Identification of comorbid post-traumatic stress disorder (PTSD) in patients with other serious mental illness is of substantial importance given that this is associated with poorer clinical outcomes of these disorders,Reference Campbell, Felker, Liu, Yano, Kirchner and Chan1–Reference Seow, Ong, Mahesh, Sagayadevan, Shafie and Chong4 and that PTSD is a treatable disorder.5 Some studies suggest that a large proportion of patients in secondary-care mental health services with other (non-PTSD) primary diagnoses meet criteria for PTSD on screening, and that there is usually no record of PTSD in the patient's clinical records.Reference Kilcommons and Morrison6–Reference Wang and Vivek9 If these estimates of undetected PTSD are accurate this raises a serious concern that PTSD is not adequately identified through routine clinical care pathways. Other studies, however, report much lower frequencies of undetected PTSD.Reference Brady10–Reference Tagay, Herpertz, Langkafel and Senf12 Reasons for variation in estimates of PTSD across studies could include differences in the characteristics of the people in the study (such as gender, primary diagnosis) or of the study methodology (such as measurement or selection bias). An accurate estimate of the frequency of undetected PTSD in secondary care, and an understanding of factors associated with variation in frequency is required to determine if, and how, services should respond. In this study, we systematically review the literature to determine whether undetected PTSD is present at a prevalence that would reflect substantial clinical importance within secondary-care mental health services. For the purpose of this study we define ‘substantial clinical importance’ as presence of undetected PTSD in 10% or more of patients in secondary care, an arbitrary value but one that we believe most service providers would agree merits clinical concern. Furthermore, we also aim to determine the extent to which variation in reported estimates might be because of sample characteristics or methodological biases. To our knowledge there have not been any previous systematic reviews addressing these aims.
Method
Our protocol (online supplement DS1 available at https://doi.org/10.1192/bjp.2017.8; not pre-registered) followed Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelinesReference Stroup, Berlin, Morton, Olkin, Williamson and Rennie13 and a PRISMA checklist was completed (online supplement DS2).
Literature search
We (S.D.) searched the following databases from 1980 to 22 August 2016: Embase, Medline, PILOTS and PsycINFO using relevant keywords and subject headings (online supplement DS3). We (H.C., H.M., A.P. and S.Z.) hand searched reference lists of included studies to identify further relevant papers. We restricted the search to published, peer-reviewed studies, but not by study design. Only English-language studies were included.
Selection criteria
Our inclusion criteria were: (a) participants in secondary care (i.e. specialist mental health services) with a mental illness diagnosis according to DSM or ICD criteria; (b) screened for PTSD using a measure based on DSM or ICD criteria; (c) used medical records to obtain participants’ clinical diagnoses of PTSD; (d) reported proportion of sample with PTSD on screening, and with PTSD in medical records; and (e) reported data for individuals aged 16 and over. Studies where samples were selected on the basis of (a) having a diagnosis of PTSD, (b) having a trauma history, or (c) being referred to a trauma service were excluded.
Study selection and data extraction
We examined all titles and abstracts (S.Z., H.C. and A.P.) and obtained full texts of potentially relevant papers. Working independently and in duplicate, we (S.Z., C.L., H.R., H.C., A.P. and H.M.) read the papers to determine if they met inclusion criteria using eligibility record forms (online supplement DS4). We resolved disagreements by consensus, and extracted data independently and in duplicate.
Quality assessment
The likely internal validity for each study was assessed (S.Z., C.L. and H.R.) based on key selected components of a risk of bias tool for prevalence studies,Reference Hoy, Brooks, Woolf, Blyth, March and Bain14 adapted for this review. We focused particularly on sampling strategy, response rates, and masking of screening assessment and clinical records review as the likeliest sources of bias in estimating frequency of undetected PTSD. For examination of heterogeneity, studies were also categorised into low, medium, and high risk of selection bias (online Table DS1).
Data synthesis
The proportion of PTSD that was detected (recorded) in clinical notes was estimated as: n with PTSD on record/n with PTSD on screening. The proportion with undetected PTSD was estimated as: (n with PTSD on screening – n with PTSD on record)/sample n. We grouped studies together and pooled data in a meta-analysis, although such summary estimates are only useful where studies are adequately homogenous. Studies were pooled using a random-effects model (using metaprop in Stata version 14). Presence of publication bias was investigated by viewing funnel plots and using Egger's test.Reference Egger, Davey Smith, Schneider and Minder15 We assessed heterogeneity using the I Reference Holtzheimer, Russo, Zatzick, Bundy and Roy-Byrne2 statistic.Reference Higgins and Thompson16
We investigated sources of heterogeneity by meta-regression using the metareg command. We hypothesised that frequency of PTSD on screening might be higher for veterans (because of potentially greater exposure to traumas, and increased recognition by clinicians), patients diagnosed with a psychotic disorder (as the hierarchical approach to diagnosis and the phenotypic overlap between re-living experiences and hallucinations could lead to reduced identification of PTSD compared with other diagnoses), in-patients (as potentially indexing more severe illness), studies using self-report PTSD questionnaires (as lower specificity than interviews) and in studies with a greater likelihood of selection bias, and that frequency might vary by country of study (because of different rates of PTSD in different populations). We also examined, as secondary hypotheses, variation in relation to age (as greater cumulative exposure to trauma with age), gender (as PTSD is more common in women) and year of publication (as services studied in recent publications might be more aware of comorbid PTSD).
We also examined pooled estimates for specific diagnostic categories: (a) psychotic disorders, (b) affective disorders (depressive disorders and bipolar disorder), (c) substance use disorders, (d) anxiety and adjustment disorders, (e) eating disorders, and (f) personality disorders. As relatively few studies included only participants with one primary diagnosis or presented results separately for diagnostic groups, we also repeated these analyses including studies where >50% of the sample had the same diagnosis.
Results
Search results
The literature search yielded 7581 references. After reading titles and abstracts, the full articles of 223 papers were assessed for eligibility, and 194 of these were excluded (PRISMA flow diagram, Fig. 1).
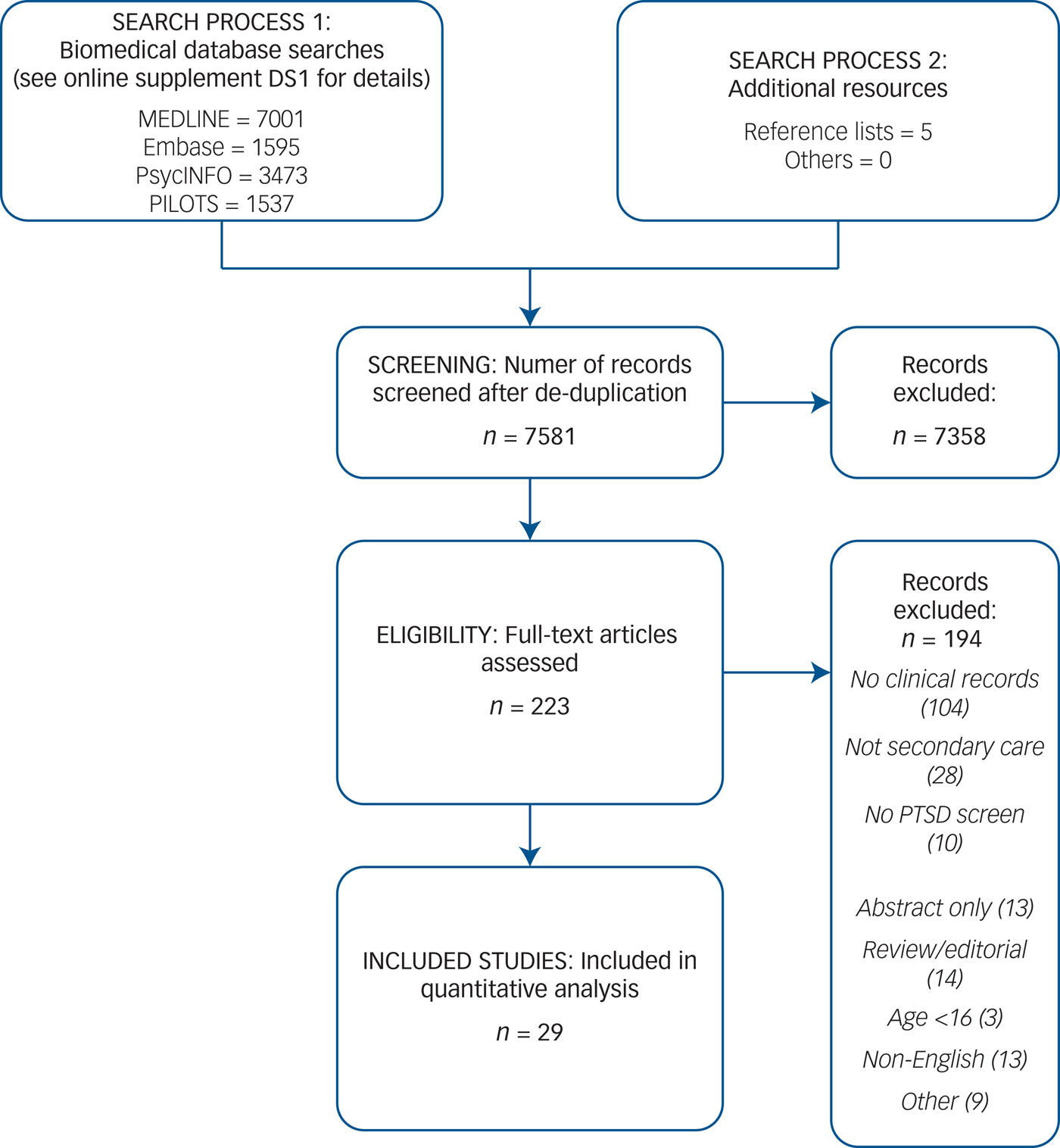
Fig. 1. PRISMA flow diagram.
Included studies
We included 29 studies (6412 individuals) that had data to allow us to estimate the extent of undetected PTSD in a secondary-care mental health setting (online Table DS2). Of these, 15 were based in the USA,Reference Kimerling, Trafton and Nguyen7–Reference Davidson and Smith11, Reference Bonn-Miller, Bucossi and Trafton17–Reference Villano, Rosenblum, Magura, Fong, Cleland and Betzler26 3 in each of Australia,Reference Howgego, Owen, Meldrum, Yellowlees, Dark and Parslow27–Reference McFarlane, Schrader, Bookless and Browne29 the UKReference Kilcommons and Morrison6, Reference Reynolds, Mezey, Chapman, Wheeler, Drummond and Baldacchino30, Reference Reynolds, Hinchliffe, Asamoah and Kouimtsidis31 and the Netherlands,Reference de Bont, van den Berg, van der Vleugel, de Roos, de Jongh and van der Gaag32–Reference Lommen and Restifo34 2 in Germany,Reference Tagay, Herpertz, Langkafel and Senf12, Reference Tagay, Schlegl and Senf35 and 1 each in South Africa,Reference Van Zyl, Oosthuizen and Seedat36 SpainReference Alvarez, Roura, Foguet, Oses, Sola and Arrufat37 and Turkey.Reference Kavakci, Semiz, Kartal, Dikici and Kugu38 Three studies were in military veteran populationsReference Kimerling, Trafton and Nguyen7, Reference Bonn-Miller, Bucossi and Trafton17, Reference Calhoun, Stechuchak, Strauss, Bosworth, Marx and Butterfield18 and 26 were in non-veterans, 1 within an incarcerated population.Reference Gosein Varendra, Stiffler Jon, Frascoia and Ford Elizabeth23 Most studies (n = 16) included individuals with a variety of mental health disorders, whereas the rest ascertained individuals with specific disorders (six with substance use disorders,Reference Kimerling, Trafton and Nguyen7, Reference Bonn-Miller, Bucossi and Trafton17, Reference Dansky, Roitzsch, Brady and Saladin22, Reference Reynolds, Mezey, Chapman, Wheeler, Drummond and Baldacchino30, Reference Reynolds, Hinchliffe, Asamoah and Kouimtsidis31, Reference Gielen, Havermans, Tekelenburg and Jansen33 four with psychotic disorders,Reference Kilcommons and Morrison6, Reference Calhoun, Stechuchak, Strauss, Bosworth, Marx and Butterfield18, Reference de Bont, van den Berg, van der Vleugel, de Roos, de Jongh and van der Gaag32, Reference Lommen and Restifo34 two with mood or anxiety disordersReference Komiti Angela, Jackson Henry, Judd Fiona, Cockram, Kyrios and Yeatman28, Reference Van Zyl, Oosthuizen and Seedat36 and one with eating disordersReference Tagay, Schlegl and Senf35). The mean age of participants (28 studies) was 38.8 years (range 26.5 to 51.9 years).
Prevalence of PTSD
The median prevalence of PTSD on screening was 33.3% (interquartile range (IQR) 23.4–40.0%), with evidence of substantial heterogeneity across studies (pooled mean 31%, 95% CI 26–36%, I Reference Holtzheimer, Russo, Zatzick, Bundy and Roy-Byrne2 = 93.1%) (online Fig. DS1). When we examined the prevalence of PTSD on screening within specific disorder categories the heterogeneity was substantially lower for studies with a primary diagnosis of a substance use disorder, but not for other diagnostic groups (online Fig. DS2). The mean prevalence of PTSD on screening in samples of participants with a substance use disorder was 36% (95% CI 33–40%, study n = 6, 793 individuals, I 2 = 0%), with a psychotic disorder was 31% (95% CI 21–41%, study n = 6, 2994 individuals, I 2 = 89.1%), with an affective disorder was 39% (95% CI 19–62%, study n = 3, 155 individuals, I 2 = 87.4%) and with a mixture of disorders was 30% (95% CI 22–39%, study n = 16, 2303 individuals, I 2 = 94.5%).
The median prevalence of PTSD diagnoses in clinical records was 2.3% (IQR 1.1–4.5%), with evidence of substantial heterogeneity (mean 3%, 95% CI 2–4%, I 2 = 85.3%). Of those with PTSD on screening, median level of detection (i.e. recorded in notes) was 11.5% (IQR 2.8–19.4%), with substantial heterogeneity across studies (mean 10%, 95% CI 6–16%, I 2 = 86.6%).
Undetected PTSD
The median proportion of participants within each study that had undetected PTSD was 28.6% (IQR 18.2–38.6%), with evidence of substantial heterogeneity across studies (mean 27%, 95% CI 22–32%, I 2 = 93.3%) (Fig. 2). There was no evidence of publication bias arising from an absence of small studies with lower proportions of undetected PTSD (Egger test (29 studies), P = 0.743).
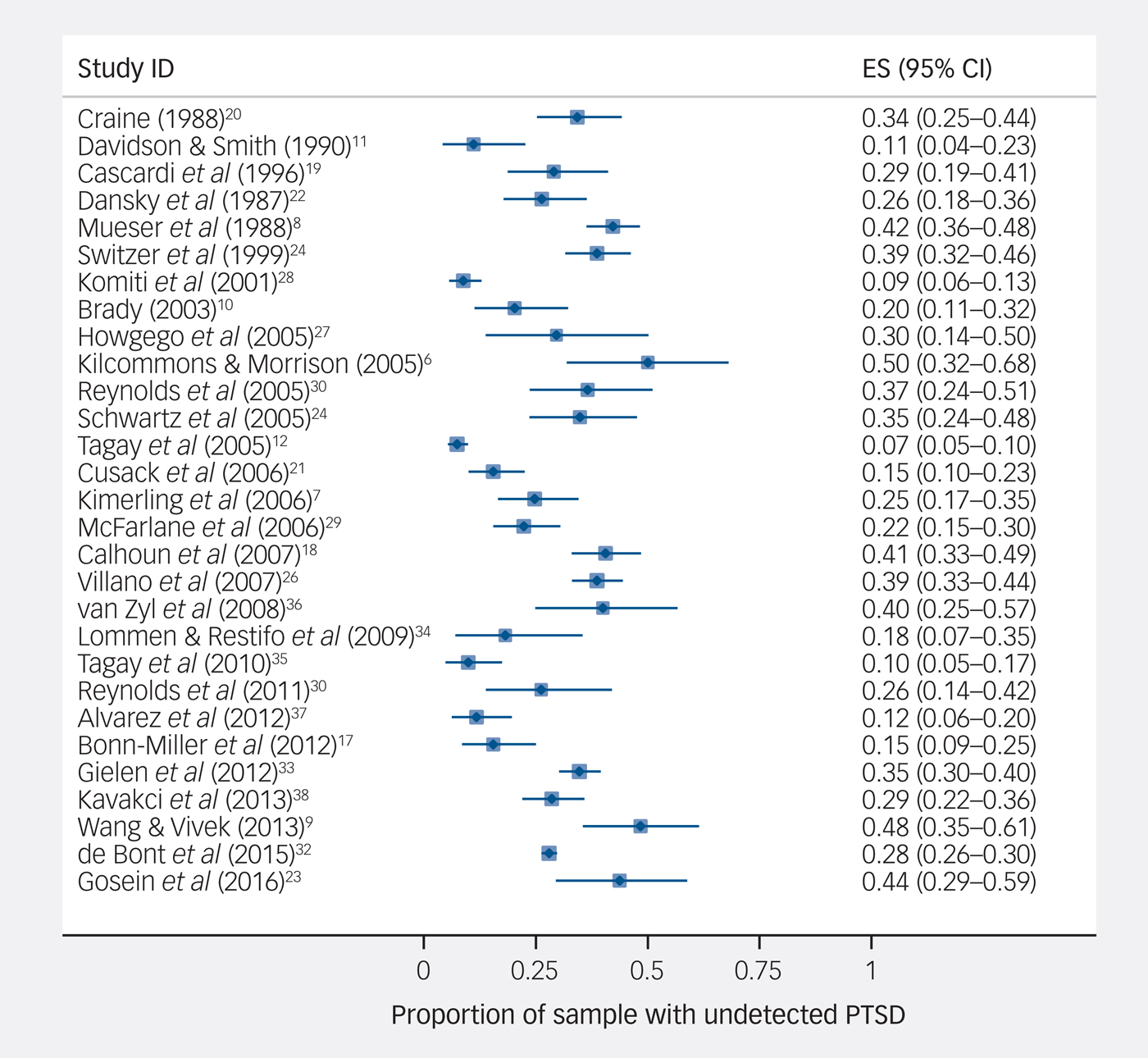
Fig. 2 Prevalence of undetected post-traumatic stress disorder (PTSD).
The mean prevalence of undetected PTSD in participants with psychotic disorders was 28% (95% CI 19–37%, study n = 6, 2994 individuals, I 2 = 86.3%), with substance use disorders was 27% (95% CI 21–34%, study n = 6, 793 individuals, I 2 = 71.1%), with affective disorders was 34% (95% CI 14–57%, study n = 3, 155 individuals, I 2 = 88.5%), and for samples with a mixture of disorders was 27% (95% CI 19–35%, study n = 16, 2303 individuals, I 2 = 94.4%) (Fig. 3).
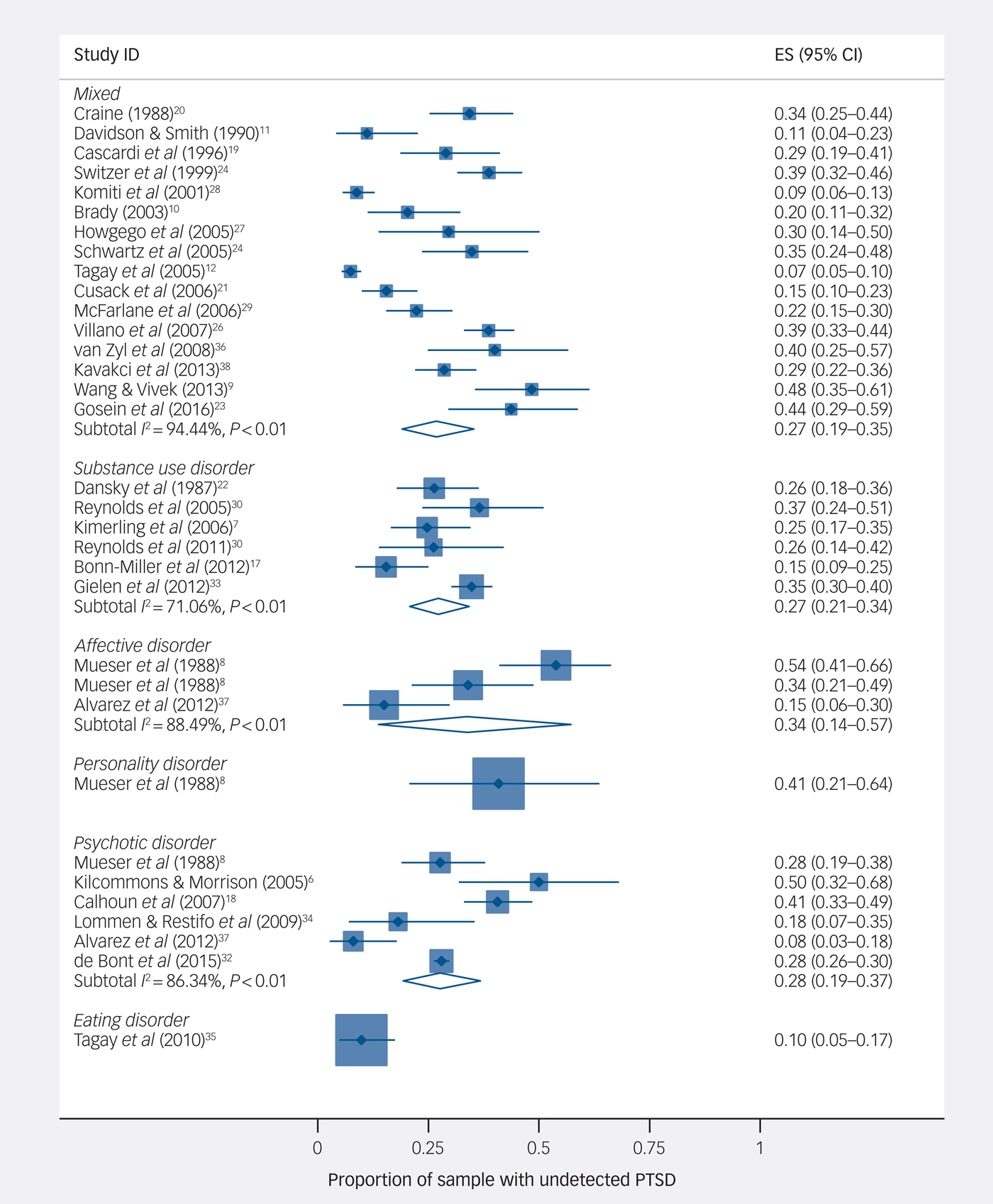
Fig. 3 Proportion of sample with undetected post-traumatic stress disorder (PTSD), by diagnostic subgroup.
Results were similar when we included studies where more than half of participants had the same diagnosis (online Fig. DS3). In a stratified analysis there was no evidence that undetected PTSD was less common when restricting studies to those using a structured interview for screening for PTSD (median proportion 26.3%, IQR = 20.3–38.6%) compared with those using a self-report questionnaire (median proportion 28.8%, IQR = 15.5–40.6%).
Exploring heterogeneity
Given the strong evidence of heterogeneity, the overall estimates of undetected PTSD are not particularly informative, and we therefore explored potential sources of heterogeneity (Table 1 and online Table DS3).
Table 1 Meta-regression of primary variables explaining variation in frequency of undetected post-traumatic stress disorder (PTSD)

a. Bias risk (low) – coded as non-low (0), medium (1), low (2); country – coded as USA (1) v. rest (0); in-patients – coded as out-patients only (0), mixed (1), in-patients only (2); psychosis – per 10% increase in sample with a psychotic disorder; PTSD tool – coded as interview (0) v. questionnaire (1); veterans – coded as veterans (1) v. non-veterans (0).
b. Adjusted for other variables in the table (residual I 2 = 5.6%)
PTSD on screening
Meta-regression showed strong evidence that levels of PTSD on screening varied across country of origin (P = 0.005, residual I 2 = 19.6%), with estimates being higher in studies from the USA (USA v. rest: difference 13%, 95% CI 4–22%, P = 0.007). There was very weak evidence that PTSD on screening was higher in studies with higher proportions of older participants (P = 0.078) and men (P = 0.071), but little evidence that other variables explained heterogeneity.
Clinical detection of PTSD
There was some evidence that PTSD, if present on screening, was less likely to have been detected in samples with a higher proportion of patients with a psychotic disorder (P = 0.024), and more likely to have been detected in samples of veterans (P = 0.053) and studies that used interviews to screen for PTSD (P = 0.068). There was little evidence that variation in detection of PTSD was associated with the other variables examined.
Undetected PTSD
There was some evidence from meta-regression that levels of undetected PTSD were higher in studies from the USA (P = 0.050) and in studies on in-patients (P = 0.072), but little evidence that levels were higher in studies with proportions of patients with a psychotic disorder (P = 0.156). However, in a multivariable model including the primary explanatory variables, there was strong evidence that undetected PTSD was higher in studies from the USA (P = 0.001) and in samples with greater proportions of patients with a psychotic disorder (P = 0.006).
Quality assessment
A total of 14 of the 29 studies described either random sampling or sampling of consecutive admissions or patient contacts (online Table DS3). Of these 14 studies, 9 reported response rates, 5 of which included data from 75% or more of eligible patients.
Masking of researchers to PTSD histories in clinical records was reported for 3 of the 16 studiesReference Switzer, Dew, Thompson, Goycoolea, Derricott and Mullins25 that relied on research interviewers to determine the presence of PTSD on screening, whereas 13 studies used self-report screening measures. Masking of researchers to PTSD screening results when searching the clinical records for PTSD diagnoses was reported for 2 of the 29 studies,Reference Brady10, Reference Switzer, Dew, Thompson, Goycoolea, Derricott and Mullins25 and 1 study excluded participants with PTSD in their clinical records at study entry.Reference Van Zyl, Oosthuizen and Seedat36
Estimates of PTSD on screening were lower for studies with the lowest risk of bias in a stratified analysis, although confidence intervals overlapped substantially (lowest risk 24%, 95% CI 12–40%; intermediate risk 31%, 95% CI 22–41%; highest risk 35%, 95% CI 28–42%). A similar pattern was observed for estimates of undetected PTSD (lowest risk 21%, 95% CI 9–36%; intermediate risk 29%, 95% CI 19–39%; highest risk 28%, 95% CI 22–33%).
Discussion
In this systematic review we found the frequency of PTSD on screening was very high in samples of patients ascertained through secondary-care services. Although there was substantial heterogeneity in estimates, precluding any useful interpretation of a summary meta-analytic estimate, the IQR across studies ranged from 23 to 40%, indicating that a substantial proportion of patients in secondary-care mental health services met criteria for PTSD in most studies to date.
The frequency of PTSD on screening was high, whereas the frequency with which PTSD was documented in the clinical records was low. Our results indicate that in the majority of cases, mental health clinicians fail to recognise PTSD in their patients. Furthermore, given how common PTSD was on screening, the failure of clinical recognition of this disorder was one that potentially affected a substantial proportion of all patients under the care of specialist mental health services.
Possible explanations
This interpretation of our results depends on a number of key assumptions. First, we are assuming that a diagnosis of PTSD would have been noted in the clinical records had mental health staff identified this as being present. Although it is possible clinicians may have been aware of a PTSD diagnosis but deemed it as irrelevant to the patient's current presentation and not worthy of recording, this seems unlikely. A second, and perhaps more critical assumption, is that the screening tools used to identify PTSD in these studies were valid and did not substantially overestimate the presence of PTSD. A total of 13 studies used self-report questionnaire measures, and all measures used have been validated, with good specificity against the Clinician-Administered PTSD Scale (CAPS) that is considered to be the gold-standard for assessment of PTSD (0.86 for the PTSD checklist (PCL);Reference Blanchard, Jones-Alexander, Buckley and Forneris39 0.93 for the Trauma Screening Questionnaire (TSQ);Reference Brewin, Rose, Andrews, Green, Tata and McEvedy40 0.71 for the PTSD symptom scale – self report version (PSS-SR);Reference Sin, Abdin and Lee41 0.71 for Self-Report Inventory for PTSD (SRIP)Reference Hovens, Bramsen and van der Ploeg42). More relevant, however, is the positive predictive values (PPVs) of these instruments. The PCL, as used by some studies in this review, had a PPV of 0.8 (cut-off score 50) in a sample where 45% of participants had PTSDReference Blanchard, Jones-Alexander, Buckley and Forneris39 and a PPV of 0.7 in another study with a PTSD prevalence of 39%.Reference Harrington and Newman43 Similarly the PPV for the TSQ (6+ items cut-off) was 0.86 in a study with a PTSD prevalence of 34%,Reference Brewin, Rose, Andrews, Green, Tata and McEvedy40 for the SRIP (cut-off 52) was 0.71 with a PTSD prevalence of 47%,Reference Witteveen, Bramsen, Hovens and van der Ploeg44 and for the PSS-SR was 0.64 with a PTSD prevalence of 43%.Reference Coffey, Gudmundsdottir, Beck, Palyo and Miller45
The true proportion of PTSD in these samples if screened with a gold-standard assessment might therefore be slightly lower than that estimated in these studies, although it is unlikely to be substantially lower. Consistent with this, although only 2.1% of the sample in one study had a diagnosis of PTSD in their clinical records,Reference Gielen, Havermans, Tekelenburg and Jansen33 only a further 2.7% had a record of ‘possible PTSD’, making minimal difference to the estimates for undetected PTSD (34.8% compared with 32.2% respectively). Only three studies in our review used the CAPS, however, many studies used other diagnostic interviews that are also likely to be robust measures of PTSD. Furthermore, there was little evidence from the meta-regression that the type of PTSD assessment tool was associated with explaining heterogeneity in the frequency of PTSD on screening.
The third, and final, assumption is that the studies are not biased in a way that leads to substantial overestimates of undetected PTSD. We assessed the quality of these studies, focusing particularly on the strategy for sampling and response rates as being the most likely sources of selection bias. Studies that did not sample all consecutive admissions, or a random sample of patients, may have recruited individuals with an increased likelihood of having experienced a traumatic event, and consequently of having PTSD; for example, patients with a known trauma history may have been selected for recruitment by researchers/clinicians, or may have been more likely to participate. Such scenarios could lead to overestimates in the prevalence of PTSD on screening, and hence undetected PTSD in our review. Most studies were susceptible to such selection bias, and PTSD on screening and undetected PTSD were lower in studies rated with lowest risk of bias. However, there was little evidence from the meta-regression that selection bias risk was associated with heterogeneity in prevalence of undetected PTSD.
Although selection bias might have led to overestimates of PTSD on screening, there are also a number of reasons why prevalence of undetected PTSD may have been underestimated. Absence of masking of researchers to clinical diagnosis when conducting screening interviews, and to screening outcome when retrieving clinical records, introduces the possibility of information bias that would most likely lead to underestimates of undetected PTSD. Furthermore, in two studies underestimates of undetected PTSD may have been particularly likely. One study excluded patients with high scores on the Brief Psychiatric Rating Scale,Reference Alvarez, Roura, Foguet, Oses, Sola and Arrufat37 thus potentially excluding individuals with greater likelihood of PTSD given the association between comorbid PTSD and illness severity. In the other, screening results were entered into the clinical notes,Reference Dansky, Roitzsch, Brady and Saladin22 potentially influencing discharge diagnoses.
Heterogeneity
The strongest characteristic associated with prevalence of PTSD on screening and of undetected PTSD was country, with studies from the USA having substantially higher levels of PTSD than other countries. This is consistent with population-based studies of PTSD that report lifetime prevalence of 8% in the USAReference Kessler, Sonnega, Bromet, Hughes and Nelson46 compared with 1.9% in Europe.Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha and Bryson47 Explanations for differences across countries are almost certainly complex and likely to involve cultural dynamics and historical context, as well as variation in exposure to interpersonal violence and other sources of trauma.Reference Burri and Maercker48, Reference Duckers, Alisic and Brewin49 PTSD was also less likely to be detected in patients with psychotic disorders. One explanation for this is that symptoms of PTSD can be interpreted as psychotic, particularly if severe; for example, re-living experiences, especially during dissociative states, can be classed as hallucinations, and altered beliefs about safety and trust characteristic of severe PTSD can be experienced with delusional intensity.
Strengths and limitations
We had a comprehensive search strategy in terms of the search terms and databases searched to ensure we identified relevant studies, however, we excluded studies that were not published in the English language, and this may have led to some studies being missed. Furthermore, although we took a rigorous approach to address heterogeneity in our results the number of studies in these analyses meant that power may have been limited to identify factors that had smaller effects on frequency of undetected PTSD. Although the degree of heterogeneity precluded us from deriving a meta-analytical estimate for undetected PTSD, nevertheless estimates from 22 of the 29 studies were consistent with at least 10% of patients having undetected PTSD (our a priori definition of clinical importance) as judged by the bounds of the confidence intervals.
Finally, the ability of a systematic review to inform evidence depends upon the quality of the included studies. A number of studies had potential for selection bias, although limiting studies to those with low risk of bias did not alter the conclusions of our findings. Furthermore, although the use of self-report questionnaires as screening instruments may be viewed as an important limitation of many of the included studies in that they might overestimate the frequency of undetected PTSD, there was no evidence that the frequency of undetected PTSD was any lower when restricting our analyses to studies that used only structured interviews for screening.
Implications
If, as suggested by our IQR, 18 to 39% of patients in secondary-care mental health services have undetected PTSD, this has important implications for clinical services. Increased training of mental health staff in identifying symptoms of PTSD, and perhaps particularly in distinguishing re-living experiences from psychotic symptoms, seems warranted.
Presence of comorbid PTSD is associated with poorer clinical outcomes for a number of disorders. More importantly, it is possible that for some patients, the disorder being treated by clinicians (for example depression, agoraphobia, obsessional–compulsive disorder, addictions, psychosis) is secondary to PTSD; failure to recognise and treat the underlying PTSD can lead to failure in recovery from these secondary disorders. This is avoidable, as PTSD is a treatable disorder.5
Concerns about high levels of undetected PTSD have been voiced for approximately two decades,Reference Mueser, Goodman, Trumbetta, Rosenberg, Osher and Vidaver8, Reference Dansky, Roitzsch, Brady and Saladin22, Reference Switzer, Dew, Thompson, Goycoolea, Derricott and Mullins25 yet many healthcare providers do not appear to have taken adequate steps to address this problem, as evidenced by the more recent publications in our review. There is clearly a need for more robust methodology to more accurately determine the extent to which PTSD goes undetected within clinical services, and to determine the likely cost to individuals, service providers and society that might serve as drivers to motivate change. However, even if the true value of undetected PTSD is at the lower limit of the IQR reported here, there is a clear need to trial a PTSD screening programme to examine its feasibility and impact on clinical outcomes. If shown to improve patient outcomes and be cost-effective, such screening programmes should become a standard part of secondary-care mental health services in the future.
Funding
This study was supported by the NIHR Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2017.8









eLetters
No eLetters have been published for this article.