The schizophrenia spectrum of disorders have a peak age at onset from the late teens to mid-twenties. Reference Hafner, Maurer, Loffler, Fatkenheuer, an der Heiden and Riecher-Rossler1 Childhood-onset schizophrenias are considered a rare but a generally more severe form of the condition, Reference Nicolson, Lenane, Hamburger, Fernandez, Bedwell and Rapoport2 potentially providing an opportunity for further understanding aetiology because of a greater loading of causal factors. Reference Childs and Scriver3 Epidemiological data on childhood-onset psychosis are lacking, although evidence from cohort studies suggests that cases tend to have a more insidious onset and higher rates of comorbid developmental disorders Reference Eggers4–Reference Padgett, Miltsiou and Tiffin6 compared with adult-onset illness. The largest such cohort comprised approximately 100 North American individuals. Reference Rapoport, Chavez, Greenstein, Addington and Gogtay7,8 However, it is not clear how representative these were of childhood-onset schizophreniform psychoses more generally, having been recruited via a highly specialist referral centre. The objectives of the present study were to establish the incidence, symptom and treatment profiles, sociodemographic characteristics and short-term course in all cases of childhood-onset schizophrenia-spectrum disorders occurring in the British Isles over a 12-month period.
Method
Individuals under 14 years, presenting from 1 September 2010 to 1 September 2011 with suspected non-affective psychosis were notified by the treating child psychiatrist through the Child and Adolescent Psychiatric Surveillance System (CAPSS), which is operated by the Royal College of Psychiatrists’ Centre for Quality Improvement. Reference Lynn, Viner and Nicholls9 Notifying clinicians completed initial and 1-year follow-up questionnaires. The mean return rate for CAPSS reporting cards during the study was 67%, including ‘nil returns’. To reduce the risk of unreported cases, circular reminder emails were sent to the Royal College of Psychiatrists in Scotland Faculty of Child and Adolescent Psychiatry and the Quality Network for In-Patient CAMHS (QNIC), which ascertained only two additional cases. The case definition 10 was based on the ICD-10 diagnostic criteria for schizophrenia and related disorders. 11
Incidence was calculated as the number of cases reported/total children in that age range (10–14 years) within the population (UK and Republic of Ireland) expressed as cases per 100 000. Population denominator estimates were obtained from the UK Office of National Statistics (ONS) and the Central Statistics Office (Ireland). Indices of urbanicity and multiple deprivation were derived from partial postcodes linked to the relevant ONS data. This study was approved by West London REC 2 and the National Information Governance Board (NIGB) under Section 251.
Results
Figure 1 shows a flow diagram of case reporting. Of 122 reported cases, a total of 28 potential cases, from 16 different clinicians, were unable to be followed up as there were insufficient data obtained to judge eligibility. However, these latter reports were likely to represent misreports rather than true cases (Fig. 1). Thus, our analysis was based on the 8 confirmed cases of early-onset non-affective psychosis, equating to an overall incidence estimate of 0.21/100 000 (95% CI 0.08–0.34). A sensitivity analysis suggested that the range of incidence estimates is from 0.21 to 1/100 000 at-risk population, assuming a minimum of 8 and a maximum of 39 true cases (the latter value includes the 28 cases that were reported with no further information provided and the additional three cases lost to 1-year follow-up). One individual was classified as having schizoaffective disorder, depressive type (incidence 0.026/100 000), one with schizoaffective disorder, mixed type (0.026/100 000), three with paranoid schizophrenia (0.078/100 000), one with unspecified non-organic psychosis (0.026/100 000), one with other acute psychotic disorder (0.026/100 000) and one with undifferentiated schizophrenia (0.026/100 000).
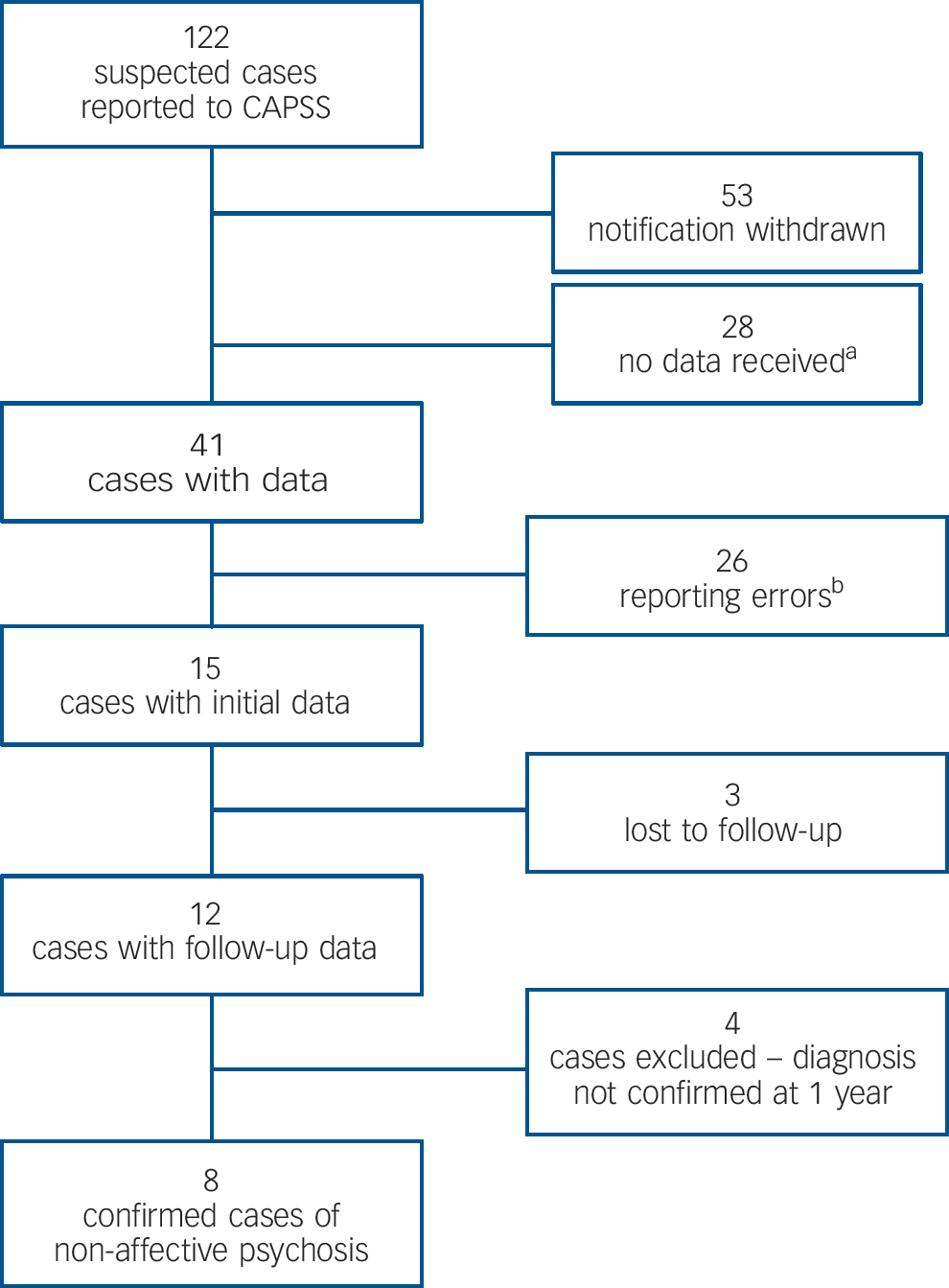
Fig. 1 Flow diagram of case ascertainment.
CAPSS, Child and Adolescent Psychiatric Surveillance System.
a. Twenty-eight cases were reported by 16 clinicians with insufficient information provided to establish caseness.
b. These were mainly excluded on the basis of the young person being above the age of cut-off for the case definition or presenting outside of the surveillance period. One case was excluded because of intellectual disability.
Five individuals were female; six were White, one Black and one Asian. The mean age was 12.98 years (range 11–13 years, s.d. = 1.09). Five had a confirmed or probable family history of psychiatric disorder (schizophrenia in one individual and transient psychosis in another) and in three more than one family member was affected. The median home population density was approximately 8 people per hectare (large British cities have densities usually in excess of 35 people per hectare).
Delusions occurred in all individuals (generally paranoid in content) and hallucinations in seven individuals but also in three individuals with unrelated diagnoses at follow-up. Other symptoms reported were formal thought disorder (n = 6), depressed mood (n = 4), conduct problems/disturbed behaviour (n = 3), elevated/irritable mood (n = 3), negative symptoms (n = 3), catatonia (n = 1) and obsessions/compulsions (n = 1). Five children were perceived as at least of moderate risk of violence according to clinicians’ ratings on a bespoke questionnaire. Three patients were also reported to be at least at moderate risk of self-harm. All but one had comorbidity, most commonly autism spectrum disorder (n = 2 and 1 possible). At baseline four individuals had already had in-patient admissions.
At 1 year only one individual maintained a recovery; the remainder having relapsing or chronic symptoms; the 1-year Clinical Global Improvement (CGI) scale Reference Guy12 classified two individuals very much improved; two much improved; two no change; one much worse, and for one individual there were missing data. Functioning (educational, social and/or practical) outcome was reported as at least poor/moderate (v. good) in six individuals. Five had had at least one in-patient admission (compulsory for two individuals). Only one individual was not prescribed psychiatric medication, and seven had been treated with at least two different medications (one with clozapine).
Discussion
Our findings highlight both the rarity and the general severity of very early-onset schizophrenia. In contrast to previous findings in schizophrenia in early adulthood, there was no suggestion of an excess of males, Black and minority ethnic people or urban dwellers. High rates of admissions to hospital and multiple trials of antipsychotics suggested a degree of complexity and treatment resistance. Our cases were obtained from a national population using an established surveillance system. The main limitation is the very small number of cases confirmed at follow-up and the number of reports with no associated information, curtailing our ability to make inferences. The high rates of ‘false positives’ underline the challenges of accurate diagnosis, but the low number of confirmed cases is also a finding in itself. Delusions and thought disorder were more predictive of ‘true caseness’ than hallucinations, which may be a poor marker of emerging schizophreniform illness in children.
Funding
We are grateful to the Wolfson Research Institute for Health and Wellbeing for funding this work. P.A.T. was supported in his research by a Higher Education Funding Council for England (HEFCE) clinical senior lecturer fellowship.
Acknowledgements
We thank the CAPSS executive committee for facilitating the study and the many consultant child and adolescent psychiatrists who returned the study notification cards. A special thanks to Mr Richard Lynn for his specialised advice to the study team and to Dr Emily Henderson, Ms Catherine Dickie and Dr Joanne-Marie Cairns-Nagi for their help processing the demographic data.




eLetters
No eLetters have been published for this article.