinal plants, significant work has been done regarding biodiversity and health, including a vast body of Indigenous traditional knowledge (Reference Rounsevell, Fischer, Torre-Marin Rando and MaderIPBES, 2018b; WHO-CBD, 2015). In more mainstream contemporary environmental health science, direct health outcomes of biodiversity have been understudied and underverified so far. There is evidence for positive associations between species and ecosystem diversity, and psychological and physical well-being and immune system regulation. There is more evidence for self-reported psychological well-being than for well-defined clinical outcomes. High biodiversity has been associated with both reduced and increased vector-borne disease risk (Reference Aerts, Honnay and Van NieuwenhuyseAerts et al., 2018).
Ecosystem change is recognized as a risk factor for disease emergence and spread, but a specific role for biodiversity is not always clear. Biodiversity may reduce disease risk by what is called the dilution effect. The dilution effect hypothesis proposes that high vertebrate species richness reduces the risk of infectious diseases among humans because pathogens are “diluted” among a high number of animal reservoir species that differ in their capacity to infect invertebrate vector species (Reference Schmidt and OstfeldSchmidt and Ostfeld, 2001). Under the dilution effect hypothesis, the transmission and burden of infectious diseases are expected to be lower in animal species-rich, natural environments through lower infection prevalence in vectors (Reference Johnson, Hitchens and Smiley EvansJohnson et al., 2015; Reference Ostfeld and KeesingOstfeld and Keesing, 2017), even when higher species richness also implies higher pathogen richness (Reference Dunn, Davies, Harris and GavinDunn et al., 2010). However, factors such as species composition, persistence of contacts between reservoirs and vectors, and the various ways in which reservoirs and nonreservoirs are affected by environmental change may all affect the dilution mechanism. The amplification effect, in which the infection prevalence in vectors increases following an environmental change affecting biodiversity, has also been observed (Reference Faust, Dobson and GottdenkerFaust et al., 2017). The conditions in which dilution or amplification will be observed are still the object of research (Reference Johnson, Hitchens and Smiley EvansJohnson et al., 2015; Reference Kilpatrick, Dobson and LeviKilpatrick et al., 2017; Reference Morand and HurstMorand, 2018). However, it has been established that the risk of disease spread appears higher in human-dominated and simplified habitats (Reference Morand and HurstMorand, 2018). Habitat fragmentation affects both pathogen diversity and pathogen prevalence. The perturbation hypothesis holds that if a habitat is fragmented, the sum of fragments will not be able to sustain the same diversity and prevalence of pathogenic species (but also reservoirs and vectors) as the original habitat (Reference Murray and DaszakMurray and Daszak, 2013). However, fragmentation also leads to a longer boundary between the habitat(s) and those of other communities. This in turn increases the chance of encounters between communities of hosts and vectors. The pathogen pool diversity hypothesis thus assumes that this intensified interaction raises the transmission of pathogens between habitats and species, and within populations. Hence, ongoing habitat fragmentation may both decrease and increase disease transmission risk. Beyond fragmentation, the ongoing “Anthropocene defaunation” leads to almost empty tropical forests (Reference Dirzo, Young and GalettiDirzo et al., 2014). The sharp decline of many animal populations has dramatic implications for zoonotic diseases, by both decreasing and increasing transmission risks. As the diversity of host populations decreases, so will the diversity of the microbes (including pathogens) they harbor. Decreasing host diversity means the loss of important interspecific regulations provided by predation or competition. The remaining pathogens hosted by more abundant but less diverse hosts or vectors released from competition or predation show enhanced transmission. This is particularly evident for pathogens able to switch host species easily and those living in synanthropic species such as rodents or some mosquito vectors. The recent study by Reference Gibb, Redding and ChinGibb et al. (2020) demonstrates how global land-use changes favor zoonotic reservoirs and increase the risks of zoonotic diseases, and more specifically in Southeast Asian environments with critical ongoing defaunation (Reference Morand and HurstMorand, 2018).
5.2.2 Integrative Concepts
Integrative approaches to health have quite a long history. The WHO Constitution in 1946 envisioned a comprehensive view of health: “health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (WHO, 2006: 1). In the WHO meeting in Alma-Ata (today Almaty, Kazakhstan) in 1978, a holistic and intersectoral conceptualization of health assumed importance: “[health] involves, in addition to the health sector, all related sectors and aspects of national and community development, in particular agriculture, animal husbandry, food, industry, education, housing, public works, communications and other sectors; and demands the coordinated efforts of all those sectors” (WHO, 1978: 2). As mentioned above, in 1986, the WHO Ottawa Charter for Health Promotion highlighted the need for a stable ecosystem as a basis for good health (WHO, 1986). In 2002, the World Summit on Sustainable Development initiated the foundation for an inclusive framework: WEHAB (Water, Energy, Health, Agriculture [food, nutrition] and Biodiversity and Ecosystems) (United Nations, 2002). In 2005, the Millennium Ecosystem Assessment identified key connections between biodiversity, ecosystems and human well-being (WHO, 2005), and in 2006 the Finnish presidency of the European Union presented the concept of “Health in All Policies” as a main health theme (Reference PuskaPuska, 2006). In the Finnish opinion, the core of “Health in All Policies” was to focus on health determinants mainly controlled by policies of sectors other than health. The wish was to address policies in the context of policy-making at all levels of governance. The idea in fact dates back even further: In 1978, at the WHO International Conference on Primary Health Care, the Alma-Ata Declaration emphasized the role of sectors other than health in the creation of public health: “the highest possible level of health is a most important world-wide social goal whose realization requires the action of many other social and economic sectors in addition to the health sector” (cited in Reference StåhlStåhl, 2018: 38). Health as overarching generic principle raises the question: Can One Health follow in these footsteps as an overarching governance integrator, while also being more inclusive by incorporating animal, plant and ecosystem health?
Several integrative governance perspectives regarding challenges with environmental (natural and built) determinants of health are gaining traction today, even if some of these concepts already have some history. This is driven by concern for emerging infectious diseases, rapid increases of noncommunicable diseases, rising morbidity due to ecosystem and climatic changes, and increased awareness of challenges of chemical use in human living environments and in livestock farming, including antibiotics, fertilizers and pesticides in agroecological systems and so on (WHO, 2012). One Health, EcoHealth, planetary health, global health, conservation medicine, biodiversity and health, agrihealth and health pluralism are examples of these broader frameworks, which aim for an integrated perspective on health and the living environment (Reference Assmuth, Chen and DegelingAssmuth et al., 2019).
EcoHealth encompasses ecosystem approaches to health, covering the biological, physical, social and economic environments and their relation to human health (Reference LebelLebel, 2003). The concept One Health originated at the interface of animal and human health (Reference Woods and BresalierWoods and Bresalier, 2014) with the aim of covering a larger diversity of expertise than health and veterinary sciences, and over time broadened its perspective to the environment (Reference Rüegg, McMahon and HäslerRüegg et al., 2017). Reference Zinsstag, Schelling, Waltner-Toews and TannerZinsstag et al. (2011) proposed One Health as an approach aimed at tackling complex patterns of global change, in which the inextricable interconnection of humans, pets, livestock and wildlife, along with their social and ecological environments, is evident and requires integrated approaches to human and animal health and their respective social and environmental contexts. The WHO and CBD State of Knowledge Review on biodiversity and health (2015) proposed One Health as an overarching framework for integrated efforts, while also recognizing and relating to other relevant approaches, such as EcoHealth. Earlier, a tripartite collaboration among the Food and Agriculture Organization (FAO), the World Organisation for Animal Health (OIE) and WHO (2010) proposed a similar integrated effort, also called One Health. A related concept is One Welfare, which aims to relate animal, human and environmental welfare under one umbrella (Reference BourqueBourque, 2017; also see Chapter 9). Similarly, the Lancet Commission on planetary health (Reference Whitmee, Mace and HainesWhitmee et al., 2015) highlights the integrated nature of human and planetary health.
In a different vein, there has been fresh thinking on alternative worldviews and perspectives provided by diverse knowledge systems on health and well-being for tackling sustainability challenges. The idea of holistic health traditions has existed for centuries, but recently there have been new frames of reference that allow mainstreaming of such holistic approaches. According to some health cultures, optimal health is “To be established in one’s self or own natural state” (Reference Payyappallimana, Morandi and NambiPayyappallimana, 2013: 105). To achieve this, one must have a balance of physical, mental, spiritual, social and ecological dimensions of existence. Based on this philosophy, there are distinct epistemological principles and practices for the prevention of disease and promotion of health and health care in several Indigenous and Local Knowledge cultures. Shared explanatory frameworks, healing practices including rituals, physical healing environments and so on become central in such a context. Sacredness is attributed to trees, grains, animals, hills, forests, streams, mountains and caves that are worshiped through rituals, ceremonies, festivals and fairs. Such knowledge, belief systems and worldviews find expression in agroecological traditions, art, songs and other symbolic representations and practices linked to well-being. For instance, in a study among communities of coastal Tamil Nadu, Reference SujathaSujatha (2007: 178) states, “the body is seen as being constituted by food which is the vehicle by which the external ecology is internalized.”
A shared perspective across Indigenous and local communities in the Indian subcontinent is the inherent relationship between the “outside” and “inside” worlds. In Āyurveda and other traditional knowledge systems of medicine in the subcontinent, this is known in terms of “loka” (macrocosm) and “puruṣa” (microcosm). Similar traces of this principle form an underlying basis for all Indigenous and Local Knowledge traditions. Health in Āyurveda is understood as a positive state and is based on the outcomes of adaptive feedback that each person establishes with the environment and determined by the ability of a person to adapt and self-manage (Reference Morandi, Tosto, Roberti di Sarsina and DallaMorandi et al., 2011). Similarly, in other cultures the biopsychosocial model of health (Reference EngelEngel, 1977) brings the concept of health from a purely biological realm into, as the name suggests, the psychological and social realms of health. The concept has gained popularity with health professionals, making them consider the broader factors impacting on the health and well-being of individuals and communities, indicating that health care alone does not provide health. Likewise, the concept of “salutogenesis,” coined by Aaron Reference AntonovskyAntonovsky (1979), depicts an approach that focuses on the drivers of health and well-being rather than focusing on morbidities or pathogenesis.
Though seemingly quite similar in holistic and integrative ambition, these overarching concepts do not necessarily result in identical definitions of nature and linkages with human health, nor in common framing of challenges and remedies (Reference Keune and AssmuthKeune and Assmuth, 2018). Different expert groups may identify themselves differently with the concept of One Health. On the one hand, there is a community of expertise and practice focusing mainly on nature-related health benefits, and on the other one concerned mainly with its risks (Reference Keune and AssmuthKeune and Assmuth, 2018). While the former community advocates for nature-based solutions as a path to a better future, some prominent virologists representing the latter community label nature as an extreme threat to human health. Some of the latter group even state, “nature is the biggest bioterrorist,” from which yet unknown threats should be avoided: one must “intervene in the conditions of emergence of the future, before one may be besieged by nature’s own act of emergence” (Reference MutsaersMutsaers, 2015: 128). This biosecurity framing has led to the development of vaccines, but also brought forward preventative culling of wildlife and domestic animals, resulting in a strategy with questionable ethics. Clearly, a balancing of perspectives is needed to escape such paradigmatic deadlocks. An approach coined Structural One Health (Reference Wallace, Bergmann and KockWallace et al., 2015) extended the concept of One Health to include the socioeconomic perspective more clearly. It criticized the prior iteration of One Health for failing to address the fundamental structural, political and economic causes underlying collapsing health ecologies, similar to ideas of transformative change. Figure 5.2 illustrates Structural One Health compared to other approaches, highlighting different characteristics of different health approaches and interventions.
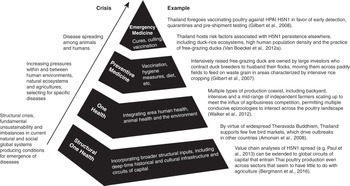
Figure 5.2 Structural One Health
“Structural One Health investigates the broader context of a disease, including out beyond the local, more proximate mechanisms of emergence on which more episodic One Health focuses. Preventive and emergency medicine are deployed in response to threats on the health of specific populations and individuals. For all mechanisms that promote disease (under ‘crisis’), the proximity in space, time and causal origin to any given outbreak increases up the pyramid. The relative importance of each point along the scale is dependent on the collective interplay between all parts of the pyramid. An array of inputs and outcomes for highly pathogenic avian influenza H5N1 in Thailand is shown across the schematic”.
5.2.3 Dilemmas in Nature-Based Approaches to Health
Reference Horwitz, Finlayson and WeinsteinHorwitz et al. (2012) and Reference Roiko, Kozak, Cleary, Murray, Tibbetts, Rothlisberg and NeilRoiko et al. (2019) summarize the complex character of nature–health linkages with reference to the paradox of the health imperative, and the opposite of the environmentalist’s paradox: Where, from an ecosystem services point of view, one would expect a clear relation between a healthy ecosystem and human health, the environmentalist’s paradox points at the fact that degradation of an ecosystem, for example by using DDT for malaria control, can in fact be beneficial in the short-term for human health. The health imperative exemplifies cases where a healthy ecosystem can, in fact, pose human health threats, for example the presence of mosquitoes in urban nature conservation areas, which may support spreading infectious diseases under specific conditions.
Reference Bauer, Kenneth and PelikanBauer et al. (2006: 156) illustrate this dilemma by comparing the focus on pathogenesis to that on salutogenesis (Figure 5.3). With pathogenesis, the focus is mainly on health risk factors for individuals in their living environment, leading to “disease, disorders, subjective sickness, malfunctioning and impairment.” With salutogenesis, the focus is mainly on human health-supporting resources, including “fitness, subjective wellbeing, optimal functioning, meaningful life and positive quality of life.” Both concepts should be considered to be complementary and interacting throughout life.
Balancing these two perspectives in relation to nature is also a clear challenge in primary health care (Reference Lauwers, Bastiaens, Remmen and KeuneLauwers et al., 2020). In the fast-growing body of scientific literature on nature–human health linkages, a role for primary health care is still only marginally present. Also, specific uptake tools for practical consideration of these linkages in primary health care seem lacking. Besides, the need for a primary One Health care approach has been highlighted (Reference Lauwers, Bastiaens, Remmen and KeuneLauwers et al., 2020).
Further scientific challenges on nature–human health linkages remain. One recent review on “types and characteristics of urban and peri-urban green spaces having an impact on human mental health and wellbeing” (Reference Beute, Andreucci and LammelBeute et al., 2020) illustrates this for an important subdomain of nature-related health benefits in the urban context (see Chapter 14). Clearly, the extensive review could not find a gold standard for a particular green space type or characteristic working best for everyone, everywhere and at every time. This heterogeneity may be explained in terms of differences in exposure duration and differences in experiences, and there are different effects for different target groups. This would lead to recommendations for a variety of green space types to capture all potential users, their different needs and their activities.
5.3 Challenges in One Health Governance
These apparent contradictions and dilemmas at the conceptual and practical level form the challenging landscape in which One Health governance should intervene. Currently, there is no clear agreement on, or understanding of, what is best practice regarding One Health knowledge (Reference Rüegg, Häsler and ZinsstagRüegg et al., 2018). A key challenge is knowledge integration (incorporating a diversity of knowledge related to different disciplines, topical areas and practices) and learning by doing. Clearly this takes time and effort: More mature initiatives become more holistic as they evolve in a trial and error process (Reference Buttigieg, Savic and CauchiButtigieg et al., 2018; Reference Fonseca, Torgal and de MeneghiFonseca et al., 2018; Reference Hanin, Queenan, Savic, Rüegg and HäslerHanin et al., 2018; Reference Paternoster, Tomassone and TambaPaternoster et al., 2017). In addition, the importance of knowledge integration and particularly the sharing of data is well-recognized but is often hampered by political boundaries. A phenomenon that has been reported for the governance of the Sustainable Development Goals (SDGs) (Reference Nilsson, Chisholm and GriggsNilsson et al., 2018) can also be observed in One Health (Reference Hanin, Queenan, Savic, Rüegg and HäslerHanin et al., 2018). The evaluation of an international effort for infectious disease surveillance showed that national as well as institutional borders are challenging for the sharing of data (Reference Hanin, Queenan, Savic, Rüegg and HäslerHanin et al., 2018). Whether this has structurally changed during the COVID-19 pandemic remains to be seen.
Another important One Health challenge is interdisciplinary and transdisciplinary approaches, which appear to be one of the most demanding practices in the academic context (Reference Léger, Stärk, Rushton and NielsenLéger et al., 2018; Reference Muñoz-Prieto, Nielsen and Martinez-SubielaMuñoz-Prieto et al., 2018). There seems to be a disconnect between the ambition to work across disciplines and the cultural practice in science of evaluating achievements based on scientific, preferably high-impact, publications. The prevailing competitive mentality in academia is a serious obstacle to the trusted collaboration required for interdisciplinary progress. An explicit mandate to reach beyond academia and connect to practitioners can result in a surprisingly good alignment with the One Health concept (Reference Radeski, O’Shea, De Meneghi and IlieskiRadeski et al., 2018). Partnerships spanning collaborators from government, academia and practitioner circles may generate more holistic solutions.
5.3.1 The Scission between Human Health Benefits and Threats from Nature
As already mentioned above, although One Health acts as an integrating umbrella for talking about health, there appear to be two main opposing narratives around nature–human health linkages, under the same heading of “One Health” (Reference Keune, Kretsch and De BlustKeune et al., 2013). But even without explanatory causal links, a comprehensive conversation about the management of our environment requires a constructive dialogue between those two communities. To move from a struggle for prerogative of interpretation to a co-construction of understanding, it will be necessary to have more direct interaction and discourse between the different viewpoints and groups, through transdisciplinary governance.
5.3.2 Which Ethics?
As emphasized by Reference Morand and LajaunieMorand and Lajaunie (2019) and Reference Lainé and MorandLainé and Morand (2020), ethical reflection in the field of health and biodiversity would require examining the relevant scientific domains (i.e. biology, ecology, evolution, human medicine, animal medicine, political science, environmental studies, anthropology and law), their epistemology and, for some, deep roots in the colonial sciences based on a paternalistic perspective, dominated by the lens of the Western worldview on reality. Consequently, several ethical responses to public health crises have been proposed with “One Bioethics,” “One Health ethics,” “Global Health ethics” and, more recently, “Planetary Health ethics,” with no consensus among bioethicists. The need to recognize scientific pluralism appears essential for interdisciplinarity, but it requires acknowledging the values and practices of each scientific domain. It requires also a decolonized (less Western paternalistic) and a more-than-human (respecting also nonhuman health) One Health approach (Reference Lainé and MorandLainé and Morand, 2020). Further, it needs to be stressed that even though perspectives like One Health are more encompassing, they are to be implemented in a context of highly linear positivist science and a practice structure of current health systems that have limited capacities related to human resources, knowledge and so forth.
While “Global Health ethics” is essential in underlining the importance of justice and equity, a “One Health ethics” or a “Planetary Health ethics” could refer more to a metaethics regarding the ecological crisis and its implications for the study of nature or biodiversity. The question is, then: Is nature reducible to a simple mechanism such as the dilution effect, or is it a complex adaptive system of physical and sensible interactions between various life forms including humans? Considering what kind of nature is at play in a health crisis has profound consequences for the attitudes toward nature and people and for health policy responses. COVID-19, as well as previous pandemics, shows that crises are often systemic, which calls for the development of systemic actions with better nature stewardship, and resonates well with the ideas of transformative change.
5.3.3 Balancing Top-Down and Bottom-Up Health Norms and Challenges
Contemporary medical practice relies heavily on norms and reference values. A strong deviation from a mean is commonly considered as pathology, implying that regularity (i.e. the mean) is a healthy objective. Consequently, decision matrixes are often positivist, objective and deterministic, with the aim of reestablishing normalcy. Similarly, in public health, veterinary health and food safety, solutions are often prescribed top-down, implying singular linear pathways in isolated aspects of health. There are obvious advantages of this approach when it comes to health management at scale, such as decision-making for resource allocation in a national health service. However, current health management is in stark contrast to the observation that complex systems show fractal behavior, in a coherent variation and diversity (Reference WestWest, 2012). A complex adaptive systems approach in medicine would require moving away from preestablished medical problems with expected solutions, and working with people toward defining the medical goal itself. Such an approach requires, of course, an acceptance of unpredictability, uncertainty and ambiguity (Reference Strand, Rortveit and ScheiStrand et al., 2004) – something most health care systems are not set up to deal with. At the onset of the COVID-19 pandemic, many aspects were unknown. Nevertheless, in order to prevent its spread, swift action was needed. It proved more successful to take some generic assumptions to contain highly infectious diseases and to implement a crude strategy in Mongolia and Taiwan, for example, than to delay action waiting for sufficient detailed knowledge. The ambiguity of the evidence and the unclear relation to the situation in the field kept fueling public debates about the way to deal with the pandemic in many other democratic states, while lives were lost to the disease.
There is no doubt that norms and reference values have an important place in daily practice, but there is a risk that such norms may obliterate other potential pathways to health. In the context of One Health, the question arises: To what degree are such norms universal and time independent, and to what degree would they require contextualization? While a strong focus on individual choice in health care has the advantage of more tailor-made health strategies, the right to individualism stands in contrast with the needs of communities or societies. Especially in developed countries, when people make unhealthy choices, the health costs either result in a loss of solidarity because the community does not want to cover the consequences of individual behavior, or in rising health expenses for the community. Another example is the individual choice of vaccination, where people who may choose to abstain from vaccination contribute to lowering community or herd immunity and thereby increase disease risks. Here again, cohesion appears to be an important concept, that is, solidarity needs to be reciprocal: While individuals consider the resilience of the community in their acts, the community can offer solidarity in return. Importantly, at various levels of socioeconomic status, health should be discussed and co-produced. This shows that One Health is more than an integrated approach to emerging infectious diseases, but a way to address many health concerns, from malnutrition to traffic accidents, in an integrative and inclusive governance process. The impacts are considerable as they affect legislation and require, and represent, transformative change. Some possible approaches have been proposed such as social prescription (Reference Jani and GrayJani and Gray, 2019; Reference Jani, Pitini, Jungmann, Adamo, Conibear and MistryJani et al., 2019), positive health dialogue (Reference Huber, van Vliet and GiezenbergHuber et al., 2016), quintuple helix innovation (Reference Carayannis, Barth and CampbellCarayannis et al., 2012), critical complexity (Reference CilliersCilliers, 2005; Reference KeuneKeune, 2012), participatory action research (Reference Kincheloe, Kapoor and JordanKincheloe, 2009) and salutogenesis (Reference Lindström and ErikssonLindström and Eriksson, 2005; Reference Lindström and Eriksson2006).
5.3.4 What Are the Values Associated with Health?
In the search for generic validity of concepts and frameworks, it goes unnoticed that we know very little about the lives of those who experience the complex entanglements between humans, animals and ecosystems on a daily basis, and whose stewardship is decisive for change to occur. Although there are studies on more general values (World Values Survey Association, n.d.) – particularly the comparative value of health for oneself – people, animals and ecosystems have not been explored. While currently, with few exceptions, justice is an anthropocentric notion, the aim of achieving interspecies health equity as an outcome of One Health suggests that there may be a need to develop a framework for biocentric social justice (see Chapters 8 and 9).
5.3.5 The Need for a Scalable Definition of Health
Such a framework would need to be grounded in a generic understanding of health. Exchange across different disciplines and sectors in charge of different scales of life, from microorganisms to national and global economies, reveals a large variety of definitions of health. At the level of ecosystems, the concept of health is controversial (Reference RapportRapport, 1998). But also at an individual level, our concepts of personal health are diverse. Health can be regarded as a dynamic, adaptive process rather than a static state. A potential framing would be health as resilience at the individual level, with well-being and welfare as emerging properties of a functional co-adaptation between an individual and their direct environment. In some Indigenous cultures, an individual is also seen as a constantly changing substratum and thus health as interaction between two dynamic (in some contexts deteriorating) systems. The concept of resilience can be evaluated at multiple levels of social-ecological systems. Metrics for resilience are different at different scales, primarily because change occurs at much slower rates at larger scales and is faster at smaller scales, thus preventing the same relative time resolution at all scales. Nonetheless, the principal idea can be transferred across all scales and can also accommodate for cultural differences. Consequently, One Health approaches would need to foster resilience at all scales, and as a minimal requirement not reduce resilience at any scale in a social-ecological system. This would allow humans and nonhumans to live together and allow adaption to various challenges in the short and long term.
5.3.6 Will Egoism Define the Boundaries?
Inclusive governance – as used in the field of sustainable development – may help to make use of One Health opportunities and to promote dialogue and solutions for intergenerational health if there is propensity among participants to engage, connect, reflect and change. It is expected that economic activities that promote human well-being, sustainability and justice will need to be coupled with a steady-state or degrowth economy respecting planetary boundaries. This is essentially the premise of ecological economics. The future will show whether people are willing to rethink today’s concept of prosperity driven by continuous increase in economic growth. Data show that the link between income and life-satisfaction is only linear up to a certain point (Reference Clark, Flèche, Layard, Powdthavee and WardClark et al., 2018). Given that the paradigm from which a system arises has a high leverage on the system outcomes, it appears intuitive that there are important drivers of well-being, health and disease rooted in our current shared values (Reference MeadowsMeadows, 2008). It may be time for health professionals to engage in a broader conversation about transformative change.
5.4 Methodological Gaps
So far, many participatory methods rely on workshops and group facilitation. In order to operationalize participation at a larger scale, scalable tools must be developed. While these are available for example for smart cities, in the field of One Health this has not been developed. Furthermore, the call for transdisciplinarity would require multiple perspectives and the facilitation of interactions across many social boundaries.
While the skill set usually associated with public health, veterinary health or conservation relies strongly on natural science, it appears much more important to be equipped with skills unusual in these fields, such as nonviolent communication, philosophy of science, history of science, macroeconomics, systems thinking, designing thinking, dealing with scales, and (nonequilibrium) social sciences. Also, the importance of self-reflection can be stressed: dealing with ambiguity and uncertainty, and critiquing our own and others’ paradigms.
While we have discussed the concerns about the prescriptive nature of legislation previously, market mechanisms (see Chapter 6) are also failing to provide public health, animal health and welfare, and environmental protection, as the latter are not restricted to tangible entities and not tradable. Impaired health and reduced resilience at all scales is often a result of cumulative behavior. The current socio-ecological context does not seem to provide the appropriate feedback and incentives for sustainable behavior. In the light of modern neuroscience and nonequilibrium social sciences, it appears to be an achievable target to reflect on the processes and features needed in a social-ecological system for all life to thrive. Solutions may be found in ecological economics, where concepts of degrowth, green growth and similar are discussed to provide alternatives to the prevailing increasing economic growth theory. Reference DalyDaly (2003) observed that beyond a certain point, growth is uneconomic and that multiple forms of ill health and the costs thereof can increase faster than wealth. Consequently, novel conceptualizations of growth and their measurement tools provide an opportunity for different narratives, research and strategies, and relate well with, and are an integral part of, ideas of transformative change and governance.
5.5 Early One Health Lessons from COVID-19
The COVID-19 pandemic, a singular disruptive event in recent human history, has required rapid, innovative, coordinated and collaborative approaches to manage and ameliorate its worst impacts. However, the threat remains, and learning from initial efforts may benefit the response management in the future. One Health approaches to managing health challenges through multistakeholder engagement need an enabling environment, for example in terms of available budgets or the instigation of integrative and inclusive processes. Reference Häsler, Bazeyo and ByrneHäsler et al. (2020) described three case studies from state (New South Wales, Australia), national (Ireland) and international (sub-Saharan Africa) scales that illustrate different aspects of One Health in action in response to the COVID-19 pandemic. In Ireland, a One Health team was assembled to help design complex mathematical and resource models. In New South Wales, state authorities engaged collaboratively with veterinarians and epidemiologists to leverage disease outbreak knowledge, expertise and technical and support structures for application to the COVID-19 emergency. The African One Health University Network linked members from health institutions and universities from eight countries to provide a virtual platform for knowledge exchange on COVID-19 to support the response. Themes common to successful experiences included a shared resource base, interdisciplinary engagement, communication network strategies and a global perspective for addressing local needs.
The authors concluded that the COVID-19 pandemic showed the need for improvement of emerging infectious disease (EID) preparedness, early warning and prevention. The cost of unpreparedness is high, leading to high mortality rates and draconic measures like lockdowns. Early warning systems in support of more targeted and rapid responses need to be strengthened. Better/broader understanding of the consequences of human–environment interactions is also needed. Several key drivers for EID clearly came to the foreground: 1. Human population density, with degrading natural ecosystems associated with increased disease transmission risk. 2. Global travel and trade. 3. Excessive consumption: resulting in the aforementioned environmental degradation, which is a defining factor for facilitating pandemics and exacerbating the effects. Barriers for overcoming these challenges are largely structural in character, both institutional (governance) and socioeconomic (see Chapter 4).
Next to direct COVID-19 / One Health related challenges, some generic challenges are relevant to One Health operationalization. The need for better interdisciplinary and transdisciplinary collaborative arrangements is one of the core ambitions of One Health. Structural barriers for collaboration remain, including a lack of mutual understanding regarding the expertise of others, meaning that work continues in silos within rigid structures. Also, attitudinal barriers remain, such as lack of openness toward collaboration. “Old” governance challenges appear even more prominent: well-coordinated multilevel, integrative governance at local, regional, national and global levels remains a crisis management challenge. Current governance structures clearly showed deficiencies in adequate crisis management, including a general lack of preparedness and lack of coordination. A better balance between relevant governance issues is needed, including social issues.
Enhanced scientific capacity is needed; there is currently insufficient long-lasting research capacity in all sectors: animal health, human health, plant health and ecosystem health. This warrants increased mutual understanding and overcoming silos: There is lack of sufficient knowledge of the expertise of the others. We need open science: sharing instead of competing on crucial knowledge. The connection between science and policy is problematic: The science-policy interface was already struggling at the beginning of the COVID-19 crisis, when early warnings from scientists were not taken seriously.
Systemic health challenges, like COVID-19, need a systemic approach, such as Structural One Health. This requires an integrative perspective, overcoming barriers between disciplines, sectors and topical foci. This also requires a One Health funding framework, in order to provide sufficient resources. The COVID-19 crisis clearly revealed some systemic weaknesses, and may offer momentum for change. Finally, we notice the positive role and importance of nature for health during the COVID-19 pandemic and resulting confinement measures. The lockdown policies adopted in several countries, encouraging outdoor physical activity, highlighted the role of nature recreation facilities in the urban context for human health, and the challenge of accessibility for many urban households. In situations where visits to natural surroundings were still possible, an increase in visits was observed, as shown, for example, by a public survey during the first COVID-19 wave in Belgium (Reference Lenaerts, Heyman and De DeckerLenaerts et al., 2021). People also reported a positive effect on human health and well-being. In situations where such visits were restricted, people looked forward to using parks and other natural areas, resulting in an increase in visits when allowed under lockdown restrictions. This highlights the need to account for social differences in options for contact with nature. The least deprived often live in single family dwellings with gardens and thus enjoy natural surroundings, even when confined to their homes. In preparation for future pandemics, policies should plan for socially equal access to natural surroundings (Reference Slater, Christiana and GustatSlater et al., 2020), including for human health care workers, who during a pandemic have to perform their tasks under severe pressure. In return, the increased visiting intensity of natural spaces in high density areas also poses a threat to those very spaces, and the related health benefits, and requires attention in a sustainable governance context.
5.6 Conclusions
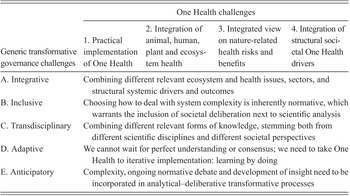
We see many opportunities for applying One Health to transformative biodiversity governance. The transformative governance ambitions (see Chapter 1) resonate quite well with the One Health ambitions and challenges presented in this chapter. A synthesis is presented in Table 5.1.
We discuss the specific elements of the table and how they are linked in further detail. The specific One Health aspects concern the following challenges: (1) Practical implementation of One Health. This still is considered a challenge, especially when taking into account the other aspects (expectations, demands) mentioned below. Initially, (2) Integration of animal, human, plant and ecosystem health was mainly considered as the core aim of One Health. As described in the chapter, there are still challenges in that respect. This very much relates to (3) An integrated view on nature-related health risks and benefits: traditionally One Health was mainly focused on health risks, taking potential health benefits of nature contact far less into account. Finally, (4) Integration of structural societal One Health drivers, or Structural One Health, which can be seen as a more critical, fundamental and preventative turn in the One Health debate, taking it beyond the development of vaccines and culling of “dangerous” animals.
One Health, like transformative change, deals with systemic challenges. Taking into account and structuring complexity and decision-making, and dealing with inherent uncertainties, unknowns and ambiguities, is therefore at the core. The process of how to deal with complexity, also from the scientific perspective, can be perceived as a social and normative process in itself. Complexity can never be fully grasped and should encourage us to choose what has to be taken into account for understanding and action. These choices have an important framing effect and are normative in nature, requiring a combined scientific and deliberative effort (Reference CilliersCilliers, 2005; Reference KeuneKeune, 2012). In order not to stand still, we need to act wisely and deliberatively, in an adaptive learning-by-doing approach.
Collaboration is key to One Health to overcome silos. The implementation of One Health can benefit from transdisciplinary and iterative processes between policy, science and practice, and will enhance practical relevance of these collaborations (Reference Hitziger, Aragrande and BerezowskiHitziger et al., 2019). This also requires a collaborative attitude (soft skills) and a sharing attitude (open data, data sharing, integrated data base management).
In support of the above-mentioned One Health challenges, several elements of an enabling environment are to be considered. An important element is a dedicated network for professionals, practitioners and stakeholders. When the ambition of integration leads to the creation of large One Health institutions, this runs the risk of building fences rather than creating openness to (new) collaborations. This may be overcome by focusing on open, collaborative networks like Communities of Practice, which are less (institutionally) bound and more flexible, and are open to newcomers and new ideas and approaches (Reference Keune, Flandroy and ThysKeune et al., 2017). Such networks should not be limited to scientific experts, but also need to include policy experts, local knowledge holders, practitioners, grassroots organizations and all relevant stakeholders. The Network for EcoHealth and One Health (NEOH), the European chapter of EcoHealth International, is a good example, and so are other similar nature–health initiatives (Reference Keune, Friesenbichler, Häsler, Marselle, Stadler and KornKeune et al., 2019).
One Health approaches aim to overcome ad hoc reactive actions responding to emerging health challenges. It is better to develop proactive anticipatory governance capacity and preparedness, to allow us to better foresee health risks. The introduction of One Health concepts in primary, secondary and tertiary education, with the aim to raise awareness and create a natural understanding of systems and their interlinked nature, is important. Finally, the availability of sufficient financial and other resources for One Health science, policy and practice remains another crucial challenge. Current investment practices then have to put less focus on a purely economic rationale, and focus more on other rationales for society at large. A One Health funding framework could be supportive in allocation of funding, both in science, policy and practice.